6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ffe423380000005d06000001000900
6go6ckt5b5idvals|3125
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Introduction
Fibroids represent the most common benign pelvic tumor and are mainly uterine in origin. Rarely, ectopic locations of fibroid have been reported in the literature like ovaries, urethra, bladder, peritoneum and vulva [
1]. Vaginal leiomyoma is a very rare benign tumor with only few cases being reported so far. The first case was reported by Denys De Leyden in 1773 [
2]. Its variable appearances and presentations lead to a diagnostic challenge which is sought only after histological confirmation.
Case Report
A 40-year-old female, parity 4 living 4, reported to the casualty with complaints of frequent menses since 3 years and urinary retention for 2 days. On further probing, she gave history of a prolapsing mass 5 years back. She reposited the mass back inside once after which it never came out. The patient was relieved of urinary retention after Foleys catheterization.
On examination, she was obese with BMI 31.2 kg/m2 and vitally stable. On per abdominal examination, the abdomen was pendulous, soft and non-tender with no lump palpable. On local examination, a bulge of around 8×6 cm was present over left sided labia majora. On per speculum examination, the vagina was entirely filled by a mass whose origin could not be defined. However, the cervix could not be visualised. On per vaginal examination, a mass of around 10×6 cm arising from the left lateral vaginal wall was felt. The upper margin was well demarcated with base being 1 cm from the introitus. It was smooth surfaced, firm in consistency, slightly mobile, non-tender and occupying left as well as posterior fornices. The cervix was felt with difficulty which was firm in consistency and displaced towards the right side. The uterus and bilateral adnexa were normal. The rectal mucosa was free but same mass was felt on per rectal examination. All the blood investigations were normal. On trans-abdominopelvic ultrasonography, heterogenous hypoechoic mass of 12.6×6.2 cm filling the vagina and abutting the posterior wall of urinary bladder was seen. However, no invasion into the bladder was noted. Uterus was normal in size with endometrial thickness of 9 mm and rest of the organs were normal [Fig.1].
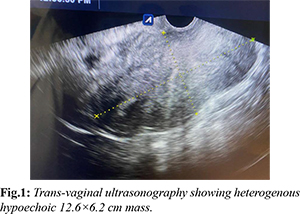
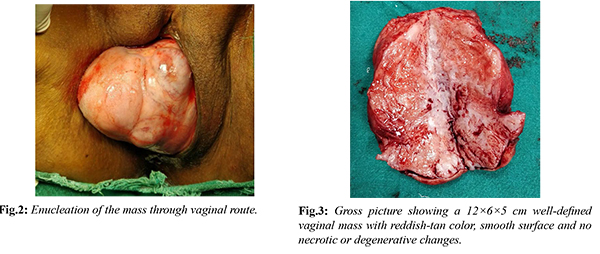
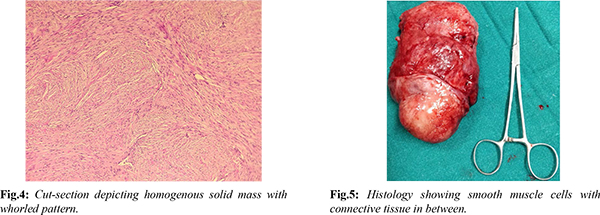
The differential diagnosis after this scenario were myofibroblastoma, angiomyofibroblastoma, angiomyxoma, liposarcoma or vaginal malignancy. Decision for surgical excision was taken for symptomatic relief and to rule out malignancy. Enucleation of the vaginal mass was done through vaginal route under regional anaesthesia and sent for histopathological examination [Fig.2]. Gross examination revealed a 12×6×5 cm well-defined, reddish-tan and smooth surface solid mass with no degenerative or necrotic changes in it [Fig.3]. Cut-section depicted grey-white homogenous solid mass with whorled pattern [Fig.4]. Microscopically, well-circumscribed mass was composed of intersecting and interlacing fascicles of smooth muscle fibres arranged in whorled pattern [Fig.5]. These findings were consistent with the diagnosis of vaginal leiomyoma. Post-operative period was uneventful and patient was discharged on post-operative day 3. During 6 months of follow-up following surgery, patient has been asymptomatic throughout and her menstrual cycles were regular and normal.
