|
|
|
|
|
Recurrent Childhood Abdominoperineal Malignant Fibrous Histiocytoma
|
|
|
citalopram and alcohol reddit citalopram alcohol cravings
From the Department Of Surgery and Histopathology1, University of Maiduguri Teaching Hospital Maiduguri, Borno State, Nigeria. |
|
|
|
|
|
Corresponding Author:
|
Dr. Usman Mohammed Tela
Email: umtela@yahoo.com |
|
|
|
|
|
|
|
|
Received:
07-SEP-2012 |
Accepted:
28-SEP-2012 |
Published Online:
30-SEP-2012 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
Malignant fibrous histiocytoma (MFH) is a rare soft tissue tumour that arises from primitive mesenchymal tissue in children. We present MFH that started during infancy presenting later with giant abdominoperineal lesion with multiple recurrences but remains disease free after 10 years of last curative excision. This case demonstrated that MFH follows less aggressive course in children and adequate surgical resection can be curative even in recurrent disease.
|
|
|
|
|
|
Keywords :
|
Abdominoperineal, Childhood, Recurrent, Malignant fibrous histiocytoma.
|
|
|
|
|
|
|
|
|
|
|
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff34ba01000000b500000001001100 6go6ckt5b5idvals|145 6go6ckt5b5idcol1|ID 6go6ckt5b5|2000F757Tab_Articles|Fulltext Malignant fibrous histiocytoma (MFH) is a soft tissue tumour that arises from primitive mesenchymal tissue in children. It usually consists of fibroblastic and histiocytic elements in storiform pattern. This sarcoma was first described by Ozzello et al in 1963 as malignant histiocytoma and fibrous xanthoma [1]. Soft tissue sarcomas are generally rare tumour in both children and adult contributing to 7% and 1% of all malignancies respectively [2,3]. MFH though one of the commonest soft tissue sarcoma in adult is extremely rare in children [4,5]. We present this patient with giant abdominoperineal MFH with no recurrence after 10 years following wide local excision.
Case Report
Our patient is a 21 years old young male who developed a small nodule in the right groin at the age of 3 months. The swelling gradually increased in size and remain asymptomatic until at eight years of age when it spontaneously ulcerated with rapid increase in size. There was associated purulent discharge and pain. He underwent excision in a peripheral hospital which was followed by recurrence after seven months. The initial histology was not available for review. The tumour recurred after 2 further excisions in the same hospital. He was then referred to our hospital with grotesque weeping mass over the lower abdomen and perineum.
General physical examination revealed a non-emaciated boy with pallor and fever. Abdominoperineal examination revealed a huge fungating ulcerated mass over the lower abdomen, root of the penis and scrotum measuring about 30x23x15 cm and discharging foul smelling purulent fluid [Fig. 1]. No clinical features of systemic metastases were present.

Fig.1: Preoperative tumor involving abdominoperineal region.
The wound cultured Staphylococcus aureus and Pseudomonas aeroginosa which was treated with sensitive antibiotics. Histology revealed malignant fibroblastic and histiocytic cells in fascicles and vaguely storiform pattern with hypocellular and myxoid background [Fig. 2]. Infiltration of skin with malignant cells was present. Histological diagnosis of malignant fibrous histiocytoma, myxoid variant was made. Chest radiograph and abdominal ultrasound examination were essentially normal.
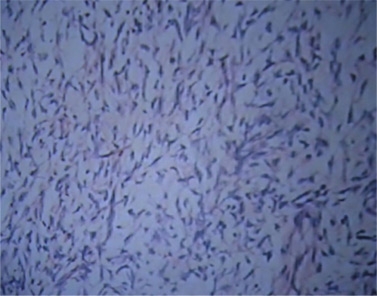
Fig.2: Photomicrograph of Malignant Fibrous histiocytoma (Myxoid variant) [H & E × 128].
He had wide local excision with 5 cm margin including total scrotal excision. Split thickness skin graft was used to resurface parts of the wound. Exposed testes were buried in pockets created in the medial aspect of both thighs. He had recurrence free 10 years follow up period [Fig. 3 and 4]. He is now requesting for scrotal reconstruction. Recent seminal fluid analysis, chest radiograph and abdominopelvic ultrasound examinations revealed normal parameters.

