6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff2873300000007206000001000c00
6go6ckt5b5idvals|2030
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Introduction
A soil dwelling, dimorphic pathogenic fungi, Histoplasma capsulatum is endemic in North and South America, Indonesia and Malaysia [
1]. In India, Gangetic delta bed region of West Bengal and Assam form the endemic region [
2]. Infants, elderly and immunocompromised individuals present with acute and chronic pulmonary and disseminated forms [
3]. Extra-pulmonary form of histoplasmosis, in form of skin, oral or visceral involvement, almost exclusively occurs in disseminated form of pulmonary histoplasmosis in immunocompromised patients [
4]. Localized oral histoplasmosis is a rare presentation in immunocompetent individuals [
5-
7]. Here, we present a case of known smoker and tobacco chewer, who presented in our surgical oncology clinic with non-healing oral ulcer.
Case Report
This 52 year male, known diabetic and smoker for 30 years, presented with chief complaints of non-healing ulcer since 10 months over left cheek and right upper alveolus following tooth extraction. Clinical examination revealed a 2.5×3 cm ulcero-infiltrative lesion over the left buccal mucosa extending approximately 1 cm from left commissure to around 2 cm anterior to the left anterior tonsillar fossa and not involving upper or lower gingiva-buccal sulcus. Another 3×3 cm ulcero-proliferative lesion was seen at hard palate on right side involving left upper alveolus. No cervical lymph node was palpable [Fig.1a,b]. The margins of the ulcer were everted, with characteristic surrounding induration. A clinical diagnosis of invasive carcinoma of oral cavity was made.

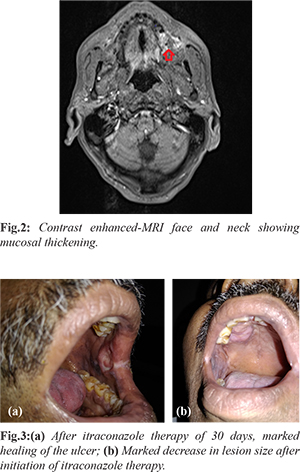
Further evaluation was done with tissue biopsy and imaging. CECT chest revealed no abnormalities except for few insignificant subcentimeric fibronodularities. MRI face and neck revealed 1.7×1.1 cm lesion in left buccal mucosa which appeared heterogeneous hyperintense on T2W1 and STIR and hypointense on T1W1 with heterogeneous enhancement [Fig.2]. Punch biopsy from both the ulcers were taken. Biopsy suggested mature stratified squamous with no dysplasia. Numerous multinucleated giant cells with intracellular encapsulated forms of fungus confirming in morphology to Histoplasma and the yeast form was positive for periodic acid-Schiff stain. In view of absence of systemic or pulmonary symptoms or immunosuppression, a diagnosis of localized mucocutaneous oral histoplasmosis was made. Individual was treated with oral itraconazole 200 mg. Patient showed steady clinical and symptomatic improvement with serial pictures depicting steady response and resolution of the signs and symptoms after around 30 days of therapy [Fig.3a,b]. The individual was continued on itraconazole for almost nine more months.
Discussion
Samuel Darling first described disseminated histoplasmosis in a patient who was suspected to have died of milliary tuberculosis in 1905 [
8]. Primary site of infection for histoplasmosis is the lungs [
9]. Air borne microsporidia are commonly responsible for the spread of this disease and form yeast cells which replicate in the reticuloendothelial cells resulting in granuloma formation in which T cell mediated immune response eventually clears up the infection [
10]. However, in immunocompromised individuals, this infection can spread to multiple organs including oral cavity, lymph nodes, liver or spleen leading to disseminated histoplasmosis [
11].
Localized extra-pulmonary histoplasmosis is extremely rare. Various presentations which have been reported are pyrexia of unknown origin, acute adrenal deficiencies, central nervous system lesions or ulcerated oral lesions [
6]. Only a few case reports of localized oral histoplasmosis are available and a generalized consensus for treatment of oral localized histoplasmosis has not been established. Many investigators are of the opinion that oral lesions are in fact initial manifestation of the systemic dissemination occurring in immunocompromised individuals and so prefer treating even localized oral mucocutaneous lesion with systemic antifungals (amphotericin B) and oral azoles [
6,
11]. However, few authors have recommended to treat localized oral histoplasmosis in immunocompetent patients as a localized disease only and treat with oral azoles, as was done in this case, showing improved clinical results and avoiding the strong and often irreversible side effects of amphotericin B [
12,
13]. Oral histoplasmosis presents and very closely mimics invasive oral carcinoma and thus reinforcing the role of tissue diagnosis in every case of invasive carcinoma before jumping to radical treatment.
Conclusion
Localized oral mucocutaneous histoplasmosis is a definite entity in the immunocompetent patient which masquerades as invasive carcinoma. Tissue diagnosis gives a definite diagnosis and oral azoles are effective as a treatment option for such lesion.
Contributors: AA: manuscript writing, literature review, and patient management; VKA: manuscript editing, references and patient management. VKA will act as a study guarantor. Both authors approved the final version of this manuscript and are responsible for all aspects of the study.
Funding: None; Competing interests: None stated.
References
- Antinori S. Histoplasma capsulatum: more widespread than previously thought. The Am J Trop Med Hyg. 2014;90:982.
- De D, Nath UK. Disseminated histoplasmosis in immunocompetent individuals-not a so rare entity, in India. Mediterranean Journal of Hematology and Infectious Diseases. 2015;7(1):e2015028.
- Rubin H, Furcolow ML, Yates JL, Brasher CA. The course and prognosis of histoplasmosis. Am J Med. 1959;27:278-288.
- Alva E, Vásquez J, Frisancho O, Yoza M, Yábar A. Colonic histoplasmosis as a diagnostic manifestation of AIDS. Revista de gastroenterologia del Peru: organo oficial de la Sociedad de Gastroenterologia del Peru. 2010;30:163-166.
- Alcure ML, Júnior ODH, de Almeida OP, Bonilha H, Lopes MA. Oral histoplasmosis in an HIV-negative patient. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics. 2006;101:e33-e36.
- Iqbal F, Schifter M, Coleman H. Oral presentation of histoplasmosis in an immunocompetent patient: a diagnostic challenge. Australian Dental Journal. 2014;59:386-388.
- Mignogna M, Fedele S, Russo LL, Ruoppo E, Muzio LL. A case of oral localized histoplasmosis in an immunocompetent patient. European Journal of Clinical Microbiology and Infectious Diseases. 2001;20:753.
- Hagan T. The discovery and naming of Histoplasmosis: Samuel Taylor Darling. JAMA. 1905;1907.
- Rippon JW. Medical mycology; the pathogenic fungi and the pathogenic actinomycetes: Eastbourne, UK; WB Saunders Company; 1982.
- Edwards JA, Rappleye CA. Histoplasma mechanisms of pathogenesis–one portfolio doesn't fit all. FEMS Microbiology Letters. 2011;324:1-9.
- Vidyanath S, Shameena P, Sudha S, Nair RG. Disseminated histoplasmosis with oral and cutaneous manifestations. Journal of Oral and Maxillofacial Pathology. 2013;17:139.
- Fortuna G, Mignogna M. Oral histoplasmosis of a healthy man in a non-endemic area. Infection. 2011;39:497.
- John M, Koshy JM, Mohan S, Paul P. Histoplasmosis presenting as a laryngeal ulcer in an immunocompetent host. Journal of The Association of Physicians of India. 2015;63:69-71.