|
|
|
|
|
Collagenous Fibroma in Parotid
|
|
|
|
Mariana Silva Costa, Luísa Frutuoso, Florinda Cardoso, Alexandre Alves, Mário Caetano Nora Department of General Surgery, Centro Hospitalar de Entre o Douro e Vouga, Santa Maria da Feira, Portugal. |
|
|
|
|
|
Corresponding Author:
|
|
Dr. Mariana da Silva Costa Email: mariana87costa@gmail.com |
|
|
|
|
|
|
|
|
Received:
12-OCT-2019 |
Accepted:
18-MAR-2020 |
Published Online:
15-MAY-2020 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
Background: Desmoplastic fibroblastoma (collagenous fibroma) is a rare fibrotic tumor that presents as a firm, slowly growing, painless mass. In order to deepen the understanding of the diagnosis and differential diagnosis of desmoplastic fibroblastoma, we planned to analyze the clinical, radiological, and histopathological features and the outcome of desmoplastic fibroblastoma. Case Report: The authors report a case of a 48-year-old woman with a hard, slightly mobile nodule with imprecise limits in the right mandibular angle, with 9 month evolution. Ultrasound showed a hypoechoic, solid nodule in the superficial portion of the parotid gland. Full parotidectomy was performed by detection of a contiguous nodule at the deep plane, adhering to the buccal branch of the facial nerve. Histology revealed a collagen fibroma. Conclusion: Awareness of this rare lesion arising in atypical location such as the parotid is required, as diagnosis and management can be challenging. |
|
|
|
|
|
Keywords :
|
Collagen, Desmoplastic Fibroma, Facial Nerve, Parotid Gland, Salivary Glands.
|
|
|
|
|
|
|
|
|
|
|
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff2c852d0000006706000001000400 6go6ckt5b5idvals|995 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
Collagenous fibroma (CF) is a rare benign tumor first described by Evans in 1995 that typically presents as a firm, slowly growing and painless mass [ 1]. Nielsen et al. and Hasegawa et al. proposed the name "collagenous fibroma" as being not only more descriptive of its histological composition but also more reflective of its benign prognosis [ 2]. The most common complaint is of a solitary, mobile, painless mass of more than 6 months duration [ 3, 4]. Literature points to a male preference in the fifth and sixth decade of life. Grossly the lesion appears as a well-circumscribed, disc-shaped mass with a firm consistency and a homogeneous fibrous cut surface [ 3]. In 2013, the WHO described the microscopic appearance of desmoplastic fibroma as being composed of slender, spindle to stellate cells with minimal cytological atypia and abundant collagenous matrix [ 5]. The differential diagnosis is for CF includes a wide variety of soft tissue lesions, especially solitary fibrous tumor (SFT) and, most importantly, desmoid fibromatosis (DFM). This report documents a rare parotid lesion which may mimic other more common parotid gland neoplasms.
Case Report
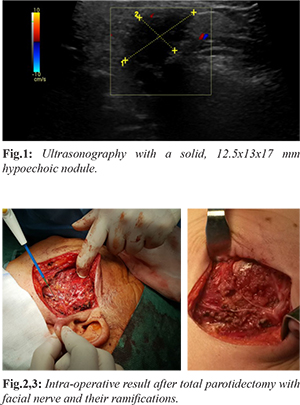
We report a 48-year-old woman presenting with a nodule localized at the right mandibular angle with a 9-month duration. On examination, a hard nodule of about 2 cm, slightly mobile and with imprecise limits was palpable. There were no history of trauma, infection or weight loss. There were no macroscopic changes of the overlying skin, no regional lymphadenopathy and the patient had normal facial nerve function. Ultrasonography showed a solid, 12.5×13×17 mm, poorly delimited, high-attenuating, hypoechoic nodule located at the superficial portion of the gland in close relation to the retro-mandibular vein. No vascularization was identified in the power doppler evaluation. No enlarged lymph nodes in the ganglion chains of the supra-hyoid neck were noted [Fig.1]. The patient was submitted to two core biopsy that were insufficient for diagnosis and surgical excision was performed under general anaesthesia. Total parotidectomy was performed because intra-operatively a lesion contiguous to the deep plane and adherent to the buccal branch of the facial nerve was noted [Fig.2,3].
