|
|
|
|
|
Lurking in the Lungs: Unveiling Bronchopulmonary Lophomoniasis
|
|
|
|
Neeta Gade1, Satyajeet Sahoo2, Soumyabrata Nag1, Vishal Shete1, Meena Mishra1, Pooja Taiwade1 Departments of 1Microbiology and 2Pulmonary Medicine, All India Institute of Medical Sciences, Nagpur, Maharashtra, India. |
|
|
|
|
|
Corresponding Author:
|
|
Dr. Neeta Gade Email: drneetagade@aiimsnagpur.edu.in |
|
|
|
|
|
|
|
|
Received:
09-JUL-2023 |
Accepted:
08-SEP-2023 |
Published Online:
05-OCT-2023 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
Background: Lophomonas, a protozoa gaining recognition as a pathogen, has drawn increased attention owing to its link with respiratory tract infections. Typically residing in the hind-gut of cockroaches, Lophomonas has been identified as a causative agent impacting both upper and lower respiratory tracts in humans. This case report presents an unusual instance of bronchopulmonary lophomoniasis in a patient from Central India. Case Report: A 44-year-old man, who had previously contracted COVID-19, visited the Pulmonary Medicine outpatient department (OPD) with enduring respiratory symptoms. Despite undergoing various rounds of both injectable and oral antibiotics, there was no improvement in the patient's condition. Radiological examination revealed interstitial haziness and consolidation in the left mid and lower zones, accompanied by mild cardiomegaly on chest X-ray. Broncho-alveolar lavage (BAL) fluid analysis through wet mount examination, Giemsa, and Trichrome stain unveiled the presence of Lophomonas blattarum. Conclusion: This unique case illuminates the need for heightened awareness among healthcare professionals regarding the potential involvement of uncommon pathogens like Lophomonas in respiratory illnesses. The successful diagnosis through microscopic examination demonstrates the pivotal role of such techniques in guiding appropriate and targeted treatment. |
|
|
|
|
|
Keywords :
|
Antibiotics, Broncho Alveolar lavage, Fever, Lungs, Pneumonia.
|
|
|
|
|
|
|
|
|
|
|
|
Introduction
Parasitic infections are a major health concern that affects millions of people worldwide. Globalisation, climate changes, increased international travel, and increasing numbers of immunocompromised individuals have contributed to the increased vulnerability of population to parasitic diseases [1]. A diverse range of helminths and protozoa has the potential to impact the respiratory system, with clinical manifestations varying from asymptomatic infection to severe and life-threatening conditions. Lophomonas, a unicellular flagellated protozoan parasite, is emerging as a notable pulmonary pathogenic protozoan in recent times. The first report of human pulmonary infection by Lophomonas was reported by Chen and Meng from China in 1993 [2]. During the last decade, cases of human lophomoniasis in both immunocompromised and immunocompetent individuals affecting both upper and lower respiratory tract have been reported from several tropical countries such as China, Iran, Peru, Mexico, Turkey, India [3,4]. It is difficult to distinguish respiratory symptoms of bronchopulmonary lophomoniasis from symptoms of other common respiratory conditions like bronchial asthma, pneumonia, and bronchopulmonary diseases [5]. The laboratory diagnosis of bronchopulmonary lophomoniasis primarily involves the microscopic examination of morphological characteristics of multi-flagellated protozoa in different specimens like sputum, broncho-alveolar lavage (BAL), or tracheal aspirate. Nevertheless, discerning and distinguishing Lophomonas from ciliated bronchial epithelial cells using light microscopy can pose challenges. Thus, a polymerase chain reaction (PCR) test has been developed recently to overcome the microscopic diagnostic pitfalls but due to its limited availability, use of staining techniques remains crucial in preventing identification errors [6]. Swift and precise identification of this protozoan with multiple flagella is essential for guiding the correct treatment, considering that Metronidazole is the preferred drug for lophomoniasis, which is not typically prescribed empirically for common respiratory infections [7]. Here, we present an unusual case of bronchopulmonary lophomoniasis involving a young male patient who sought medical attention at Pulmonary Medicine OPD of our tertiary healthcare centre in Central India.
