6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff2e1601000000f800000001000400
6go6ckt5b5idvals|120
6go6ckt5b5idcol1|ID
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Introduction
Breastfeeding provides optimal nutritional, immunological, and emotional nurturing for the growth and development of infants. Hypernatremia is a rare complication that may occur in exclusively breastfed babies due to inadequate lactation or high breastmilk sodium. This may cause seizures, intracranial hemorrhage, vascular thrombosis and death.[1] The entity is often missed or inappropriately diagnosed as sepsis due to non-specific presentation and lack of awareness of this entity among health care providers. We describe two neonates with hypernatremic dehydration secondary to lactation failure; they were managed successfully and discharged after appropriate breastfeeding counseling to their mothers.
Case Report
Case 1
A 4 day old male neonate was shifted from the postnatal ward to the neonatal intensive care unit with the mother complaining of excessive irritability and fever. The baby, a product of non-consanguineous parents, was born to a 25 year old primigravida at 39 weeks of gestation by normal vaginal delivery. Antenatal period was uneventful. Apgar Scores were normal. Birth weight was 3000g. He was exclusively breastfed since birth. There was no history of diarrhea or vomiting. The baby was passing urine about 1 to 2 times per day. The mother complained of difficulty in getting the baby to latch and breastfeed properly due to post-partum hemorrhage and had breast engorgement.
At presentation, the baby was moderately dehydrated and febrile, with axillary temperature of 39 °C. Vital signs and neonatal reflexes were normal. Anterior fontanelle was sunken and the abdomen had a doughy feel on palpation. The baby had a weight loss of 10.6 % (320g) since birth. He was icteric till abdomen. Sepsis screen, cerebrospinal fluid examination and arterial blood gas were normal. Serum sodium were elevated (166 mEq/L). Relevant clinical details and investigations are summarized in Table I. Breast milk sodium of the mother was 77mEq/L.
We diagnosed the neonate as having hypernatremic dehydration secondary to lactational failure. He was successfully managed with replacement of fluids by calculation of the free water deficit. This was calculated as follows [2,3]:
Birth weight of the baby= 3000 g
Weight loss at admission = 10.6%= 320g
Fluid deficit= weight loss=320 mL
Since the baby was not in shock, initial fluid bolus of 10–20 mL/kg of Ringer Lactate solution was not required. We started directly with rehydration therapy, aimed at correction of water deficit and sodium excess over 48 hours. The fluid (in the form of 10% dextrose in N/4 saline with 20 mEq/L of potassium) was administered evenly at the rate of 19.2 mL/h for 48 hours as per following calculations:
Maintenance fluid=100 mL/kg/d x 2 d x 3 kg = 600 mL.
Maintenance+ deficit= 600 mL+ 320 mL =920 mL
Rate=920 mL/48 h = 19.2 mL/h
The mother was counselled regarding manual expression of milk and asked to express breast milk every 2 hourly which was quantified daily. Besides, hot fomentations and analgesics were prescribed to relieve breast engorgement. Emphasis was placed on the following topics: manual expression of breast milk, effective counseling to build confidence and give support, explaining why exclusive breastfeeding is important, breastfeeding physiology and positioning /attachment of baby to the breast. She was also prescribed domperidone to increase milk production. Hypernatremia resolved by 48 hours, while the breast milk sodium normalized by the 3rd day (Table II). The baby was off intravenous fluids by the third day. The breastmilk output continued to progressively increase and breastmilk was re-initiated on the third day, with partial formula supplementation. The baby was successfully discharged on day 14 on exclusive breastfeeding after demonstrating weight gain. Blood urea and creatinine normalized at discharge.
Case 2
This female baby presented on day 6 of life with lethargy, fever and jaundice. The baby was born to a 26 year old primigravida at 38 weeks of gestation by normal vaginal delivery. Antenatal and intranatal periods were uneventful. The baby weighed 2000g at birth and was being exclusively breastfed. There was no history of diarrhea or vomiting. The baby had decreased frequency of urine passage.
At presentation baby was dehydrated and lethargic. She was febrile with axillary temperature of 39.5oC and icteric till soles. There was a weight loss of 240 g since birth (12%). Vital signs were normal. Neonatal reflexes were sluggish. Investigations showed a negative sepsis screen and serum sodium of 159mEq/L (Table I). Cerebrospinal fluid examination and arterial blood gas were normal. Management and free water deficit calculations were similar to case I. The baby required phototherapy on which jaundice resolved. Hypernatremia as well as breast milk sodium normalized by the 3rd day (Table II). Thereafter, exclusive breastfeeding was re-initiated and the baby was discharged on day 13 after showing weight gain. Blood urea and creatinine normalized at discharge.
