|
|
|
|
|
Prostate Specific Membrane Antigen Avid Thyroid Cancer in Patients with Prostate Cancer: A Report of Two Cases
|
|
|
|
Saranya Sasikala1, Anand Narayan Chinnachamy1, Arumugam Rajkumar2, Arulraj Pitchamuthu3 Departments of Radiation Oncology1, Medical Oncology2 and Surgical Oncology3, Valavadi Narayanasamy Cancer Center, G. Kuppuswamy Naidu Memorial Hospital, Coimbatore 641037, India. |
|
|
|
|
|
Corresponding Author:
|
|
Dr. Saranya Sasikala Email: drsaranyasasikala@gmail.com |
|
|
|
|
|
|
|
|
Received:
10-MAY-2023 |
Accepted:
14-OCT-2023 |
Published Online:
15-NOV-2023 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
Background: Ga-68 labelled Prostate specific membrane antigen-Positron emission tomography (PSMA-PET) is widely used in staging of intermediate and high-risk prostate cancer or restaging after biochemical recurrence. Despite the term “prostate specific”, incidental uptake with Ga-68 PSMA-PET in benign and non-prostatic malignancy has been reported. Case Report: Here we present two cases of carcinoma prostate with PSMA-PET avid lesions in thyroid, requiring further evaluations due to its non-specificity and on evaluation found to be a synchronous double malignancy of prostate and carcinoma thyroid. Conclusion: PSMA-PET, though has high sensitivity and specificity in staging for prostate cancer, can be taken up by multiple other malignancies and non-malignant conditions. If clinical picture warrants, additional confirmatory investigations are required, might change the staging and the treatment. |
|
|
|
|
|
Keywords :
|
Biopsy, Lung, Prostate, Prostate Specific Antigen, Staging, Thyroid.
|
|
|
|
|
|
|
|
|
|
|
|
Introduction
Ga-68 labelled Prostate specific membrane antigen- Positron emission tomography (PSMA-PET) is widely used in staging of intermediate and high-risk prostate cancer or restaging after biochemical recurrence. PSMA is a type II integral membrane glycoprotein in cell surface, involved in hydrolysis of N-acetyl L-aspartyl L-glutamide into N-acetyl L-aspartate and L-glutamate. PSMA is expressed 10-80 fold in almost all cancer cells of prostate and its transmembrane location with large extracellular domain provides an accurate target for detection of extra-prostatic disease, lymph nodes and bone lesions [ 1- 3]. Despite the term “prostate specific”, several case reports describing the incidental uptake with Ga-68, PSMA-PET in benign and non-prostatic malignancy has been reported [ 4- 6]. Here we present two cases of carcinoma prostate with PSMA-PET avid lesions in thyroid, requiring further evaluations due to its non-specificity and on evaluation found to be a synchronous double malignancy of prostate and thyroid.
Case Report
Case 1
A 72 years old male presented with complaints of lower urinary tract symptoms for 2 months duration. Serum PSA done was 15 ng/mL. MRI of pelvis showed prostate measuring 4.8×3.6×3.9 cm, volume 34 cc, diffuse T2W hypo-intensity noted in entire prostate with loss of zonal differentiation. An ill-defined early enhancing lesion noted in left side of the mid gland of prostate measuring 1.9×1.4 cm. Peri-prostatic fat planes were indistinct on the left side. No pelvic or para-aortic lymphadenopathy was seen. Histopathological examination of trans-rectal ultrasound guided biopsy of prostate revealed acinar adenocarcinoma Gleasons score of 3+4 (grade group 2) involving 13 out of 14 cores. PSMA-PET CT showed avid lesions in prostate, thyroid, enlarged pre-tracheal node and multiple pleural nodules in right lung [Fig.1].
