|
|
|
|
|
Successful Management of Corneal Perforation Following Keratoplasty with Emergency Periosteal Grafting
|
|
|
|
Cut Putri Samira, Dian Islami Rumah Sakit Umum Cempaka Lima Banda Aceh, Aceh, Indonesia. |
|
|
|
|
|
Corresponding Author:
|
|
Dr Dian Islami Email: dianislami78@gmail.com |
|
|
|
|
|
|
|
|
Received:
28-DEC-2024 |
Accepted:
30-APR-2025 |
Published Online:
25-JUL-2025 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
Background: Corneal ulcers, if left untreated, can progress to perforation, threatening both vision and ocular integrity. When corneal donor tissue is unavailable, periosteal grafts provide a temporary solution to preserve eye structure and manage infection until definitive intervention becomes feasible. Case Report: A 39-year-old woman underwent a periosteal graft for a perforated corneal ulcer in her right eye. While the graft preserved the globe's integrity, her vision was limited to hand movement. In 2024, penetrating keratoplasty (PK) was performed, achieving a corrected distance visual acuity (CDVA) of 6/24 five months postoperatively with a clear graft. However, at seven months, CDVA decreased to 6/40 due to cataract progression, with cataract surgery planned to improve visual outcomes further. Conclusion: This case highlights the role of periosteal grafts in maintaining ocular integrity when donor tissue is inaccessible and demonstrates the potential for delayed PK to yield substantial visual improvement. Comprehensive postoperative care and planned cataract surgery are critical for optimizing long-term outcomes and enhancing patient satisfaction. |
|
|
|
|
|
Keywords :
|
Cornea, Corneal Ulcer, Donors, Infection, Penetrating Keratoplasty, Visual Acuity.
|
|
|
|
|
|
|
|
|
|
|
|
Introduction
Corneal ulcers are characterised by a breach in the corneal epithelium leading to tissue necrosis, stromal swelling, and cellular infiltration. Perforation can occur when the ulcer progresses deeply enough to create a full-thickness defect, which can be identified by fluorescein dye leakage on slit-lamp examination. Patients typically present with vision loss, ocular pain, and clear fluid leakage that may be mistaken for tears [ 1]. In resource-limited settings where donor corneas are not readily available, periosteal grafts harvested from the anterior tibial crest have been utilised as an emergency measure to manage corneal perforations [ 2]. These grafts provide tectonic support to maintain globe integrity and control infection, although they do not restore vision. This case report describes a patient who initially underwent a temporary periosteal graft in the right eye as an urgent intervention for a perforated infectious corneal ulcer when donor tissue was unavailable. The primary aim was to preserve ocular structure and resolve infection. Three years later, to improve vision and cosmetic appearance, the patient underwent penetrating keratoplasty (PK) [3]. PK, involving the complete removal of the diseased cornea and its replacement with a healthy donor cornea, remains a definitive treatment for various corneal pathologies and is vital in achieving meaningful visual rehabilitation [4].
Case Report
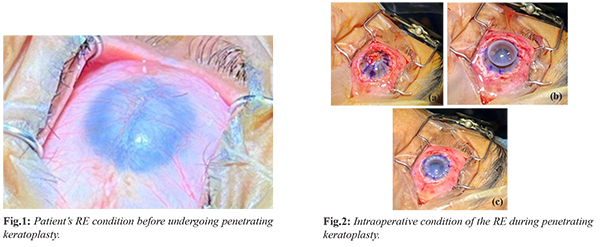
A 39-year-old female presented in 2020 with a 4 mm infectious corneal perforation in her right eye (RE). Due to unavailability of donor tissue, a periosteal graft from the anterior tibial crest was performed along with systemic and topical antibiotics, effectively resolving the infection and preserving globe integrity. Postoperatively, her visual acuity remained hand movement, classified as blindness by WHO. Financial constraints and donor shortage delayed keratoplasty for three years. On presentation before penetrating keratoplasty (PK), the RE appeared quiet with an integrated periosteal graft [Fig.1], visual acuity was hand movement, left eye vision was 6/6, and intraocular pressures were normal in both eyes (14 mm Hg) [Fig.2].