Case Report
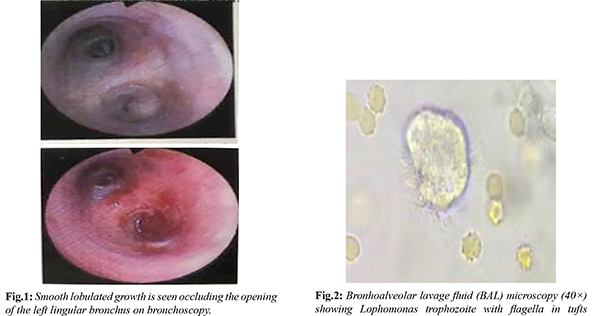
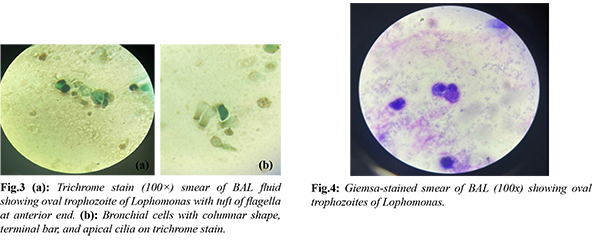
A 44-year-old male farmer, residing in Maharashtra, India presented with recurrent history of febrile illness for six months. It was characterised by high-grade fever with chills, headache, cough with expectoration, and shortness of breath. He was treated at various hospitals, with parenteral and oral antibiotics, without improvement, before admission at our facility. The patient had a history of mild coronavirus disease 2019 (COVID-19) in April 2021 two months before the onset of presenting complaints. The patient had no history of any other underlying co-morbid condition. On admission, the patient was febrile (101°F), and tachypneic (Respiratory rate - 28/min). Other vital parameters were within normal limits. During the examination of the respiratory system, bronchial breathing was observed in the left lower zone of the lung. Laboratory analysis indicated a total leukocyte count of 14,200/cu.mm, with 84% polymorphonuclear cells, 9% lymphocytes, and 4% eosinophils. His liver function tests and kidney function tests were within normal limits. Cultures of blood, sputum, and urine did not yield the growth of pathogens. The chest X-ray displayed interstitial haziness and consolidation in the left mid and lower zones, along with mild cardiomegaly. Subsequent fibreoptic bronchoscopy revealed a smooth, lobulated growth obstructing the opening of the left lingular bronchus [Fig.1]. BAL fluid with biopsy tissue were obtained. Wet mount examination of BAL sample under microscope revealed many live, oval, approx. 20-30 µm in size, motile ciliary structures with granular cytoplasm [Fig.2 and Video 1]. Morphologically it was identified as Lophomonas blattarum. Giemsa and Trichrome staining were performed on the BAL sample smear to validate the observations. Trichrome stain smear proved instrumental in distinctly recognising and distinguishing the oval trophozoite of Lophomonas with a tuft of flagella from bronchial cells exhibiting columnar shape, terminal bar, and apical cilia [Fig.3,4]. KOH examination and acid-fast bacilli staining of BAL sample were negative. Cytology report of biopsy tissue was negative for malignant cells. No organisms were cultured from BAL sample. The patient was initiated on a course of oral Metronidazole at a dosage of 400 mg three times a day for a duration of 14 days. A positive response was observed, as evidenced by improvement in a subsequent chest X-ray and the absence of the protozoa in a repeat bronchoalveolar lavage sample.
Discussion
Lophomonas are anaerobic, free-living multi-flagellate parabasalids existing in diverse aquatic settings, including freshwater, brackish water, and marine environments. Lophomonas comprises two species: Lophomonas blattarum and Lophomonas striata. Both are found as a commensal agent in the hind-gut of certain arthropods such as termites and omnivorous roaches, several species of cockroaches including Blatta orientalis, Periplaneta americana, and Blattella germanica. The parasite demonstrates both trophozoite and cyst phases; nevertheless, only the trophozoite stage is observable in human tissue, whereas both forms are visible in the gut of the insect host. It is excreted in the faeces of the host into the environment, where it forms cysts under external environmental conditions. The cyst form may be inhaled and parasitised in the human respiratory tract and can cause sinusitis or broncho-pulmonary infection [8]. It has been incriminated in a variety of other human diseases like gastroenteritis, and diarrhoea and sometimes may also lead to more serious complications such as liver damage, anaemia, and even death. The protozoon trophozoite appears as round-ovoid or piriform in shape with 20-60 µm in length and 12-20 µm in width. The cytoplasm looks granular, with some phagocytosed food particles. At one of the poles (the apical zone), the protozoon has a tuft of numerous flagella. The outer flagella are smaller, distinct, and arranged in an irregular orientation. On occasion, the nucleus may be observed as a round dark structure positioned slightly below the point where the flagella attach [1,5]. Lophomoniasis has been documented in 10 countries spanning four continents, with a predominant occurrence in Asia. Due to limited awareness among researchers and physicians globally about the Lophomonas parasite, its actual prevalence is often underestimated, positioning it as a neglected tropical infection in various regions. A systematic review of reported cases by Nakhaei et al. demonstrated a 91.85% prevalence of Lophomonas in Asia, 7.2% in America, 0.65% in Europe, and 0.3% in Africa [9]. Iran reported the highest number of cases, followed by China, with five cases documented in India to date. Notably, many published cases exhibited indications of prior or concurrent respiratory conditions [9]. This case report details an instance of bronchopulmonary lophomoniasis in a male patient who manifested with non-resolving pneumonia. Literature has reported co-infections of Lophomonas with HIV and TB [8-10]. Notably a recent study by Nakhaei et al. from Iran highlighted co-infection of L. blattarum with COVID-19 [11]. Our patient's presentation occurred six months post his COVID-19 illness, without a comprehensive diagnostic evaluation in the interim for his recurrent respiratory symptoms. Given the heightened risk of COVID-19 transmission, physicians often avoided direct BAL sampling during the pandemic. In our specific case, although the sputum sample showed no evidence of Lophomonas, a conclusive diagnosis was achieved through diagnostic bronchoscopy. Identifying Lophomonas is challenging, with culture proving difficult; therefore, the primary methods for detection are wet mount and stained smear examinations using light microscopy. In our case, the application of trichrome staining on the BAL smear demonstrated enhanced effectiveness in differentiating Lophomonas from bronchial cells. Maintaining a high level of suspicion and conducting a thorough diagnostic evaluation are crucial for diagnosing this overlooked pulmonary parasitic infection. The effective response to oral Metronidazole underscores the significance of precise diagnosis in guiding the implementation of suitable therapeutic measures.