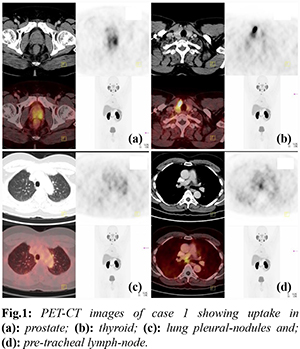
A differential diagnosis of carcinoma prostate with metastasis or synchronous double primary in thyroid was made. Ultrasound (USG) guided biopsy of thyroid lesion and pre-tracheal node revealed follicular neoplasm. Immunohistochemistry was positive for TTF-1 and thyroglobulin and negative for PSA. He underwent thoracoscopy and biopsy of the pleural nodule in order to determine the origin. Histopathological examination showed metastatic adenocarcinomatous deposit in the pleural and lung from a primary prostatic acinar adenocarcinoma with immunohistochemistry strongly positive for PSA and negative for TTF-1. Patient underwent total thyroidectomy with central lymph node dissection and bilateral orchidectomy. Thyroid gland showed follicular variant of papillary carcinoma involving both lobes of thyroid with three nodes positive for metastasis. Post-operative Iodine-131 scan with 1.5 mCi showed minimal residual thyroid tissue in the neck. He received radioiodine ablation therapy with 30mCi of I-131 and six cycles of palliative chemotherapy with Docetaxel and Prednisolone. Post-chemotherapy PSMA-PET scan showed no evidence of disease in the body and serum PSA reduced to 0.01 ng/mL. Whole body Iodine-131 scan showed no residual disease. Patient is biochemically and clinico-radiologically disease free 18 months since completion of treatment.
Case 2
A 58-year-old male evaluated for complaints of lower abdominal pain for two months duration, serum PSA done was 48 ng/ml. MRI of pelvis showed limited disease in prostate with extra-capsular extension and sub-centrimetric iliac nodes. Histopathological examination of trans-rectal ultrasound guided biopsy of prostate revealed adenocarcinoma with Gleason’s score of 7 (3+4), grade group 2. PSMA-PET CT showed avid lesions in prostate and left lobe of thyroid. USG neck done revealed 3.3×2.9×2.9 cm nodule in the left lobe of thyroid with focal extra-thyroid extension into the neck anteriorly. Fine needle aspiration cytology of the left thyroid nodule was suspicious of papillary carcinoma. Patient underwent total thyroidectomy with central lymph node dissection and bilateral orchidectomy. Thyroid gland showed classic papillary carcinoma in the left lobe of thyroid thyroid with lympho-vascular space invasion and extra-thyroid extension to neck strap muscles with one node positive for metastasis. He is being planned for post-operative Iodine-131 scan and radical radiotherapy to prostate and pelvic nodes.
Discussion
PSMA is consistently expressed in prostate cancer epithelium, enabling detection of prostate cancer with 80% sensitivity and 97% specificity on per lesion analysis and also detects relapse and metastasis with 95% sensitivity with positive predictive value of 98%. Therefore, it is used in diagnosis, staging, restaging, response to therapy and prognostication [ 4, 5] and has paved way for radio-ligand therapy. However, wide range of benign and malignant tumors shows heterogeneous expression of PSMA in cancer neo-vasculature. Endothelial expression is most likely responsible for the radiotracer uptake on PSMA imaging for many benign conditions as well like meningioma, cerebral infarct/ haemorrhage, lung consolidation, gynecomastia, venous thrombosis. Several isolated case reports have shown incidental PSMA uptake in especially in high grade glioma, renal cell carcinoma, thyroid [7-9] and lung cancer, multiple myeloma and malignant melanoma, of which renal cell carcinoma has been the most abundantly reported. PSMA-PET has proved superiority in detection of brain metastasis over FDG-PET. Expression of PSMA in thyroid cancer is a recent interest in determining the utility and feasibility in detection as PSMA is expressed in the microvasculature and to facilitate improved therapies especially in aggressive and less differentiated thyroid cancer refractory to radioiodine therapy [10,11]. In our cases, patients diagnosed with carcinoma prostate had an incidental uptake of PSMA tracer in thyroid gland with possibilities of metastasis from prostate [12,13] or second primary. The non-specific uptake in thyroid primary also necessitated the evaluation of lung lesions to ascertain its origin.
Conclusion
PSMA-PET, though has high sensitivity and specificity in staging for prostate cancer, can be taken up by multiple other malignancies and non-malignant conditions. If clinical picture warrants, additional confirmatory investigations are required, might change the staging and the treatment.
Contributors: SS: manuscript writing, patient management; ANC: manuscript editing, patient management; AR, AP: critical inputs into the manuscript. SS will act as a study guarantor. All authors approved the final version of this manuscript and are responsible for all aspects of this study. Funding: None; Competing interests: None stated.
