|
|
|
|
|
Managing a Gastrocolocutaneous Fistula with Delayed Presentation after PEG Placement without Surgery
|
|
|
|
Kaveh Najafi1, Helen Markowski1, DJ Green1, Frank Bauer1, Bruce Davis1, Karen Lewandowski RN2, Shashvat M Desai2, John P Kepros1
1Department of Trauma, Acute Care Surgery and Surgical Critical Care, HonorHealth Scottsdale Osborn, Scottsdale, AZ; 2Honor Health Research Institute, Honor Health Scottsdale Osborn, Scottsdale, AZ. |
|
|
|
|
|
Corresponding Author:
|
|
Dr Kaveh Najafi
Email: knajafi@honorhealth.com |
|
|
|
|
|
|
|
|
Received:
14-APR-2022 |
Accepted:
18-JAN-2023 |
Published Online:
25-JAN-2023 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
Background: This case report describes the successful non-surgical management of a gastrocolocutaneous fistula that developed following percutaneous endoscopic gastrostomy (PEG) placement. Case Report: The patient presented several months after the procedure with abdominal pain and discharge from the PEG site. Imaging revealed a fistula between the stomach and colon, which was managed conservatively with PEG site care, bowel rest, and antibiotics. The patient's symptoms gradually improved over several weeks, and follow-up imaging showed resolution of the fistula. Conclusion: This case demonstrates that non-operative management can be a viable option for select patients with delayed gastrocolocutaneous fistulas after PEG placement. |
|
|
|
|
|
Keywords :
|
Abdominal Pain, Endoscope, Gastrostomy, Postoperative Complication, Ventilator.
|
|
|
|
|
|
|
|
|
|
|
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ffe41d390000009906000001000700
Introduction
Percutaneous endoscopic gastrostomy, PEG, is a common procedure and solution for those patients with inadequate oral intake. In fact, studies have shown that a PEG is an efficient and safe method for gastrostomy tube placement with a lower complication rate than a surgical gastrostomy [1]. During the procedure, a physician who is trained to perform endoscopic procedures inserts the endoscope and inflates the stomach. The light source should be visible through the skin and delineating the area for insertion of the tube, usually 2 cm medial to the costal margin and 2 cm inferior to the xiphoid process. Endoscopic transillumination of the abdominal wall and one-to-one finger indentation are essential steps in identifying the precise location for PEG insertion. When both techniques are used, they offer the highest likelihood of achieving favorable anatomy and proper placement. However, as with any surgical procedure, complications can occur. One very rare complication is insertion of the PEG through the colon into the stomach. Signs of this complication may present acutely after placement with fever, loose or watery bowel movements, pneumoperitoneum, peritonitis, or signs of obstruction. If identified early and the patient is symptomatic, surgical intervention is indicated [2]. Although rare, the complication may not be identified until late in the patient’s course. This is a case report of non-surgical management in a patient with a malpositioned PEG that resulted in a gastrocolocutaneous fistula that was managed non-operatively.
Case Report
The patient is a 71-year male with a past medical history that included sick sinus syndrome that required a pacemaker, congestive heart failure, end stage liver disease, cirrhosis and pulmonary hypertension presented to the emergency department (ED) for a small bowel obstruction. He ultimately needed surgical intervention and underwent a diagnostic laparoscopy converted to open laparotomy with lysis of adhesions. Post-operatively, the patient remained ventilator dependent and was transferred to the intensive care unit (ICU). After approximately 1 week in the ICU, patient remained ventilator dependent and critically ill. Therefore, the family decided to pursue a tracheostomy and PEG placement. Both procedures were uneventful. During the PEG, there was good transillumination, good single digit indentation, placed 2 finger-breadths below the costal margin and was secured at 3.5 cm at the skin. The patient was transferred out of the ICU and was doing well. Approximately 4 days later, the patient was noted to be mildly distended and a CT scan of the abdomen and pelvis with intravenous (IV) and rectal contrast was completed and showed a mild amount of free air and free fluid in addition to a mild ileus. It appeared as though the bumper was not flush against the abdominal wall. The PEG was noted to be at 5 cm, and we concluded that this was the reason that free air was noted on imaging [3]. To be thorough we also conducted a PEG study which showed a patent gastrostomy tube with no evidence of leak.