PK with an 8 mm donor graft was performed uneventfully. Postoperative therapy included oral levofloxacin 500 mg daily, methylprednisolone 16 mg twice daily, and frequent topical levofloxacin and prednisolone drops. Acetazolamide drops were added to maintain intraocular pressure. One-week post-PK, corrected distance visual acuity (CDVA) in the RE improved to counting fingers at 3 meters. Five months later, after suture removal, CDVA further improved to 6/24, although the patient reported a smoky vision due to developing cataract [Fig.3]. At seven months, the graft remained clear [Fig.4], but CDVA declined to 6/40 due to progressive cataract formation, with no improvement on pinhole testing. Astigmatism was measured at R1 38.73 mm and R2 42.12 mm, and IOP reduced to 9.2 mmHg. Current therapy includes fluorometholone and neomycin sulfate drops once daily. Planned management is cataract surgery with intraocular lens (IOL) implantation to optimise visual outcomes.
Discussion
Periosteal grafts, derived from the highly vascularised periosteum, provide an effective autologous option for emergency management of corneal perforations when donor tissue is unavailable [ 3]. In this patient, the graft successfully preserved globe integrity and controlled infection, though it did not improve vision. Definitive visual rehabilitation required penetrating keratoplasty (PK), a full-thickness corneal transplant that replaces diseased cornea with a donor graft [ 4, 5]. Post-operative outcomes of PK depend on multiple factors, including graft clarity and immune tolerance. Steroids and immunosuppressive agents are central to preventing rejection and maintaining graft viability [6]. In this case, a combination of systemic and topical levofloxacin was administered to prevent infection, aligning with evidence supporting dual antimicrobial coverage for graft protection [7,8]. Corticosteroid therapy remains the cornerstone of antirejection regimens. The patient received systemic methylprednisolone alongside frequent topical prednisolone, ensuring robust immunosuppression [9,10]. Gradual tapering of topical steroids reduces long-term risks such as glaucoma, cataract, and delayed wound healing while sustaining graft acceptance [11]. Maintenance with low-dose fluorometholone beyond the high-risk period further reduces rejection risk [11]. Despite effective management, the patient developed cataract, a known complication of PK and prolonged steroid use, reported in 24-60% of cases [12]. Intraocular pressure (IOP) management also posed challenges. Initially treated with acetazolamide to control IOP, the patient later exhibited hypotony (IOP 9.2 mmHg), likely due to increased aqueous outflow post-PK [13]. Visual acuity improved from hand movement to 6/24 at five months, though it decreased to 6/40 at seven months due to cataract progression. Astigmatism measurements (R1 38.73 mm, R2 42.12 mm) highlight refractive challenges common after PK, influenced by suture techniques, wound healing, and donor-recipient disparities [14]. These findings emphasise the importance of personalised postoperative care to optimise refractive and visual outcomes.
Conclusion
This case demonstrates that periosteal grafts effectively preserve ocular structure in corneal perforations when donor tissue is unavailable, enabling subsequent definitive visual rehabilitation with PK. Despite a three-year delay before keratoplasty, the patient achieved substantial visual improvement. Planned cataract extraction with IOL implantation is expected to further enhance outcomes. Overall, this case emphasizes the value of periosteal grafts as a temporising measure and the importance of comprehensive, tailored postoperative management to maximise long-term vision restoration.
Contributors: CPS: manuscript writing, patient management; DI: manuscript editing, patient management. DI will act as a study guarantor. Both authors approved the final version of this manuscript and are responsible for all aspects of this study. Funding: None; Competing interests: None stated.
References - Mohan M, Natarajan R, Kaur K, Gurnani B. Clinical approach to corneal ulcers. TNOA Journal of Ophthalmic Science and Research. 2023;61(4):386-395.