Table I- Clinical details and investigations of the 2 neonates
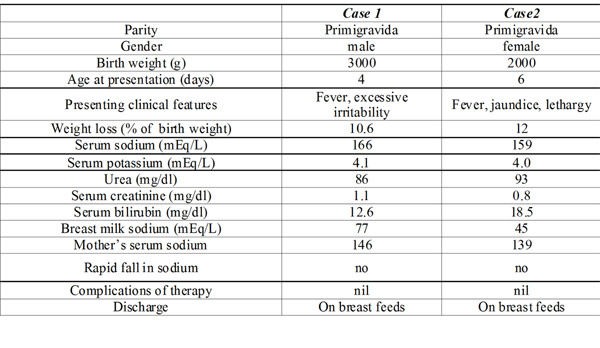
Table II -Clinical course of the neonates
Discussion
Breastfeeding is undoubtedly the best method of feeding infants. Breastfeeding rates are increasing throughout the world. [2,3] Unfortunately, in the last two decades there are increasingly appearing reports of hypernatremic dehydration, a potentially devastating condition in some exclusively breast-fed infants.[4,5,6] There are however, surprisingly fewer reports of this condition from Indian centres.[7,8,9,10] Probably, this is due to decreased awareness regarding this clinical entity as a result of which many such cases tend to be missed or wrongly diagnosed as sepsis due to the common non-specific clinical features associated with both conditions. Through the 2 cases described above, we attempt to increase awareness regarding the condition to facilitate timely diagnosis and management of such cases.
This condition is primarily due to low volume intake of breast milk, as a result of insufficient lactation secondary to ineffective milk removal from the breast. Ineffective milk removal is in turn, primarily associated with poor breast-feeding techniques (i.e., incorrect position and latching). Consequently, the breast becomes engorged, which leads to inadequate prolactin surges and galactopoiesis failure; the baby may tire and fail to stimulate further lactogenesis. The net result is that the neonate becomes dehydrated while the kidneys are mature enough to retain sodium ions. The clinical significance of high breast milk sodium levels in the etiopathogenesis of this clinical entity is unclear. It is probably not the direct cause of neonatal hypernatremia,[4] though high levels of sodium in breast milk are closely associated with lactation failure.[11,12]
In both the cases described by us, the mothers were primigravidae and had difficulty getting their babies to latch and breast-feed properly, and this resulted in insufficient milk removal by the neonate. The second neonate was in addition, small for gestational age. Small for gestational age or preterm infants suckle less powerfully than appropriately grown term infants. Also, in the first case described by us, the mother had postpartum hemorrhage, which may cause temporary pituitary ischemia or disruption and result in hypolactation.[11] Domperidone, a dopamine antagonist that blocks prolactin inhibition and can increase maternal milk synthesis, was prescribed by us in both the cases. The differential diagnosis of sepsis and meningitis were ruled out in both the cases by appropriate investigations. Both the cases also did not have any conditions associated with external fluid loss such as diarrhea which can potentially cause hypernatremic dehydration.
It is unusual to encounter the clinical presentation seen in our cases, which demonstrate that severe dehydration in breast-fed infants may occur as early as the first week of life. In most of the reports published in literature, [4,5,6,7,9,10] the infant with hypernatremic dehydration secondary to breast-feeding has been typically encountered somewhere between the first and third weeks of life. Also, our cases show that following fluid resuscitation, relactation can be achieved in motivated mothers. This is in contrast to observations by some authors wherein babies were discharged on top milk.[7] By ensuring an even rate of fluid administration in the form of 10% dextrose in N/4 saline over a period of 48 hours with periodic sodium level monitoring, we were able to prevent a precipitous fall in serum sodium, [7] which can have neurological complications.
