|
|
|
|
|
Duodenal Duplication Cyst in a 13-Year-Old Girl
|
|
|
|
Neha Baporikar1, D.D Sharma2, Yogesh Baberwal1, Sanjay Kalasua1 Departments of 1General Surgery and 2Pediatric Surgery, Rabindra Nath Tagore Medical College, Udaipur, Rajasthan, India. |
|
|
|
|
|
Corresponding Author:
|
|
Dr. Neha Baporikar Email: nehabaporikar@gmail.com |
|
|
|
|
|
|
|
|
Received:
02-JUN-2023 |
Accepted:
03-OCT-2023 |
Published Online:
25-NOV-2023 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
Background: Duodenal duplication cysts, though rare, require prompt recognition and precise treatment due to their distinctive clinical challenges. Diagnosis depends on factors like size, location, and proximity to surrounding structures, necessitating a tailored approach for optimal outcomes. Case Report: We present a 13-year-old girl with a duodenal duplication cyst, manifesting as persistent abdominal pain and nausea. Radiological investigations, including contrast-enhanced computed tomography and ultrasound, guided the diagnosis. The cyst's non-communicating nature and its close association with the gut lumen prompted a submucosal resection during surgery, preserving duodenal continuity. Conclusion: This case emphasizes the complexity of duodenal duplication cyst management. Surgical decisions are intricately tied to the individual characteristics of the cyst, emphasizing total resection as the ideal management. As we navigate this rare entity, insights gained contribute to refining diagnostic and therapeutic paradigms for optimal patient care. |
|
|
|
|
|
Keywords :
|
Duodenal cyst, Duplication cyst, Submucosal resection, Surgery.
|
|
|
|
|
|
|
|
|
|
|
|
Introduction
Duplication anomalies within the gastrointestinal tract are exceptionally rare congenital occurrences, manifesting in diverse locations and configurations. Ranging in size and shape, their clinical presentation is intricately tied to their specific location and dimensions. Among these anomalies, jejunal duplications are the most prevalent, followed by gastric and colonic duplications, with duodenal duplications ranking as the rarest at approximately 5% [ 1]. The scarcity of duodenal duplication cysts, coupled with their tendency to elicit non-specific symptoms, poses a formidable diagnostic puzzle.Surgical interventions, as achieving complete resection, the ultimate goal, becomes challenging due to the cyst's close proximity to adjacent bowel and surrounding structures. Consequently, surgery may involve partial resection, marsupialization, and, at times, intestinal derivation. The surgical approach is dependent upon factors such as cyst location, size, and anatomical considerations. In this case report, we explore the diagnostic and surgical intricacies surrounding a 13-year-old adolescent girl diagnosed with a duodenal cyst, who subsequently underwent surgical intervention.
Case Report
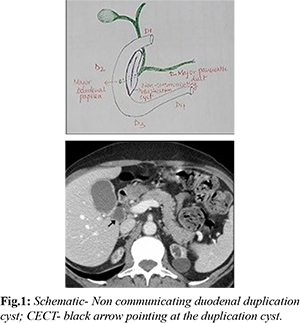
A 13-year-old female presented with upper abdominal pain persisting for the past two years. The pain, characterized as vague and dull, predominantly localized to the peri-umbilical region, particularly on the right side, and was accompanied by minimal appetite loss. Notably, there were no associated symptoms of nausea, vomiting, or altered bowel habits. On admission, the patient appeared alert, conscious, and vitally stable, exhibiting a lean build and pallor. Regional examination revealed slight tenderness upon deep palpation in the peri-umbilical region, with no discernible swelling, lump, or organomegaly. Initial investigations revealed a hemoglobin level of 9.1 g/dL, with other blood parameters within normal limits. X-ray FPA and ultrasonography (USG) of the whole abdomen did not yield significant findings. However, contrast-enhanced computed tomography (CECT) of the abdomen unveiled a thick-walled cystic lesion measuring approximately 45×36×35 mm in the supraumbilical region [Fig.1]. The lesion exhibited internal air-fluid levels and adjacent areas of increased vascularity. Subsequent repeat USG confirmed the cyst's presence, exhibiting gut wall signatures, leading to a diagnosis of a duodenal duplication cyst.Following optimization of hemoglobin levels and pre-anesthetic evaluation, the patient underwent an elective laparotomy. Exploration of the bowel revealed a cystic lesion adjacent and posterior to D2 and D3, sharing a common wall with the duodenum and adhering to the pancreas. The cyst was carefully separated, and clear fluid aspirated for cytology and biochemistry analysis. Upon opening the cyst, its internal features resembled bowel wall characteristics. Importantly, no communication was identified between the cyst and other structures, including the bowel, pancreatic duct, or biliary system.
Subsequently, submucosal resection was performed, given the sufficient thickness of the mucosa and submucosa [Fig.2]. The excess cyst wall was excised, and the remaining cavity was obliterated. Closure of the abdomen followed confirmation of hemostasis, with the resected specimen sent for biopsy. The patient was successfully extubated, and the post-operative course remained uneventful. Discharge occurred after 10 days, once oral intake was tolerated, and normal bowel function resumed. Post-operative examination of the aspirated fluid revealed a transudate nature with no enzymatic abnormalities. Histopathological analysis of the resected specimen demonstrated mucosal glands with submucosal dilated and congestive changes, consistent with the diagnosis of a duplication cyst.