Conclusion
As we navigate the complexities of respiratory infections, especially those resistant to conventional therapies, this case serves as a reminder of the importance of thorough investigations and a multidisciplinary approach. Recording instances of such unusual cases in non-endemic regions play a crucial role in advancing our understanding of atypical infections like Lophomonas. This is essential for improving diagnostic approaches, optimising treatment results, and ultimately enhancing the overall management of respiratory conditions.
Contributors: NG, SN: laboratory diagnostic part, manuscript writing, literature search; SS: manuscript editing, patient management; VS, MM, PT: critical inputs into the manuscript. NG will act as a study guarantor. All authors approved the final version of this manuscript and are responsible for all aspects of this study. Funding: None; Competing interests: None stated.
References - Khemasuwan D, Farver C, Mehta AC. Parasitic diseases of the lung. Diseases of the central airways. 2016 Mar 24:231-253.
- Chen SX, Meng ZX. Report on one case of Lophomonas blattarum in the respiratory tract. Chinese J Parasitol Parasit Dis. 1993;11:28.
- Al Ramahi JW, Masoudi OM, Jabali A, Elayyan MN, Matar A. Lower respiratory tract infection due to Lophomonas blattarum: A report of two cases and a review. J Infect Dis Ther. 2022;S3:006.
- González SN, Otero MF, Rivas LF, Galvis TD, Venegas ME, Arias DE, et al. Bronchopulmonary infection by Lophomonas blattarum in a pediatric patient after hematopoietic progenitor cell transplantation: first report in Mexico. J Thorac Dis. 2017;9:E899-902.
- Li R, Gao ZC. Lophomonas blattarum infection or just the movement of ciliated epithelial cells? Chin Med J (Engl). 2016;129(6):739-742.
- Fakhar M, Nakhaei M, Sharifpour A, Kalani H, Banimostafavi ES, Abedi S, et al. First molecular diagnosis of lophomoniasis: the end of a controversial story. Acta Parasitol. 2019;64(2):390-393.
- Shi YL, Li LH, Liao Y, Li XN, Huang XY, Liu J, et al. Diagnosis and treatment of Lophomonas blattarum infection in 26 patients with bacterial pneumonia. 2007;25(5):430-431.
- Martinez-Girón R, Cornelis van Woerden H. Lophomonas blattarum and bronchopulmonary disease. J Med Microbiol. 2013;62(Pt 11):1641-1648.
- Nakhaei M, Fakhar M, Sharifpour A, Hezarjaribi HZ, Banimostafavi ES, Nazar E. Global status of emerging Lophomonas infection: A systematic review of reported cases (1993-2020). Interdisciplinary Perspectives on Infectious Diseases. 2022;3155845.
- Verma S, Verma G, Singh DV, Mokta J, Negi RS, Jhobta A, et al. Dual infection with pulmonary tuberculosis and Lophomonas blattarum in India. Int J Tuberc Lung Dis. 2015;19:368-369.
- Sharifpour A, Zakariaei Z, Fakhar M, Banimostafavi ES, Nakhaei M, Soleymani M. Post-COVID-19 co-morbidity of emerged Lophomonas infection and invasive pulmonary aspergillosis: First case report. Clin Case Rep. 2021;9(9):e04822.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
Gade N, Sahoo S, Nag S, Shete V, Mishra M, Taiwade PLurking in the Lungs: Unveiling Bronchopulmonary Lophomoniasis.JCR 2023;13:101-105 |
|
Gade N, Sahoo S, Nag S, Shete V, Mishra M, Taiwade PLurking in the Lungs: Unveiling Bronchopulmonary Lophomoniasis.JCR [serial online] 2023[cited 2025 Oct 5];13:101-105. Available from: http://www.casereports.in/articles/13/4/Lurking-in-the-Lungs.html |

|
|
|
|
|