References - Bostwick DG, Pacelli A, Blute M, Roche P, Murphy GP. Prostate specific membrane antigen expression in prostatic intraepithelial neoplasia and adenocarcinoma: a study of 184 cases. Cancer. 1998;82(11):2256-2261.
- Lapidus RG, Tiffany CW, Isaacs JT, Slusher BS. Prostate-specific membrane antigen (PSMA) enzyme activity is elevated in prostate cancer cells. The Prostate. 2000;45(4):350-354.
- Conway RE, Petrovic N, Li Z, Heston W, Wu D, Shapiro LH. Prostate-specific membrane antigen regulates angiogenesis by modulating integrin signal transduction. Molecular and Cellular Biology. 2006;26(14):5310-5324.
- Perera M, Papa N, Christidis D, Wetherell D, Hofman MS, Murphy DG, Bolton D, et al. Sensitivity, specificity, and predictors of positive 68Ga–prostate-specific membrane antigen positron emission tomography in advanced prostate cancer: a systematic review and meta-analysis. European Urology. 2016;70(6):926-937.
- Pyka T, Okamoto S, Dahlbender M, Tauber R, Retz M, Heck M, et al. Comparison of bone scintigraphy and 68 Ga-PSMA PET for skeletal staging in prostate cancer. European Journal of Nuclear Medicine and Molecular Imaging. 2016;43(12):2114-2121.
- Malik D, Sood A, Mittal BR, Singh H, Basher RK, Shukla J, et al. Nonspecific uptake of 68Ga-prostate-specific membrane antigen in diseases other than prostate malignancy on positron emission tomography/computed tomography imaging: a pictorial assay and review of literature. Indian Journal of Nuclear Medicine. 2018;33(4):317.
- Sager S, Vatankulu B, Uslu L, Sönmezoglu K. Incidental detection of follicular thyroid carcinoma in 68Ga-PSMA PET/CT imaging. Journal of Nuclear Medicine Technology. 2016;44(3):199-200.
- Jena A, Zaidi S, Kashyap V, Jha A, Taneja S. PSMA expression in multinodular thyroid neoplasm on simultaneous Ga-68-PSMA PET/MRI. Indian Journal of Nuclear Medicine. 2017;32(2):159.
- Jena A, Zaidi S, Kashyap V, Jha A, Taneja S. PSMA expression in multinodular thyroid neoplasm on simultaneous Ga-68-PSMA PET/MRI. Indian Journal of Nuclear Medicine. 2017;32(2):159-161.
- Lodewijk L, Willems SM, Dreijerink KM, de Keizer B, van Diest PJ, Schepers A, et al. The theranostic target prostate-specific membrane antigen is expressed in medullary thyroid cancer. Human Pathology. 2018;81:245-254.
- de Vries LH, Lodewijk L, Braat AJ, Krijger GC, Valk GD, Lam MG, et al. 68 Ga-PSMA PET/CT in radioactive iodine-refractory differentiated thyroid cancer and first treatment results with 177 Lu-PSMA-617. EJNMMI Research. 2020;10(1):1-8.
- Selimoglu H, Duran C, Saraydaroglu O, Guclu M, Kiyici S, Ersoy C, et al. Prostate cancer metastasis to thyroid gland. Tumori Journal. 2007;93(3):292-295.
- Albsoul NM, Obeidat FN, Hadidy AM, AlZoubi MN, Taib AA, Shahait AD. Isolated multiple bilateral thyroid metastases from prostatic adenocarcinoma: case report and literature review. Endocrine Pathology. 2013;24(1):36-39.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
Sasikala S, Chinnachamy AN, Rajkumar A, Pitchamuthu AProstate Specific Membrane Antigen Avid Thyroid Cancer in Patients with Prostate Cancer: A Report of Two Cases.JCR 2023;13:114-117 |
|
Sasikala S, Chinnachamy AN, Rajkumar A, Pitchamuthu AProstate Specific Membrane Antigen Avid Thyroid Cancer in Patients with Prostate Cancer: A Report of Two Cases.JCR [serial online] 2023[cited 2026 Jan 5];13:114-117. Available from: http://www.casereports.in/articles/13/4/Prostate-Specific-Membrane-Antigen-Avid-Thyroid-Cancer-in-Patients-with-Prostate-Cancer.html |

|
|
|
|
|