|
|
|
|
|
Symptomatic Residual Gallbladder: A Rare Condition Associated to Subtotal Cholecystectomy: A Report of Two Cases
|
|
|
|
Rafaela Capelli1,2,5, Klaus Steinbrück3,5, Luiza Basilio2,5, Marcelo D’Oliveira2,5, Renato Cano2,5, Hanna Vasconcelos2,5, Reinaldo Fernandes3,4,5, Marcelo Enne2,5 1Department of Surgical Gastroenterology, Federal University of São Paulo, São Paulo, Brazil; 2Hepatobiliary Surgery Unit, Ipanema Federal Hospital, Rio de Janeiro, Brazil; 3Hepatobiliary Surgery Unit, Bonsucesso Federal Hospital, Rio de Janeiro, Brazil; 4Department of General Surgery, Fluminense Federal University, Brazil; 5Hepatobiliary Multidisciplinary Group, Rio de Janeiro, Brazil. |
|
|
|
|
|
Corresponding Author:
|
|
Dr Klaus Steinbrück Email: steinbruck@gmail.com |
|
|
|
|
|
|
|
|
Received:
21-MAY-2021 |
Accepted:
24-NOV-2021 |
Published Online:
30-DEC-2021 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
Background: Residual gallbladder is the remnant part of the gallbladder not resected during subtotal cholecystectomy. This technique is used mostly in cholecystitis cases, to avoid biliary injury. In some patients, the residual gallbladder may become symptomatic causing symptoms related to gallstone problems, such as symptomatic cholelithiasis, choledocholithiasis and gallstone pancreatitis. Case Report: Herein, we describe the two patients, a 52-year-old man and a 67-year-old woman, respectively submitted to cholecystectomy 16 months and 24 years before, who presented mainly abdominal pain after eating. Abdominal ultrasonography identified the remnant gallbladder in the first case. Second patient was wrongly treated for gastritis for one year, until residual gallbladder was confirmed by magnetic resonance cholangio-pancreatography. Patients underwent surgical treatment, with good results. Conclusion: Symptomatic residual gallbladder should be suspected in patients previously submitted to cholecystectomy, presenting symptoms suggestive of biliary colic. Symptoms may arise many years after the index surgery. Since this is a rare condition, a high grade of suspicion is required and imaging exams are important to confirm diagnosis. Caution is necessary during surgery, due to adhesions to the hepatic pedicle and common bile duct injury risk. |
|
|
|
|
|
Keywords :
|
Cholecystectomy, Gallbladder, Magnetic Resonance Cholangio-pancreatography, Post-Cholecystectomy Syndrome.
|
|
|
|
|
|
|
|
|
|
|
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ffe42f36000000300a000001000100 6go6ckt5b5idvals|3103 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
Cholecystectomy is the treatment of choice for symptomatic gallbladder disease. However, in few cases, the complete resection of the gallbladder is not achieved and a subtotal cholecystectomy (STC) is then performed, leaving behind a residual gallbladder (RGB). Although an infrequent event, previous studies have shown that the rates of STC have risen in the last years, either for open or laparoscopic surgery, especially in the presence of inflammation of the gallbladder [ 1, 2]. In some patients, the RGB may become symptomatic, with recurrence of symptoms presented before index surgery, such as abdominal pain, nausea, vomiting, fever, diarrhea, and jaundice, often related to the presence of residual gallstones [ 3- 5]. The time to develop symptoms, since the index cholecystectomy, can vary from days to more than forty years [ 3- 5]. This being a rare condition, patients are frequently submitted to multiple diagnostic and therapeutic procedures, before the diagnosis is made [ 4, 5]. The treatment of choice is the surgical resection of the gallbladder remnant with good results [ 3- 6]. Herein, we present two cases of symptomatic RGB after STC, effectively treated by surgery, and perform a literature review.
Case Reports
Case 1
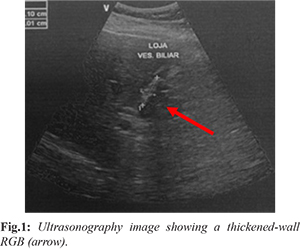
A 52-year-old man was admitted to our unit complaining of upper-right abdominal pain, vomiting and abdominal distention, mostly present after eating. Sixteen months earlier, he had undergone an open cholecystectomy due to severe cholecystitis. Except for pain in the epigastric region and right subcostal scar from the cholecystectomy, he had no abnormalities during physical examination. Laboratory tests showed mild elevated inflammatory markers (C-reactive protein: 7 mg/dL, erythrocyte sedimentation rate: 29 mm/1st hour, white blood cells 11,000/µL). Abdominal ultrasonography (USG) revealed an image of a thickened wall small gallbladder [Fig.1]. As the cholecystectomy was performed at another institution, we couldn’t get any information about his previous surgery, so we supposed that a STC was executed and a RGB was responsible for the symptoms. After one month, he underwent a new laparotomy, through the same right subcostal incision, and RGB was identified and resected with tiny gallstones inside. The patient was discharged on the 3rd post-operative day. He was followed up for 6 months, with no symptoms’ return.