- Stamate AC, Tataru CP, Zemba M. Update on surgical management of corneal ulceration and perforation. Rom J Ophthalmol. 2019;63(2):166-173.
- Samira N, Bani AP, Susiyanti M. Rare case of bilateral perforated corneal ulcer due to gonococcal infection, managed with temporary periosteal graft. BMJ Case Rep. 2016 Feb 23;2016:bcr2015213547.
- Qureshi S, Dohlman TH. Penetrating Keratoplasty: Indications and Graft Survival by Geographic Region. Vol. 38, Seminars in Ophthalmology. Taylor and Francis Ltd.; 2023. pp. 31-43.
- Anshu A, Li L, Htoon HM, de Benito-Llopis L, Shuang LS, Singh MJ, et al. Long-term review of penetrating keratoplasty: A 20-year review in Asian eyes. Am J Ophthalmol. 2021;224:254-266.
- Krysik K, Wroblewska-Czajka E, Lyssek-Boron A, Wylegala EA, Dobrowolski D. Total penetrating keratoplasty: Indications, therapeutic approach, and long-term follow-up. J Ophthalmol. 2018;2018:9580292.
- Grzybowski A, Magdalena T, Schwartz SG, Relhan N, Flynn Jr HW. The role of systemic antimicrobials in the treatment of endophthalmitis: A review and an international perspective. Ophthalmol Ther. 2020;9(3):485-498.
- Fan C, Yang B, Huang Y. Efficacy of 0.5% Levofloxacin and 5.0% Povidone-Iodine eyedrops in reducing conjunctival bacterial flora: Metagenomic analysis. J Ophthalmol. 2020;2020:1780498.
- Szaflik JP, Major J, Izdebska J, Lao M, Szaflik J. Systemic immunosuppression with mycophenolate mofetil to prevent corneal graft rejection after high-risk penetrating keratoplasty: a 2-year follow-up study. Graefe’s Archive for Clinical and Experimental Ophthalmology. 2016;254(2):307-314.
- Azevedo Magalhaes O, Shalaby Bardan A, Zarei-Ghanavati M, Liu C. Literature review and suggested protocol for prevention and treatment of corneal graft rejection. Eye (Basingstoke). 2020;34:442-450.
- Qi X, Wang L, Zhang X, Liu M, Gao H. Topical administration of tacrolimus and corticosteroids in tapering doses is effective in preventing immune rejection in high-risk keratoplasty: a 5-year follow-up study. BMC Ophthalmol. 2022;22:101.
- Tang Q, Yao K. Challenges in cataract surgery after penetrating keratoplasty managed using femtosecond laser A series of 3 case reports. Medicine (United States). 2024;103(25):e38614.
- A Owaidhah O. Cornea Transplantation-Induced Glaucoma: A Review of Glaucoma Secondary to PKP, DMEK, and DSAEK Procedures. EyeWiki. 2024 Mar 14. Available from: https://eyewiki.org/Cornea_Transplantation-Induced_Glaucoma:_A_Review_of_Glaucoma_Secondary_to_PKP,_DMEK,_and_DSAEK_Procedures. Accessed December 27, 2024.
- Bhayani R, Walkden A. Managing Post Keratoplasty astigmatism. Clinical Ophthalmology. 2024;18:1727-1734.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
Samira CP, Islami DSuccessful Management of Corneal Perforation Following Keratoplasty with Emergency Periosteal Grafting.JCR 2025;15:53-56 |
|
Samira CP, Islami DSuccessful Management of Corneal Perforation Following Keratoplasty with Emergency Periosteal Grafting.JCR [serial online] 2025[cited 2026 Feb 16];15:53-56. Available from: http://www.casereports.in/articles/15/3/Successful-Management-of-Corneal-Perforation-Following-Keratoplasty-with-Emergency-Periosteal-Grafting.html |

|
|
|
|
|