6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff248b2c0000006807000001000400
6go6ckt5b5idvals|980
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Introduction
Melanoma is a malignant disease usually arising in the skin but more rarely it can arise from other epithelia such as the paranasal sinuses, other mucosal locations (mucosal melanoma) and ocular locations. The breast can be a site of both primary malignant melanomas arising from the breast parenchyma or from overlying skin or metastatic lesions from other locations [
1]. Primary non-cutaneous breast melanomas without evidence of a skin primary lesion are very rare and only a few cases have been reported in the literature [
2]. It constitutes only less than 5 percent of all melanomas in the body.
Case Report
A 63 year old female presented with complaints of mass in left breast for 6 months duration. It had progressively increased in size and now presented as a fungating mass in left breast. She also gives a history of ulcer over the skin of left breast for 3 months associated with pain and bleeding. General physical and systemic examination was normal. No other skin lesions were made out anywhere else in the body.
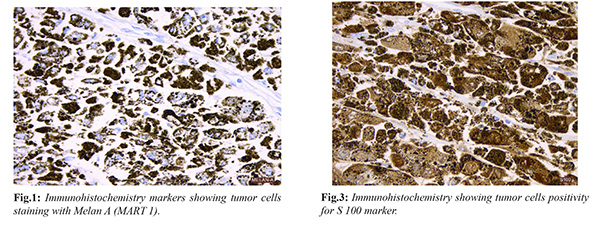
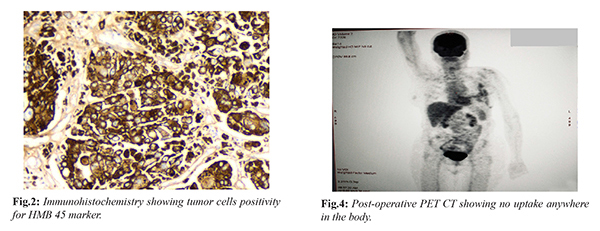
Local examination revealed a fungating mass measuring 5×5 cm in the upper outer quadrant of left breast associated with ulceration and bleeding. A mobile 2×2 cm left axillary node was palpable. Examination of right breast, right axilla and right supraclavicular fossa was normal. Basic blood investigations, chest X-ray and ultrasound abdomen and pelvis failed to reveal any abnormality. Trucut biopsy was attempted but could not be done in view of severe bleeding. She underwent left modified radical mastectomy with axillary node dissection. Histopathological examination microscopically showed a high grade malignant neoplasm composed of interconnected cords and strands of cells with a high degree of pleomorphism, vesicular nuclei and prominent nucleoli. 12 axillary nodes were dissected and all were negative for malignancy. Morphology was suggestive of poorly differentiated malignant neoplasm, high grade. Immunohistochemistry (IHC) was done for further categorization. The tumor cells were strongly positive for Melan-A (MART-1) [Fig.1], HMB45 [Fig.2] and S 100 [Fig.3]. They were negative for vimentin, synaptophysin, CD 31, desmin, CD34 and TLE-1. Based on morphology and IHC it was diagnosed as a case of primary malignant melanoma of left breast. Post-operative period was uneventful. She underwent PET CT [Fig.4] after one month of surgery which did not show uptake anywhere else in the body. Now the patient is on regular follow up.
Discussion
Malignant melanoma is a highly malignant tumor that is derived from melanocytes. It can occur anywhere on the body; however is commonly found in the skin, mucous membranes and the choroid. Malignant melanoma can present in breast and it constitutes about less than 5 percent of all melanomas [
1]. Malignant melanoma of breast can manifest as (i) malignant melanoma of the breast parenchyma only without skin involvement called as primary malignant melanoma of breast (PMMB) or (ii) melanoma of skin overlying the breast (iii) metastatic lesions from other sites and (iv) intransit metastasis. PMMB usually present as mass in the breast similar to our patient. In addition to the mass she also had an ulcer overlying the breast associated with bleeding which is unusual.
