6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff64e5370000006207000001000300
6go6ckt5b5idvals|3122
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Introduction
Acute pulmonary embolism is a component of venous thromboembolism (VTE), which may prove fatal if not suspected and subsequently treated [1]. The incidence of pulmonary embolism (PE) is reported to be around 3-9% of COVID-19 in hospitalized patients [2] and up to one-third of those requiring intensive care unit (ICU) admission [3], despite standard prophylactic anticoagulation. Cases have been reported around the world as delayed presentation of pulmonary embolism during recovery from COVID. In patients suffering from multiple myeloma, incidence of PE has been reported to be 3% [4]. A high clinical suspicion remains the key for early diagnosis. We report a case of multiple myeloma who presented as acute massive PE in post-covid recovery phase, despite being on therapeutic anticoagulation.
Case Report
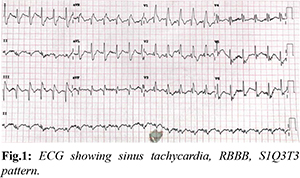
A 49-year-old male, an African national, presented to our Emergency Department (ED) with complaints of sudden onset breathlessness for 30 minutes, associated with chest tightness. On arrival, he was tachypneic with a rate of 28 breaths/min and oxygen saturation of 72% on room air, which improved to 93% on 4 liters oxygen. His blood pressure was 90/60 mmHg, heart rate of 134/min, core body temperature of 98.2° F, and random blood sugar of 85 mg/dL. Chest auscultation revealed decreased air entry over left bases with occasional crepitations. Initial 12 lead ECG showed sinus tachycardia, new onset right bundle branch block (RBBB) with deep S waves in lead I, Q waves and inverted T waves in lead III [Fig.1]. Arterial blood gas analysis showed hypoxemia with high lactate levels: pH-7.402, pCO2-35.9 mmHg, pO2-65.2 mmHg, K-3.8 mmol/L, Na-134 mmol/L, lactate-8.6 mmol/L, HCO3-22.3 mmol/L.
He had past history of multiple myeloma and received bortezomib, cyclophosphamide and dexamethasone (VCD protocol) as chemotherapy three years ago. Subsequently, he underwent an autologous bone marrow transplant. Five months ago, he suffered from COVID-19 pneumonia and had good recovery. Two weeks before presentation to emergency department, he was diagnosed to have deep venous thrombosis of left popliteal vein for which he was prescribed injection enoxaparin 80 mg twice daily as therapeutic anticoagulation. He reported full compliance to the prescription.
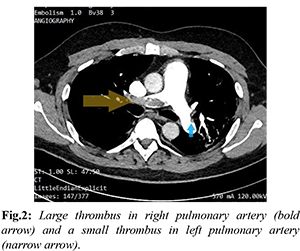
Baseline hematological and biochemical profile, including cardiac enzymes returned normal reports. Covid IgG antibodies were highly reactive (level of 44.9 AU/mL). His chest -x-ray was normal and echocardiography showed no right atrium or right ventricle dilatation, pulmonary artery pressure 32 mmHg. In view of high suspicion of pulmonary thromboembolism, CTPA (CT-pulmonary angiography) was done which revealed massive thrombus in distal right pulmonary artery extending to segmental and subsegmental branches and some thrombus in left pulmonary artery [Fig.2]. Lung parenchyma showed ground glass opacities (post covid changes) bilaterally with atelectasis, predominantly in lower lobes.
Considering the potential high risk with presence of persistent hypotension - a decision of thrombolysis was made by PERT (pulmonary embolism response team). Intravenous thrombolysis with recombinant tissue plasminogen activator (Alteplase) 100 mg over 2 hours was started in emergency department. Later anticoagulation was maintained with heparin infusion at 1200 IU/hr with supportive care. Patient was shifted to coronary care unit for further monitoring and subsequent care. He showed marked improvement over a period of two days with normalization of pulse rate, respiratory rate and saturation on room air. ECG returned to normal sinus rhythm. He was started on oral anticoagulant rivaroxaban 15 mg twice daily as a switch over from heparin during his stay in hospital. At the time of decision of discharge patient’s simplified PESI (Pulmonary Embolism Severity Index) score was 0. He was discharged on oral rivaroxaban after five days of hospitalization.