Case 2
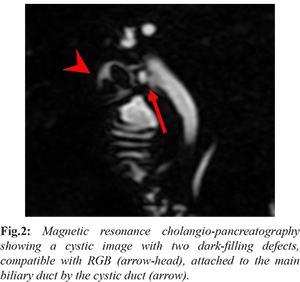
A 67-year-old woman was admitted to the gastroenterology department referring a one-year history of upper abdominal pain and nausea after eating. During this period, she was evaluated in a basic health unit, where she underwent endoscopy, which showed mild gastritis, and treatment with a proton pump inhibitor was started. No improvement in symptoms was observed. She was then evaluated with abdominal USG, that identified a cystic cavity with concrements close to the liver hilum, suggestive of cholecystolithiasis. As she had undergone open cholecystectomy 24 years earlier, the possibility of RGB was raised and the patient was referred to our hospital. Patient declared no co-morbidities and physical examination revealed an abdominal right paramedian scar. Laboratorial tests were normal. We proceeded with the investigation and a magnetic resonance cholangio-pancreatography (MRCP) was performed, identifying a 2.8 cm cystic image, in the topography of the gallbladder, with two dark-filling defects within it, indicative of biliary stones [Fig.2], confirming the suspicion of RGB. Patient was taken to surgery and, despite the presence of adhesions and local fibrosis, surgery was carried out by laparoscopy with complete resection of the RGB [Fig.3]. The patient was discharged one day after surgery and remained symptom-free seven months after surgery.

Discussion
Subtotal cholecystectomy refers to the partial resection of the gallbladder, either intentionally, to prevent biliary injury, or involuntarily, because of imprecise identification of the anatomy [ 7, 8]. The subtotal cholecystectomy technique was first described by Madding in 1955 [ 9], but was only 30 years later, after the series report by Bornman and Terblanche [ 10], that its use was expanded, as a replacement for total cholecystectomy in cases of difficult dissection, due to acute inflammation and/or fibrosis [ 7, 8]. Even though the rates of STC increased in the last years, it is still a rare event, with an incidence of 0.4%, according to a review performed by Sabour et al., of 290,855 patients submitted to surgery due to acute cholecystitis [ 1]. RGB is the remnant part of the gallbladder not resected during STC. In some patients, the RGB may become symptomatic, often in the setting of gallstone-related problems, such as acute cholecystitis, symptomatic cholelithiasis, choledocholithiasis, gallstone pancreatitis, and/or cholangitis [ 3- 5, 11]. Preview studies demonstrated that the presence of calculi within the RGB or common bile duct (CBD) is almost constant in symptomatic patients, with rates higher than 96% [ 3- 5, 11]. The most frequent manifestation reported is abdominal pain, similar to biliary colic, present in 69-100% of patients, followed by nausea, vomiting, fever, and diarrhea [ 3- 5, 11]. Less frequently, signs of CBD obstruction are present, like jaundice, cholangitis, biliary pancreatitis, acholic stools, and dark urine [ 3- 5, 11]. In the largest series of symptomatic RGB published so far, Singh et al. reported four interesting cases of cholecysto-cutaneous fistula as consequence of inflammation of the RGB [ 3]. The time between the index STC and the beginning of symptoms can vary a lot, ranging from a few days to 41 years [ 3- 5]. In the cases reported here, patients presented abdominal pain as the main symptom, which is in conformity with literature. Complaints started sixteen months and twenty-four years after first surgery, respectively for patient 1 and 2, which corroborates the variation in time to onset of symptoms. As the main manifestations of a symptomatic RGB are non-specific and can start over a wide variation of time, patients are normally submitted to many diagnostic modalities to evaluate them. Grossman et al. reported that an average of three (range 1-8) diagnostic tests were performed on patients in the process of diagnosing a symptomatic RGB [ 4]. Singh et al. described that abdominal USG is the preferable initial investigation exam if RGB is suspected, as it is helpful to diagnose RGB and calculi within it, in up to 97.8% and 89% of cases, respectively [ 3]. However, these results could not be observed in other studies [ 4, 5]. Computed tomography (CT) scan appears to have even worse accuracy rates to identify RGB, with sensitivity around 70% [ 3- 5]. When other methods fail to promote diagnosis, MRCP is the exam of choice, with sensitivity of 90-100% [ 3- 5]. Additional diagnostic studies reported in the investigation of symptoms related to RGB included endoscopic retrograde cholangiopancreatography (ERCP), hepatobiliary imino-diacetic acid, endoscopic ultrasound, esophagogastroduodenoscopy, gastric emptying studies, and esophageal manometry [ 4]. In the cases described here, the first patient diagnosis was carried out by USG, soon after onset of symptoms. On the other hand, the second patient was submitted to three exams and was wrongly treated for gastritis, during almost a one-year period, until RGB with calculi was confirmed by MRCP. We believe that the long time between cholecystectomy and start of symptoms, 24 years, was a confounding factor that delayed the correct diagnosis. After RGB is diagnosed, treatment is eminently surgical, by complete resection of the remnant part of the gallbladder, via laparotomy or laparoscopy [ 3- 5, 11]. Although there are reports of RGB/CBD stones management with ERCP/extracorporeal shockwave lithotripsy [ 4, 12], these treatment modalities do not treat the cause of the pathology, i.e. the RGB. Surgical treatment is associated with excellent outcomes, with a high rate of complete resolution of symptoms (98-100%) [3-6], as we could observe with our patients. Laparoscopy approach can be difficult, due to fibrosis and adhesions to the RGB and hepatic pedicle, and conversion rates in these cases can be as high as 40% [ 3]. We faced this difficulty in our second case, but laparoscopic resection of the RGB could be accomplished. The reoperation to resect the RGB demands experienced surgeons to manage the hepatic pedicle and avoid injury, specially to the biliary tract, which can be involved by great fibrosis and inflammatory process.