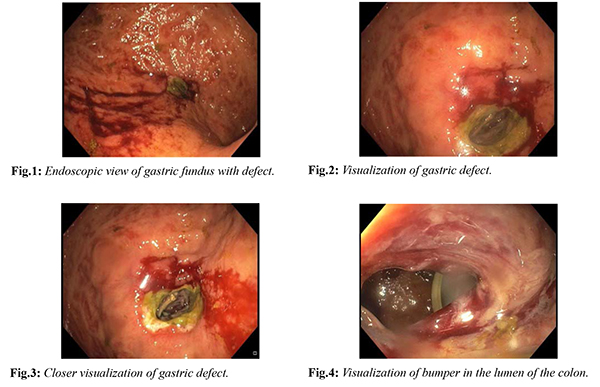
The following week the patient is noted to have an episode of hypotension and is transferred back to the ICU. Clinically, he improved with fluid resuscitation but it is noted that he is not tolerating tube feeds. In fact, when put to suction, 500 cc were removed. A gastro-intestinal (GI) consult was placed for a repeat esophagogastroduodenoscopy (EGD) and placement of a gastrostomy-jejunostomy (GJ) tube, with the thought that the patient has developed delayed gastric emptying and thus the reason for inability to tolerate tube feeds [Fig.1-4]. During the upper endoscopy, there was a deformity noted in the gastric body proximally causing obstruction. The deformity could not be positively identified which raised concern for a possible malignancy versus a gastric ulcer. Repeat imaging with oral contrast via the PEG now showed the gastrostomy tube in the transverse colon, however the free air has resolved, and the fluid in the abdomen is consistent with simple ascites. At this point, the patient has been hospitalized for approximately 1 month, on a ventilator and is severely decompensated with end stage liver disease and hepatorenal syndrome. We felt that at this time, he would not likely survive a major surgical procedure. Because he was not septic or peritonitic, the decision was made to leave the PEG in place for a total of 4 weeks from its date of insertion and then to be removed it bedside. After the PEG was removed successfully, a colostomy bag was placed over the fistula site for the management of drainage of the liquid stool. Over the following week, the output slowly started to decrease. An upper GI small bowel series with contrast via the naso-gastric (NGT) was performed and no definite evidence of a gastro-colic fistula was seen. The patient resumed tube feeds via a Dobhoff tube and was eventually transferred to a long-term ventilator care facility.
Discussion
The “pull” technique, also known as the Ponsky technique, is currently considered to be the most common technique utilized to insert the PEG tube. In this method, a large bore needle is passed from the anterior abdominal wall into the stomach, a looped wire is then inserted through the needle, grasped with endoscopic biopsy forceps and then taken out through the esophagus and mouth. Subsequently the wire is fixed to the external end of the feeding tube and the tube is pulled from the mouth to the esophagus, stomach and then out though the abdominal wall. Endoscopic visualization after placement is common to assure proper placement of the bumper. Complications are minimized with the general guidance of the following practices. Prior to PEG placement, it is important to visualize the patient's abdomen for any relevant surgical scars or hernias, review the pertinent past medical and surgical history, and any also any relevant imaging to optimize the location of the feeding tube insertion site. The patient is positioned supine with the head of the bed raised to 30 degrees to prevent aspiration and to displace the colon inferiorly due to gravity. The patients are usually sedated and provided local anesthetic. A physician who is trained to perform endoscopic procedures inserts the scope and inflates the stomach. The light source should be visible through the skin and delineating the area for insertion of the tube, usually 2 cm medial to the costal margin and 2 cm inferior to the xiphoid process. Endoscopic trans-illumination on the abdominal wall and one to one finger indentation are vital steps in identifying the precise location for PEG insertion and when both identified, presents the highest likelihood of favorable anatomy and proper placement. Once the PEG is in place it should be secured to the anterior abdominal wall using a skin disc to hold the tube in good position at the level of 3-4 cm.
Despite the above, complications are still possible. One such complication is insertion of the PEG through the colon into the stomach. This occurs if the colon, usually the transverse colon, is caught between the stomach and the anterior abdominal wall while inserting the finder needle. Gastrocolocutaneous fistulas can develop in this type of PEG malposition. A gastrocolic fistula should be considered in any patient with a PEG who develops diarrhea after placement of the gastrostomy tube. Severe diarrhea may develop secondary to the osmotic load of the formula entering the colon or may appear as actual tube feeds. Gastrocolocutaneous fistulas may not be identified right away. Some remain asymptomatic while others may develop pneumoperitoneum, sepsis, peritonitis or signs of obstruction. If the patient is symptomatic with signs of sepsis or peritonitis then removal of the PEG and surgical repair of both the stomach and the colon may be indicated. Other studies also suggest that these injuries may also be repaired or clipped endoscopically [4,5,7]. In our experience, the presence of free air and signs of bowel obstruction were very concerning for malpositioning of the gastrostomy, however, all imaging modalities were negative for any findings that suggested this feared complication. With the assistance of an EGD and direct visualization, we were finally able to identify the gastrocolocutaneous fistula, 3 weeks after its initial placement of the PEG.