Discussion
Venous thromboembolism has been reported to be a major finding in post-COVID patients prompting use of prophylactic anticoagulation. Hypercoagulability and decreased fibrinolytic capacity due to multiple myeloma are the probable causes of multiple thrombosis [5]. Thrombotic events have been observed in COVID-19 patients who were not admitted to hospital but data on incidence is limited. Alban Gervaise et al. evaluated 72 outpatients with COVID-19 pneumonia after recovery that presented to ED and were referred for CTPA. PE was identified in 13 (18%) cases [6]. There is evidence of direct invasion of endothelial cells by coronavirus, potentially leading to cell injury. This may be compounded by direct and indirect pathologic consequences of COVID-19 complement activation, microvascular inflammation, endothelial exocytosis, endotheliitis, cytokine release and endothelial dysfunction which plays central role in coagulation in COVID-19 [7,8]. Risk of early recurrence of pulmonary embolism during anticoagulation therapy is not well established and poorly studied [9,10].
This patient presented with sudden onset shortness of breath, associated with chest heaviness. His CTPA showed a large thrombus in right pulmonary artery, following which he was thrombolyzed with recombinant tissue plasminogen activator, and discharged on oral anticoagulants. He had a significant past history of multiple myeloma, COVID-19 pneumonia 5 months ago, and was recently diagnosed with deep vein thrombosis and was started on anticoagulants. Despite reporting compliance with medications, and adequate dosing based on weight, patient developed massive pulmonary embolism requiring intravenous thrombolysis. Our patient is one of those rare cases whose anticoagulant failure wasn’t attributable to inadequate dosing, rather was a combination of being in a hypercoagulable state, due to his history of multiple myeloma and Covid-19 pneumonia. His large stature (weight 102.5 kg, BMI-30.01) and different ethnicity may have played a role in its development.
The post Covid-19 pneumonia complications occurring due to mild/moderate/severe illness need to be further studied and documented in detail. Pulmonary embolism remains a disease which requires high clinical suspicion, supported by validated scores and confirmed with further multi-modality investigations. Unlike infectious diseases, cardiac disorder or blood disorder, no specific symptoms, signs or investigations reflect a disease process immediately. Emergency physicians should be careful of post covid patients, with one or more risk factors, who presents with acute onset of dyspnea, despite being on anticoagulants. They should be evaluated for common causes of dyspnea but pulmonary embolism be kept in mind, so as not to miss this fatal disease.
Conclusion
Pulmonary embolism occurring despite anticoagulation is termed as anticoagulation failure. A hypercoagulable state due to prior COVID-19 pneumonia and multiple myeloma, could be a factor in anticoagulation failure. Frequent and adequate monitoring is required in patients who are initiated on anticoagulation.
Contributors: NB: manuscript writing, patient management; SJ, AP: manuscript editing, patient management; MM: critical inputs into the manuscript. NB will act as a study guarantor. All authors approved the final version of this manuscript and are responsible for all aspects of this study.
Funding: None; Competing interests: None stated.
References
- Lax SF, Skok K, Zechner P, Kessler HH, Kaufmann N, Koelblinger C, et al. Pulmonary arterial thrombosis in COVID-19 with fatal outcome: results from a prospective, single-center, clinicopathologic case series. Ann Intern Med. 2020;173:350-361.
- Helms J, Tacquard C, Severac F, Leonard-Lorant I, Ohana M, Delabranche X, et al. High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study. Intensive Care Med. 2020;46:1089-1098.
- Klok FA, Kruip M, van der Meer NJM, Arbous MS, Gommers D, Kant KM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145-147.
- Kapadia SB. Multiple myeloma: a clinicopathologic study of 62 consecutively autopsied cases. Medicine (Baltimore). 1980;59:380-392.
- Zangari M, Saghafifar F, Mehta P, Barlogie B, Fink L, Tricot G. The blood coagulation mechanism in multiple myeloma. Semin Thromb Hemost. 2003;29(3):275-282.
- Gervaise A, Bouzad C, Peroux E, Helissey C. Acute pulmonary embolism in non-hospitalized COVID-19 patients referred to CTPA by emergency department. Eur Radiol. 2020;30(11):6170-6177.
- Teuwen LA, Geldhof V, Pasut A, Peter Carmeliet P. COVID-19: the vasculature unleashed. Nat Rev Immunol. 2020;20(7):389-391.
- Libby P, Lüscher T. COVID-19 is, in the end, an endothelial disease. Eur Heart J. 2020;41(32):3038-3044.
- Cui S, Chen S, Li X, Liu S, Wang F. Prevalence of venous thromboembolism in patients with severe novel coronavirus pneumonia. J Thromb Haemost. 2020;18:1421-1424.
- Pannucci CJ, Fleming KI, Holoyda K, Moulton L, Prazak AM, Varghese TK Jr. Enoxaparin 40 mg per day is inadequate for venous thromboembolism prophylaxis after thoracic surgical procedure. Ann Thorac Surg. 2018;106(2):404-411.