Conclusion
Patients submitted to STC may develop symptoms associated with the RGB, especially when residual gallstones are present. MRCP is the preferable exam to confirm the diagnosis. Surgery is the treatment of choice to remove the RGB, with good results, but the operation can be difficult and demands expert surgeons.
Contributors: RCapelli, KS, LB, MD’O, RCano, HV, RF, and ME participated in the surgical procedures, designed the case report, collected data, wrote the paper, and critically reviewed the paper. KS will act as a study guarantor. All authors approved the final version of this manuscript and are responsible for all aspects of this study. Funding: None; Competing interests: None stated.
References - Sabour AF, Matsushima K, Love BE, Alicuben ET, Schellenberg MA, Inaba K, et al. Nationwide trends in the use of subtotal cholecystectomy for acute cholecystitis. Surgery. 2020;167:569-574.
- Tay WM, Toh YJ, Shelat VG, Huey CW, Junnarkar SP, Woon W, et al. Subtotal cholecystectomy: early and long term outcomes. Surg Endosc. 2020;34:4536-4542.
- Singh A, Kapoor A, Singh RK, Prakash A, Behari A, Kumar A, et al. Management of residual gall bladder: A 15-year experience from a north Indian tertiary care centre. Ann Hepatobiliary-Pancreatic Surg. 2018;22:36-41.
- Grossman JG, Johnston WR, Fowler KJ, Williams GA, Hammill CW, Hawkins WG. A diagnosis reconsidered: the symptomatic gallbladder remnant. J Hepatobiliary Pancreat Sci. 2019;26:137-143.
- Palanivelu C, Rangarajan M, Jategaonkar PA, Madankumar MV, Anand NV. Laparoscopic management of remnant cystic duct calculi: A retrospective study. Ann R Coll Surg Engl. 2009;91:25-29.
- Xu A, Hu H, Zhao G, Jiao L. How to successfully manage residual gallbladders laparoscopically following open techniques? Surg Laparosc Endosc Percutan Tech. 2017;27:e92-e95.
- Philips JAE, Lawes DA, Cook AJ, Arulampalam TH, Zaborsky A, Menzies D, et al. The use of laparoscopic subtotal cholecystectomy for complicated cholelithiasis. Surg Endosc. 2008;22:1697-1700.
- Walsh RM, Chung RS, Grundfest-Broniatowski S. Incomplete excision of the gallbladder during laparoscopic cholecystectomy. Surg Endosc. 1995;9:67-70.
- Madding GF. Subtotal cholecystectomy in acute cholecystitis. Am J Surg. 1955;89:604-607.
- Bornman PC, Terblanche J. Subtotal cholecystectomy: for the difficult gallbladder in portal hypertension and cholecystitis. Surgery. 1985;98:1-6.
- Vyas F, Nayak S, Perakath B, Pradhan N. Gallbladder remnant and cystic duct stump calculus as a cause of postcholecystectomy syndrome. Trop Gastroenterol. 2005;26:159-160.
- Walsh RM, Ponsky JL, Dumot J. Retained gallbladder/cystic duct remnant calculi as a cause of postcholecystectomy pain. Surg Endosc. 2002;16:981-984.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
Capelli R, Steinbrück K, Basilio L, D’Oliveira M, Cano R, Vasconcelos H, Fernandes R, Enne MSymptomatic Residual Gallbladder: A Rare Condition Associated to Subtotal Cholecystectomy: A Report of Two Cases.JCR 2021;11:235-238 |
|
Capelli R, Steinbrück K, Basilio L, D’Oliveira M, Cano R, Vasconcelos H, Fernandes R, Enne MSymptomatic Residual Gallbladder: A Rare Condition Associated to Subtotal Cholecystectomy: A Report of Two Cases.JCR [serial online] 2021[cited 2025 Dec 23];11:235-238. Available from: http://www.casereports.in/articles/11/4/Symptomatic-Residual-Gallbladder.html |

|
|
|
|
|