Differential diagnosis includes Paget’s disease in the breast nipple and areola complex which may resemble cutaneous melanoma and needs to be differentiated from it as treatment approaches are totally different. Dermal infiltration of an underlying ductal breast carcinoma in the area of the areola without pagetoid epidermal invasion may resemble malignant melanoma clinically. Usually diagnosis is made by history, histological examination and immuno-histochemistry. Pathologically angiosarcoma may resemble melanoma. IHC is needed to differentiate melanoma from the above said malignancies [
3]. In this report patient was diagnosed based on the history, histological examination with IHC correlation. Malignant melanoma is positive for Melan-A, HMB 45 and S 100 markers [
4,
5]. In our case IHC was positive for all the above three tumor markers. Another important factor is that to differentiate metastatic melanoma to the breast from other primaries in skin. A thorough complete skin examination should be performed to exclude the presence of a primary. Our patient did not have any other skin lesions in the body. Primary modality of treatment is surgical resection. Comprehensive axillary dissection is required when pre-operative axillary node metastasis is identified [
6]. In this case patient underwent left modified radical mastectomy along with axillary nodal clearance. Chemotherapy and immunotherapy are used as adjuvant therapy for high risk for recurrence [
7,
8]. Malignant melanoma is considered to be sensitive to immunotherapy. Immunotherapy is indicated in patients with thick melanoma (more than stage II B), node positive disease, recurrent lesions and metastatic disease [
9]. Our patient did not receive any adjuvant treatment.
Molecular analysis for the common melanoma BRAF V600E mutation can be carried out [
10]. PET scan may be helpful in complete staging of the disease. In this report patient also underwent PET CT scan after 1 month of surgery and did not show any other sites of metastasis. She is on regular follow up. Treatment of primary non-cutaneous breast melanoma must be based on the general principles of melanoma treatment as the rarity of the disease precludes any specific recommendations. In the absence of specific data for non-cutaneous breast melanomas, patients with axillary lymphadenopathy should be treated with axillary lymph node dissection in addition to a lumpectomy for removal of the primary tumor as per the guidelines for cutaneous locations. Metastatic disease may be treated with BRAF inhibitors combined with MEK inhibitors if BRAF is mutant, can be treated with IFN-alpha or with monoclonal antibody immunotherapy blocking CTLA4, PD1 or PDL1 [
10].
Conclusion
Primary malignant melanoma of breast is a very rare tumor. Histology alone can be often misleading. Mode of presentation makes it even rarer. IHC is needed for confirmation of diagnosis. Rare tumors like these are needed to be kept in mind before starting any treatment.
Contributors: VVG: manuscript writing, literature review and data acquisition; RB: manuscript editing, and literature review; MN: literature review, and discussion; PAR: critical inputs into the manuscript. MN will act as a study guarantor. All authors approved the final version of this manuscript and are responsible for all aspects of the study.
Funding: None; Competing interests: None stated.
References
- Kurul S, Tas F, Büyükbabani N, Mudun A, Baykal C, Camlica H. Different manifestations of malignant melanoma in the breast: a report of 12 cases and a review of the literature. Jpn J Clin Oncol. 2005;35:202-206.
- Alzaraa A, Sharma N. Primary cutaneous melanoma of the breast: A case report. Cases J. 2008;1:212.
- Ohsie SJ, Sarantopoulos GP, Cochran AJ, Binder SW. Immunohistochemical characteristics of melanoma. J Cutan Pathol. 2008;35:433-444.
- Taatjes DJ, Arendash-Durand B, von Turkovich M, Trainer TD. HMB-45 antibody demonstrates melanosome specificity by immunoelectron microscopy. Arch Pathol Lab Med. 1993;117:264-268.
- Lee AH. Use of immunohistochemistry in the diagnosis of problematic breast lesions. J Clin Pathol. 2013;66:471-477.
- Thompson JF, McCarthy WH, Bosch CM, O’brien CJ, Quinn MJ, Paramaesvaran S, et al. Sentinel lymph node status as an indicator of the presence of metastatic melanoma in regional lymphnodes. Melanoma Res. 1995;5:255-260.
- Davar D, Tarhini AA, Kirkwood JM. Adjuvant therapy for melanoma. Cancer J. 2012;18:192-202.
- Avril MF, Aamdal S, Grob JJ, Hauschild A, Mohr P, Bonerandi JJ, et al. Fotemustine compared with dacarbazine in patients with disseminated malignant melanoma: a phase III study. J Clin Oncol. 2004;22:1118-11125.
- Verma S, Quirt I, McCready D, Bak K, Charette M, Iscie N. Systematic review of systemic adjuvant therapy for patients at high risk for recurrent melanoma. Cancer. 2006;106:1431-1442.
- Chapman PB, Hauschild A, Robert C, Haneen JB, Ascierto P, Larkin J, et al. BRIM-3 Study Group. Improved survival with vemurafenib in melanoma with BRAF V600E mutation. N Engl J Med. 2011;364:2507-2525.