Histology revealed an expansive, well-limited, unencapsulated, compact, whitish, hard tissue with a 19 mm major axis that contacted the peripheral surgical plane. The remaining fragments correspond to the glandular structure without evidence of lesions. In immunohistochemistry, the lesion was focally positive for smooth muscle actin, strongly positive for vimentin and negative for B-catenin, CD10 and protein S100. Histological examination of the various fragments and immunohistochemical result favoured the diagnosis of collagenous fibroma of the parotid gland. Post-operative paralysis of the facial nerve was effectively treated with physical therapy. With four year follow up, the patient is free of disease.
Discussion
Soft tissue tumors are highly heterogeneous group of mesenchymal neoplasm grouped into benign, intermediate (locally aggressive), intermediate (rarely metastasizing) and malignant [ 6]. In 1995 Evans coined the term desmoplastic fibroblastoma. Since then, an additional eleven cases have been reported by Nielsen et al. and Hasegawa et al. who favor the name collagenous fibroma [ 2, 3, 7- 10]. According to the World Health Organization (WHO) classification of tumors of soft tissue and bone (2013), desmoplastic fibroblastoma is "a rare, benign, paucicellular tumor, characterized by densely collagenous, predominantly stellate-shaped fibroblast. Myxoid stroma may be present [ 10, 11]. Mitotic activity is rare and necrosis has not been identified. Long bones are commonly involved especially the distal femur and proximal tíbia. They have also been described in the neck, tongue, lacrimal gland and palate [ 4, 11]. The tumor cells are positive for vimentin and there was often focal reactivity for muscle actins (HHF-35) and alpha-smooth muscle actin [ 4]. The differential diagnosis includes a wide variety of soft tissue lesions, neurofibroma, fibromatosis nodular fasciitis, fibroma of the tendo sheath, solitary, perineuroma, nuchal fibroma, sclerotic fibroma of the skin, calcifying fibrous pseudotumor, low grow fibromyxoid stroma and myxoma. SFT could be excluded on the basis of the lack of hyper-cellular areas, including hemangiopericytoma like foci. Immunohistochemical staining for CD34 helps in distinguishing SFT and CF too, as the present tumor was completely CD34 negative [ 4]. Beta-catenin staining is also helpful for discriminating DFM from CF and SFT with positive nuclear reactivity for B-catenin being observed in DFM [ 4]. In this case, the tumor was focally positive for smooth muscle actin, strongly positive for vimentin and negative for B-catenin, CD10 and protein S100. Histopathologically, nodular fasciitis is generally more cellular and has greater vascularity. Also, it typically has prominent myofibroblastic differentiation with rather strong and diffuse immunoreactivity for muscle actins. Late stages of nodular fasciitis may contain areas reminiscent of those seen in collagenous fibroma, but the former more frequently exhibits cystic degeneration and often contains scattered osteoclast-like giant cells [ 4]. CF is considered to be a neoplasm because of its association with the 11q12 break points, a lack of inciting events and the initiation of reactive fibrous proliferation. This idea is also supported by the fact that a flow cytometry analysis has demonstrated diploid DNA consistent with a low S-phase fraction [ 10]. No CF is known to metastasize. A resection of the whole tumor is regarded as an adequate treatment [ 10, 12, 13]. The ability to distinguish a CF from other tumors correctly is critical for choosing the proper therapy [ 10]. As desmoplastic fibroma histologically resembles soft tissue fibromatosis, it has been speculated that radiotherapy may be effective in achieving local control. Effectiveness of radiotherapy in soft tissue fibromatosis is well documented. There have been two case reports describing treatment of desmoplastic fibroma with radiotherapy as the primary modality, in ilium and distal femur [ 5]. They concluded that radiotherapy may be an acceptable alternative therapy especially when enbloc resection has the potential to result in significant functional impairment [ 5].