Discussion
Duplication cysts, although rare congenital malformations, can manifest at various sites within the gastrointestinal tract. The duodenum is an infrequent location, accounting for only 2% of cases, with jejunal duplications being the most common [ 2]. These cysts, whether cystic or tubular, communicating or non-communicating, present diverse clinical challenges. Communicating cysts pose an elevated risk of complications, including obstruction, bleeding, and perforation. Typically possessing well-developed smooth muscle layers and mucous membranes derived from the gastrointestinal tract, these cysts often share a common wall with adjacent hollow organs and may reside in the mesentery [ 3]. Embryologically, several theories attempt to explain gut duplications, such as Bremer's aberrant recanalization theory and Lewis and Thyng's Diverticular theory. Bentley proposed the split notochord theory, particularly relevant to duplications associated with spinal anomalies [4]. The clinical presentation of duodenal duplication cysts varies based on type, site, and size, with abdominal pain being the most common manifestation. Other presentations may include a palpable mass, signs of intestinal obstruction, bleeding, perforation, jaundice, or pancreatitis due to biliary obstruction [2]. In the presented case, the 13-year-old patient experienced persistent, dull abdominal pain with associated nausea. Notably, the cyst being non-communicating mitigated symptoms of obstruction, pancreatitis, or jaundice. Radiological investigations, although crucial for diagnosis, can be challenging, and barium studies, abdominal and endoscopic ultrasound (US), and CT scans play pivotal roles. The gut signature observed in the cyst wall, indicative of the layered pattern with hyperechoic inner and hypoechoic outer layers, aids in differentiation [6]. CT imaging, alongside clinical considerations, guided the diagnosis in this case, distinguishing it from other cystic lesions. While MRI and gastroduodenoscopy are alternative diagnostic modalities, they were deemed unnecessary in this instance. Histological examination subsequently confirmed the diagnosis, categorizing the cyst based on the nature of its common wall and presence of biliary or pancreatic ducts [1]. Ideally, total resection stands as the preferred surgical approach for duodenal duplication cysts. However, the close association with the biliary-pancreatic system poses challenges, often necessitating a pancreaticoduodenectomy a major surgery with elevated morbidity and mortality. In less invasive scenarios, partial resection or internal derivation may be considered, preserving areas of maximum adherence to the duodenum [7]. In the current case, the non-communicating nature of the duplication, coupled with its common wall with the gut lumen, posed challenges for total resection. Consequently, a submucosal resection was performed, excising the free wall of the cyst while maintaining duodenal continuity. This approach aligned with the surgical principle of balancing the need for cyst removal with preserving essential anatomical structures.
Conclusion
The scarcity of duodenal duplication cysts emphasizes the need to maintain a high index of suspicion for timely diagnosis and effective treatment. The size, location, and relationship with adjacent structures significantly influence the choice of surgical intervention. While total resection stands as the ideal goal, cases involving communication or close adherence may warrant a more nuanced approach, such as partial resection or marsupialization, to ensure optimal outcomes.
Contributors: NB: manuscript writing and patient management; DDS: manuscript editing, patient management. DDS will act as a study guarantor. YB and SK: data collection and patient management.NB will act as a study guarantor. All authors approved the final version of the manuscript and are responsible for all aspects of this study. Funding: None; Competing interests: None stated.
References - Merrot T, Anastasescu R, Pankevych T, Tercier S, Garcia S, Alessandrini P, et al. Duodenal duplications. Clinical characteristics, embryological hypotheses, histological findings, treatment. European Journal of Pediatric Surgery. 2016;16(1):18-23.
- Chen JJ, Lee HC, Yeung CY, Chan WT, Jiang CB, Sheu JC. Meta-analysis: the clinical features of the duodenal duplication cyst. Journal of Pediatric Surgery. 2010;45(8):1598-1606.
- Spataru RI, Lupusoru M, Serban D, Ivanov M, Iozsa DA. Alimentary tract duplications in children - a 15 years' experience. Romanian Journal of Morphology and Embryology. 2021;62(3):751-756.
- Sharma D, Bharany RP, Mapshekhar RV. Duplication cyst of pyloric canal: a rare cause of pediatric gastric outlet obstruction: rare case report. The Indian Journal of Surgery. 2013;75(Suppl 1):322-325.
- Lewis FT, Thyng FW. The regular occurrence of intestinal diverticula in embryos of the pig, rabbit, and man. American Journal of Anatomy. 1908;7(4):505-519.
- Sangüesa Nebot C, Llorens Salvador R, Carazo Palacios E, Picó Aliaga S, Ibañez Pradas, V. Enteric duplication cysts in children: varied presentations, varied imaging findings. Insights into Imaging. 2018;9(6):1097-1106.
- Seeliger B, Piardi T, Marzano E, Mutter D, Marescaux J, Pessaux P. Duodenal duplication cyst: A potentially malignant disease. Ann Surg Oncol. 2012;19:3753-3754.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
Baporikar N, Sharma D.D, Baberwal Y, Kalasua SDuodenal Duplication Cyst in a 13-Year-Old Girl.JCR 2023;13:118-121 |
|
Baporikar N, Sharma D.D, Baberwal Y, Kalasua SDuodenal Duplication Cyst in a 13-Year-Old Girl.JCR [serial online] 2023[cited 2026 Jan 14];13:118-121. Available from: http://www.casereports.in/articles/13/4/Duodenal-Duplication-Cyst-in-a-13-Year-Old-Girl.html |

|
|
|
|
|