The cases presented by us have implications on policy and practice, especially on the crowded postnatal units of government hospitals in developing countries, as a result of which there is a tendency to discharge babies early without emphasis on monitoring for signs of successful lactation. Prevention of hypernatremic dehydration secondary to lactation failure necessitates the health care provider to be vigilant about dehydration, hypernatremia and hyperbilirubinemia in exclusively breast fed neonates while emphasizing the need to promote exclusive breast feeding. Weighing the infant within the first week after discharge may be cost-effective and provide health care advantages to newborn infants. A weight loss of more than 10% in term infants within the first week of life has been suggested as a warning sign.[13] With a trend towards early postpartum discharge nowadays, community midwives should be trained so that they can monitor carefully the growth and progress of any infants in the community who are small, preterm, or who have been identified as having some feeding difficulties. Special attention must be paid to maternal risk factors for neonatal hypernatremic dehydration such as primigravidity, breast feeding difficulties (improper positioning or attachment), breast engorgement, flat or inverted nipples, and failure of transitional milk to appear by four days; and neonatal risk factors such as infrequent passage of urine (< 6 times a day), delayed passage of yellow seedy stools (after four days), jaundice, lethargy, irritability, fever or multiple pregnancy.[13] Lactation counseling should begin at the hospital and continue even after discharge.
Key messages
-
Hypernatremic dehydration in exclusively breast fed neonates is preventable.
-
Primipara should be given appropriate counseling and support for successful initiation of breastfeeding and maintenance of lactation.
-
The health care provider should be aware of this potentially serious complication of exclusive breastfeeding and recognize neonates at risk for this potentially lethal condition.
References
-
Moritz ML, Manole MD, Bogen DL, Ayus JC. Breastfeeding-associated hypernatremia: are we missing the diagnosis? Pediatrics 2005; 116:e343-347.
-
Ryan AS, Wenjun Z, Acosta A. Breastfeeding continues to increase into the new millennium. Pediatrics 2002; 110:1103- 1109.
-
Tappin DM, Mackenzie JM, Brown AJ, Girdwood RW, Britten J, Broadfoot M, Warren J. Breastfeeding rates are increasing in Scotland. Health Bull (Edinb) 2002; 59:102-13.
-
Sofer S, Ben-Ezer D, Dagan R. Early severe dehydration in young breastfed newborn infants. Isr J Med Sci 1993; 29:85-89.
-
Livingstone VH, Willis CE, Abdel-Wareth LO, Thiessen P, Lockitch G. Neonatal hypernatremic dehydration associated with breast-feeding malnutrition: a retrospective survey. CMAJ 2000; 162:647-652.
-
Kini N, Zahn S, Werlin SL. Hypernatremic dehydration in breast-fed infants. Wis Med J 1995; 94:143–145.
-
Bajpai A, Aggarwal R, Deorari AK, Paul VK. Neonatal hypernatremia due to high breastmilk sodium. Indian Pediatr 2002; 39:193-196.
-
Bhat SR, Lewis P, Dinakar C. Hypernatremic dehydration in a neonate. Indian Pediatr 2001; 38:1174-1177.
-
Scott JX, Raghunath, Gnananayagam JE, Simon A. Neonatal hypernatraemic dehydration and malnutrition associated with inadequate breastfeeding and elevated breastmilk sodium. J Indian Med Assoc 2003; 101:318- 321.
-
Bhat MA, Kawoosa MS, Bhat JI, Ali W. Hypernatremia and intracranial complications due to inadequate exclusive breastfeed in neonates. J Pediatr Neurol 2008; 6:183-187.
-
Humenick SS, Hill PD, Thompson J, Hart AM. Breastmilk sodium as a predictor of breast-feeding patterns. Can J Nurs Res 1998; 30:67– 81.
-
Heldrich FJ, Shaw SS. Case report and review of literature: hypernatremia in breastfed infants. Md Med J 1990; 39:475– 478.
-
Laing IA, Wong CM. Hypernatremia in the first few days: is the incidence rising? Arch Dis Child Fetal Neonatal Ed 2002; 87:F158-62.
Istanbul escort services are an ideal choice for those seeking luxury and privacy in the heart of the city.
Those who want to experience unforgettable moments can explore high-quality and reliable Maslak escort options.
For special and elegant experiences, professional services are offered in the world of Istanbul escort.
Those who value privacy can benefit from exclusive opportunities on the Istanbul escort platform.
Taksim escort services stand out with their central location and reliability.
Besiktas escort seekers are offered special solutions with a warm and friendly approach.
Istanbul escort platforms hold an important place among quality and safe options.
Those who want to meet stylish and distinguished ladies can benefit from Sisli escort services.
There are professional Izmir escort alternatives in harmony with the beauty of the Aegean.
With its elite and disciplined structure, the Istanbul escort sector makes a difference.