Conclusion
We highlight this peculiar lesion and wish to increase awareness of these rare lesions amongst surgeons and pathologists alike, especially when it arises in atypical locations such as the parotid in which the panoply of differential diagnose can give the case more complexity.
Contributors: Mariana Costa was responsible for the writing the manuscript and the conception of the work; Luisa Frutuoso, Florinda Cardoso, Alexandre and Mário Nora were responsible for revising it critically. Mariana Costa will act as a study guarantor. All authors approved the final version of this manuscript and are responsible for all aspects of this study. Funding: None; Competing interests: None stated.
References - Nishio J, Akiho S, Iwasaki H, Naito M. Translocation t (2;11) is characteristic of collagenous fibroma (desmoplastic fibroblastoma). Cancer Genetics. 2011;204:569-571.
- Varghese T, Pillai KS, Sarojini SB, Khosla E. Desmoplastic fibroblastoma (collagenous fibroma) in the oral cavity. J Indian Soc Pedod Prev Dent. 2014;32:238-241.
- Ide F, Shimoyama T, Horie N, Tanaka H. Collagenous fibroma (desmoplastic fibroblastoma) presenting as a parotidmass. J Oral Pathol Med. 1999;28:465-468.
- Nagaraja V, Coleman H, Morgan J. Desmoplastic fibroblastoma presenting as a parotid tumour. A case report and review of the literature. Head and Neck Pathol. 2013;7:285-290.
- Tanwar Y, Kharbanda Y, Rastogi R, Singh R. Desmoplastic fibroma of bone. A case series and review of literature. Indian Journal of Surgical Oncology. 2018;9(4):585-591.
- Nishio J. Updates on the cytogenetics and molecular cytogenetics of benign and intermediate soft tissue tumors (Review). Oncology Letters. 2013;5:12-18.
- Evans HL. Desmoplastic fibroblastoma. A report of seven cases. Am J Surg. Pathol. 1995;19:1077-1081.
- Nielsen P, O'Connell JX, Dickersin JR, Rosenberg AE. Collagenous fibroma (desmoplastic fibroblastoma) a report of seven cases. Mod Pathol. 1996;9:781-785.
- Hasegawa T, Shimoda T, Hirohashi S, Hizawa K, Sano T. Collagenous fibroma (desmoplastic fibroblastoma) report of four cases and review of the literature. Arch Pathol Lab Med. 1998;122(5):455-460.
- Watanabe H, Ishida Y, Nagashima K, Makino T, Norisugi O, Shimizu T. Desmoplastic fibroblastoma (collagenous fibroma). Journal of Dermatology. 2008;35:93-97.
- Gong L, Liu W, Ding Y, Geng Y, Sun X, Huang X. Diagnosis and differential diagnosis of desmoplastic fibroblastoma by clinical, radiological, and histopathological analyses. Chin Med J. 2018;131:32-36.
- Coelho H, Meira J, Martins V, Campos J, Coelho A, Augusto R, et al. Fibroblastom adesmoplásico envolvendo a artéria braquial — um caso clínico único. Angiologia e Cirurgia Vascular. 2017;13(4).
- Dagli M, Eryilmaz A, Acar A, Kulacoglu S, Akmansu H. Collagenous (Desmoplastic fibroblastoma). Yonsei Medical Journal. 2004;45(5):941-943.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
Costa MS, Frutuoso L, Cardoso F, Alves A, Nora MCCollagenous Fibroma in Parotid.JCR 2020;10:99-102 |
|
Costa MS, Frutuoso L, Cardoso F, Alves A, Nora MCCollagenous Fibroma in Parotid.JCR [serial online] 2020[cited 2025 Dec 13];10:99-102. Available from: http://www.casereports.in/articles/10/2/Collagenous-Fibroma-in-Parotid.html |

|
|
|
|
|