|
|
|
|
|
Neurogenic Pulmonary Edema : A Rare Presentation of Traumatic Brain Injury
|
|
|
|
Kushagra Gupta, Ankur Verma, Sanjay Jaiswal, Wasil Rasool Sheikh, Meghna Haldar, Amit Vishen, Rinkey Ahuja, Abbas Ali Khatai Department of Emergency Medicine, Max Super Speciality Hospital, Patparganj, New Delhi. |
|
|
|
|
|
Corresponding Author:
|
|
Dr. Kushagra Gupta Email: kushagrag.9@gmail.com |
|
|
|
|
|
|
|
|
Received:
10-OCT-2022 |
Accepted:
07-FEB-2023 |
Published Online:
05-APR-2023 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
Background: The pathology behind traumatic brain injury (TBI) ranges from shifts in cellular ionic concentrations to permanent structural damage. TBI patients may develop neurogenic pulmonary edema subsequently but it is a poorly understood entity and is often misdiagnosed. Case Report: We present a case of a young female who presented in altered sensorium with a traumatic brain injury. Shortly after arrival she developed respiratory distress and shock. She was diagnosed as having a neurogenic pulmonary edema and succumbed to her injuries the following day. Conclusion: Neurogenic pulmonary edema is a fatal complication of higher grades of traumatic brain injury. Timely recognition of the symptoms along with appropriate intervention may help improve the outcomes in an otherwise bleak prognosis. |
|
|
|
|
|
Keywords :
|
Altered Sensorium, Respiratory Distress, Shock, Prognosis, Trauma.
|
|
|
|
|
|
|
|
|
|
|
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff64d9390000005907000001000200 Introduction
Neurogenic pulmonary edema (NPE), first described in a patient with status epilepticus in 1908, was also later seen in 1928 with a head trauma patient [ 1]. This condition continues to be poorly understood and sometimes misdiagnosed; its actual incidence is unknown because most of the literature relies on single case reports and necropsy results of lower number of patients with no statistical relevance. However, the clinical presentation of NPE is thought to range from subclinical to fulminant pulmonary edema. Meningeal haemorrhage is thought to be one of the most common causes of neurogenic pulmonary edema [ 2]. We present a case of a 23-year-old female who presented with traumatic brain injury (TBI) and within hours developed neurogenic pulmonary edema.
Case Report
A 23-year-old female with no known co-morbidities, presented to the emergency department (ED), with severe TBI post a road traffic accident. On primary survey she had a heart rate of 62/minute, blood pressure of 100/60 mm Hg, respiratory rate of 20/minute, oxygen saturation on room air 98% and random blood sugar of 95 mg/dL and was in altered mental status. Secondary survey revealed a sutured lacerated wound over the right temporo-parietal region and clotted blood was seen at the external auditory meatus of the right ear. She had a Glasgow coma score of 10/15. Immediate cervical spine stabilization and fluid resuscitation were initiated. The head end of the bed was raised in view of suspected raised ICP. Computed Tomography (CT) of the brain revealed small haemorrhagic contusions in bilateral frontal and temporal region along with minimal sub-arachnoid haemorrhage (SAH) noted in bilateral sylvian fissures with thin subdural collection in the right temporal region [Fig.1,2]. Initial chest x ray showed no parenchymal changes with clear bilateral lung fields.
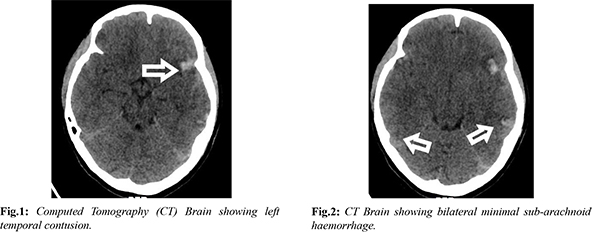
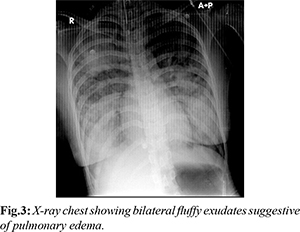
The patient was advised admission under the neurosurgical team for conservative management in the Intensive care unit (ICU). Before patient could be shifted, she suddenly became tachypnoeic and hypoxic with a respiratory rate of 35/minute and saturation on room air recorded at 70%. Her blood pressure dropped to 80/40 mm Hg. She became drowsy and her GCS deteriorated to 8/15 (E2M4V2). Immediate blood gas revealed a type 1 respiratory failure with PaO2 of 50 mmHg, pH: 7.29, lactate: 3.1 and base deficit of 8. She was immediately intubated and taken on mechanical ventilation and one litre of intravenous crystalloid was administered. Repeat bedside X-ray chest revealed fluffy alveolar opacities in bilateral mid-zones [Fig.3]. Suspecting pulmonary edema, fluid boluses were discontinued and she was started on inotropic support for shock. She also developed copious pink frothy secretions from the endotracheal tube. She was put on lung protective settings with a low tidal volume and high PEEP for the same. The patient was shifted to the ICU with differential diagnoses of severe traumatic brain injury, neurogenic pulmonary edema and ARDS. She later succumbed to her injuries the next day.