Discussion
Leiomyoma being one of the most common tumors of female genital tract, occurs mainly in the uterus. However, several extra-uterine locations have also been reported with vagina being the rarest [
3]. Vaginal leiomyoma is more common in women belonging to third- and fourth-decade age group. It is more prevalent in Caucasian women as compared to non-Caucasian groups in contrast to uterine leiomyoma which are more common in blacks [
3].
Usually, the tumor arises from the anterior vaginal wall followed by the posterior vaginal wall and least commonly from the lateral vaginal wall. Their size varies from 0.5 to 15 cm in diameter, thus having varied presentations [
4]. The present case reported vaginal leiomyoma arising from the left lateral vaginal, thereby decreasing the likelihood of clinical suspicion. Therefore, it was misinterpreted as myofibroblastoma, angiofibroma or liposarcoma. Smaller vaginal leiomyomas are usually asymptomatic but larger ones can present as lower abdominal pain, vaginal bleeding, low backache, protrusion of mass from vagina, frequency of micturition, dyspareunia, dysuria, or other features of urinary obstruction [
5]. In the present case, patient experienced urinary retention and abdominal pain. Consistency of vaginal leiomyoma can vary depending upon the amount of degeneration just like uterine fibroids. They can be hard to soft, thus giving a challenge in diagnosis [
6]. These vaginal leiomyomas are usually single, benign, well-circumscribed and slow-growing. However, some studies have reported sarcomatous changes in them [
6].
The pre-operative diagnosis is difficult with simple imaging modality like ultrasonography. But magnetic resonance imaging can prove to be definitive in diagnosis. Vaginal leiomyomas appear as well-defined solid masses with low signal intensity with homogenous contrast enhancement on T1- and T2-weighted images in magnetic resonance imaging. However, the gold standard remains histopathology for the diagnosis [
7]. The treatment of choice for vaginal leiomyoma is surgical excision and enucleation as it confirms the diagnosis and also rules out the possibility of malignancy. It can be done either through vaginal or abdominal-perineal route depending upon the size of the mass [
7]. Three patients showed recurrence within 2 years in a case series presented by Zhao’s et al., thus encouraging the need of long-term follow-up for patients with vaginal leiomyoma [
8].
Conclusion
Vaginal leiomyoma is a rare entity. Its location on lateral vaginal wall is even rarer. Emphasis should be made on including it amongst the differential diagnosis of vaginal masses. Preoperatively, medical therapies like gonadotrophin releasing hormones agonists could be given to decrease the size and blood loss in some selected cases. Thus, an awareness of this uncommon entity is crucial for early detection and appropriate management.
Contributors: MG, AC: manuscript writing, patient management; RM, BG: manuscript editing, patient management; AS: critical inputs into the manuscript. AC will act as a study guarantor. All authors approved the final version of this manuscript and are responsible for all aspects of this study.
Funding: None; Competing interests: None stated.
References
- Ammouri S. Vulvar leiomyoma: a case report. Pan Afr Med J. 2019;32:208.
- Patil RR. An unusual presentation of vaginal leiomyoma. J Midlife Health. 2019;10(4):204-205.
- Wu Y, Wang W, Sheng X, Kong L, Qi J. A misdiagnosed vaginal leiomyoma: Case Report. Urol. Case Rep. 2015;3(3):82-83.
- Egbe TO. Vaginal leiomyoma: medical imaging and diagnosis in a resource low tertiary hospital: case report. BMC Womens Health. 2020;20(1):12.
- Koranne P, Raut D, Wahane A, Uike P. A rare case of anterior vaginal wall leiomyoma. J Obstet Gynaecol India. 2014;65(2):129-131.
- Goel A. Bhavana N, Prashanth R, Sanjaya V. Vaginal leiomyoma - A common tumour at an uncommon location. Eurorad. 2020;16621.
- Wethmar E, Mouton AD, Dreyer G. Vaginal leiomyoma presenting as a lateral vaginal wall mass. South Afr J Gynaecol Onco. 2017;9(1):16-18.
- Zhao T, Liu X, Lu Y. Myxoid epithelial leiomyoma of the vulva: A case report and literature review. Case Rep Obstet Gynecol. 2015;894830.