A literature review suggests that this type of complication is rare and has an incidence rate of 0.5-3%. In some cases, these fistulas may not be identified until the tube requires replacement [10]. Data from previous reports are insufficient to propose standard management for these fistulas. Because of the fact that our patient was decompensated, unlikely to survive an exploratory laparotomy, and was also free of any signs of peritonitis, we opted for conservative management the fistula. We presumed that after 4 weeks the tracts between the stomach, transverse colon and skin were mature and this is why we decided to remove the PEG at that time. Following its removal, the fistulas appeared to heal and close on their own. Although surgical intervention is usually required for such complications, when the complication is identified late and the patient is decompensated, conservative management with TPN and removal of the PEG at 4 weeks is a viable option of management.
Conclusion
Feeding gastrostomy tubes can be placed through multiple different methods, including percutaneous endoscopic gastrostomy, laparoscopic assisted, radiologically guided, or open surgical placement. While percutaneous endoscopic gastrostomy (PEG) placement is the most widely used and accepted approach, it is not free of complication and risk. We propose that if a patient remains asymptomatic with an identified colocutaneous fistula, consider removing the PEG after approximately 4 weeks and allow the fistula to heal conservatively.
Hot best Top Replica Watches UK for men and women are available on this web.
Cheap and quality, noob factory Swiss Replica Watches ca with best movements are suited for men and women.
Contributors: KN, HM: Manuscript writing, and patient management; DJG, FB, BD, KPK: manuscript revision, and patient management; KLRN, SMD: clinical input and revision of the manuscript. KN will act as a study guarantor. All authors approved the final version of this manuscript and are responsible for all aspects of this study.
Funding: None; Competing interests: None stated.
References
- Ljungdahl M, Sundbom M. Complication rate lower after percutaneous endoscopic gastrostomy than after surgical gastrostomy: a prospective, randomized trial. Surg Endosc. 2006;20(8):1248-1251.
- Boeykens K, Duysburgh I. Prevention and management of major complications in percutaneous endoscopic gastrostomy. BMJ Open Gastroenterology. 2021;8(1):e00628.
- Güvenç BH, Rasa K, Güvenç S The presence of percutaneous endoscopic gastrostomy (PEG)-related postprocedural pneumoperitoneum. Endoscopy. 2009;41:E269-270.
- von Delius S, Huber W, Dienemann T, Gaa J, Frandah M, Schmid RM, et al. Endoscopic treatment of transcolonic misplacement of a percutaneous endoscopic gastrostomy tube. Endoscopy. 2010;422:E50-51.
- Chime C, Baiomi A, Kumar K, Patel H, Dev A, Makker J. Endoscopic repair of gastrocolic and colocutaneous fistulas complicating percutaneous endoscopic gastrostomy tube. Case Rep Gastrointest Med. 2020;2020:7262514.
- Emmett DS, Polter DE. Colocutaneous fistula after a PEG. Gastrointestinal Endoscopy. 2008;68:770.
- Cmorej P, Mayuiers M, Sugawa C. Management of early PEG tube dislodgement: simultaneous endoscopic closure of gastric wall defect and PEG replacement. BMJ Case Rep. 2019;12(9):e230728.
- Linhares M, Pereira F, Azevedo R, Sousa R, Banhudo A. Late closure by secondary intention of a large gastrocutaneous fistula after complicated percutaneous endoscopic gastrostomy. Gastroenterol Hepatol. 2020;43(1):32-33.
- Triantafyllou K, Papanikolaou IS, Stasinos I, Polymeros D, Dimitriadis GD. Percutaneous endoscopic gastrostomy tube replacement unexpected serious events. Nutr Clin Pract. 2014;29(1):142-145.
- Lee J, Kim J, Jung HY. Gastrocolocutaneous fistula: An unusual case of gastrostomy tube malfunction with diarrhea. Clinical Endoscopy. 2018;51(2):196-200.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
Najafi K, Markowski H, Green DJ, Bauer F, Davis B, Lewandowski RN K, Desai SM, Kepros JPManaging a Gastrocolocutaneous Fistula with Delayed Presentation after PEG Placement without Surgery.JCR 2023;13:7-10 |
|
Najafi K, Markowski H, Green DJ, Bauer F, Davis B, Lewandowski RN K, Desai SM, Kepros JPManaging a Gastrocolocutaneous Fistula with Delayed Presentation after PEG Placement without Surgery.JCR [serial online] 2023[cited 2026 Feb 16];13:7-10. Available from: http://www.casereports.in/articles/13/1/Managing-a-Gastrocolocutaneous-Fistula-with-Delayed-Presentation-after-PEG-Placement-without-Surgery.html |

|
|
|
|
|