Discussion
NPE is best described as rapid onset desaturation, tachypnoea, bilateral infiltrates on X-ray, and decreased PaO 2/FiO 2 ratio (<200) that occurs following an acute CNS injury [ 4]. The entity often remains under diagnosed or undiagnosed in routine clinical practice [ 5]. The incidence of this condition ranges from 8% to 50% across reports [ 6]. NPE in TBI is reported to occur immediately following primary brain injury. Therefore, it's often not considered and is overlooked within the list of differential diagnoses of an acute respiratory insufficiency occurring earlier or later within the course of treatment. Emphasis to the fact that NPE is to be considered in any rapid respiratory distress or decompensation that follows an acute CNS injury, must be given. The pathophysiology behind developing NPE is the catecholamine discharge from specific areas of the brain post TBI with or without a raised intracranial pressure. This discharge is primarily from the hypothalamus, bulb and spinal cord. The “blast theory” postulates that NPE is caused by a mechanism related to changes that increase hydrostatic pulmonary pressure, while the “permeability defect theory” suggests that increased pulmonary capillary permeability causes NPE [7]. The Blast theory described by Theodore and Robin in 1976 which considers an intense vasoconstriction secondary to a massive surge of sympathetic amines that occurs following an acute CNS injury is the more widely accepted theory. CNS insults like seizures or increased intracranial pressure are thought to be the cause for the fluid accumulation in the lungs due to change in hydrostatic pressure gradient across the alveolar capillary membrane and increased pulmonary vascular protein permeability [8-10]. Two distinct forms of NPE have been described in literature. The more common is an early form, which is characterized by an abrupt onset respiratory distress immediately following a CNS injury and a less common, delayed form, in which the onset of respiratory distress is delayed by 12-24 hours [11]. Severity of SAH is defined by the Hunter and Hess scale ranging from mild headache (Grade 0) to comatose (Grade V). Our patient had a Grade III SAH and developed NPE. Muroi et al. described in their study that patients who developed NPE had a higher SAH Fisher grade of 3-4 on CT. 60% mortality had been observed by them [12]. Our patient had a Fisher grade of 1 and yet developed NPE. Appropriate management of this condition lies in the early recognition and timely institution of methods to reduce ICP, mechanical ventilation using low tidal volume high PEEP, volume management which includes vasoactive drugs, diuretics and fluid supplements. Fluid management can be a challenge as one needs to titre between adequate cerebral perfusion and avoid worsening of the pulmonary edema [13]. a–adrenergic blockade using phentolamine has been used in some cases with documented high catecholamine levels [11].
Conclusion
NPE is commonly missed or undiagnosed and has high mortality rates in patients suffering from severe TBI. It should be considered in patients with sudden onset rapid desaturation and low PF ratio following a CNS injury either after a trauma or seizure. High index of suspicion (as our patient had a low grade SAH), early diagnosis and intervention by the emergency physician might improve the chances of survival in patients developing NPE due to TBI [14].
Contributors: KG is the principal author and contributed to the conception, literature review and design of the manuscript. AV, SJ, WRS, MH, AV, RA, AAK, contributed to drafting, discussion and critical revision of the manuscript. KG will act as a study guarantor. All authors approved the final version of this manuscript and are responsible for all aspects of this study. Funding: None; Competing interests: None stated.
References - Malik AB. Mechanisms of neurogenic pulmonary edema. Circ, 1985;57(1):1-18.
- Goyal K, Hazarika A, Khandelwal A, Sokhal N, Bindra A, Kumar N, et al. Non-neurological complications after traumatic brain injury: A prospective observational study. Indian J Crit Care Med. 2018;22:632-638.
- Ridenti FAS. Neurogenic pulmonary edema: a current literature review, Rev Bras Ter Intensiva. 2012;24(1):91-96.
- Baumann A, Audibert G, McDonnell J, Mertes PM. Neurogenic pulmonary edema. Acta Anaesthesiol Scand. 2007;51:447-455.
- Busl KM, Bleck TP. Neurogenic pulmonary oedema. Crit Care Med. 2015;43:1710-1715.
- Rogers FB, Shackford SR, Trevisani GT, Davis JW, Mackersie RC, Hoyt DB, et al. Neurogenic pulmonary edema in fatal and nonfatal head injuries. J Trauma. 1995;39:860-866.
- Sedy J, Zicha J, Kunes J, Jendelová P, Syková E. Mechanisms of neurogenic pulmonary edema development. Physiol Res. 2008;57(4):499-506.
- Theodore J, Robin ED. Pathogenesis of neurogenic pulmonary oedema. Lancet. 1975;2:749-751.
- Smith WS, Matthay MA. Evidence for a hydrostatic mechanism in human neurogenic pulmonary edema. Chest. 1997;111:1326-1333.
- McClellan MD, Dauber IM, Weil JV. Elevated intracranial pressure increases pulmonary vascular permeability to protein. J Appl Physiol. 1989;67:1185-1191.
- Davison DL, Terek M, Chawla LS. Neurogenic pulmonary edema. Crit Care. 2012;16:212.
- Muroi C, Keller M, Pangalu A, Fortunati M, Yonekawa Y, Keller E. Neurogenic pulmonary edema in patients with subarachnoid hemorrhage. J Neurosurg Anesthesiol. 2008;20(3):188-192.
- Busl KM, Bleck TP. Neurogenic pulmonary edema. Crit Care Med. 2015;43:1710-1715.
- Varghese R, Chakrabarty J, Menon G. Nursing management of adults with severe traumatic brain injury: A narrative review. Indian J Crit Care Med. 2017;21:684-697.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
Gupta K, Verma A, Jaiswal S, Sheikh WR, Haldar M, Vishen A, Ahuja R, Khatai AANeurogenic Pulmonary Edema : A Rare Presentation of Traumatic Brain Injury.JCR 2023;13:32-35 |
|
Gupta K, Verma A, Jaiswal S, Sheikh WR, Haldar M, Vishen A, Ahuja R, Khatai AANeurogenic Pulmonary Edema : A Rare Presentation of Traumatic Brain Injury.JCR [serial online] 2023[cited 2026 Mar 5];13:32-35. Available from: http://www.casereports.in/articles/13/2/Neurogenic-Pulmonary-Edema.html |

|
|
|
|
|