Fig.3: Ten years post excision.

Fig.4: Perineum 10 years post excision.
Discussion
Malignant fibrous histiocytoma arises from connective tissue in integuments, bones and viscera in any part of the body but is more commonly seen in the extremities. Different sites have been reported in children, which includes kidneys, lungs, intestine, spleen, bone and fascia [6]. MFH is more common in whites than blacks with high preponderance of male over female [5,7].
The aetiology of this tumour like other sarcomas is unknown but genetic mutations in pluripotent mesenchymal stem cells of children are believed to give rise to malignant clones [8]. Mutation in tumour suppressor genes like p53 and RB1 are also implicated [8]. Most of the patients have sporadic disease but some inherited conditions like Li Fraumeni cancer susceptible syndrome and neurofibromatosis type 1 are associated with high chances of developing sarcomas. MFH may arise from burn scars, trauma, and chronic inflammation and irradiated part of the body [9,10]. MFH is one of the commonest radiation induced sarcoma [10,11] Our patient had primary MFH which has less aggressive behaviour compared to the secondary tumour.
Histologically, MFH is divided into 5 morphological subtypes which includes: storiform-pleomorphic, myxoid, angiomatoid, giant cell and inflammatory variants[12,13]. Angiomatoid subtype is the commonest form in children but the index case had myxoid variant. Both myxoid and angiomatiod are less aggressive compared to storiform polymorphic and inflammatory variant [13]. Angiomatoid MFH has an almost invariably benign behaviour [7].
In children MFH commonly presents as slow growing painless mass as seen in the initial presentation of the index case. Pain may result from ulceration, infection and neural invasion. Inflammatory type can mimic an abscess with features of inflammation and several attempts at drainage may be made before the diagnosis is finally uncovered [14]. The index patient presented with giant ulcerated fungating mass involving the lower abdomen, root of the penis and scrotum. Those with bony involvement may present with pathological fractures. The features of pulmonary metastasis are evident in only 1% of patients [7].
Wide local excision with curative intent still remains the best form of treatment as shown in this case [4,5,13]. The location of the tumour may occasionally limit radical excision. In our case, the abdominoperineal location and the size of the lesion presented a unique challenge that warranted the total excision of the scrotum and part of penile skin. At least a margin of 5 cm in such cases is required for complete excision. Recurrence after surgery is high especially if the margin is not free of microscopic tumour. The high recurrence rate is due to growth along fascial plane and pseudocapsule formation. The index case had three recurrences before the last excision 10 years ago and remained disease free thereafter. The planned scrotal reconstruction was not done because the patient was not regular on follow up until recently. After burying the testis in medial thigh pockets for ten years, recent seminal fluid analysis still revealed normal parameters. This shows that when expertise for scrotal reconstruction is not available, medial thigh pocket is a safe site to preserve exposed testis.
Chemotherapy and radiotherapy should be used for high grade and recurrent tumour. Chemotherapy has been shown to be effective in margin positive and unresectable tumour [15,16]. High grade sarcomas with minimal tumour bulking are more sensitive to radiotherapy whereas low grade sarcomas are more resistant to radiotherapy [17]. Our patient was successfully treated with only surgery despite his multiple recurrences. Recent therapy targets angiogenesis and vasculogenesis. Till date the effect of antiangiogenic factors is not particularly striking [2].
Poor prognosis is associated with deeply sited tumours, tumour size >5cm, involvement of viscera, storiform-pleomorphic subtype and recurrence [5]. Estimated overall 5 year survival rate in children in one study was 75% [4]. MFH spreads mainly via haematogenous route with metastatic rate of 1% in angiomatoid and myxoid variant [7,11]. The lung is the commonest site of metastasis. Primary tumour of the lung is frequently fatal [16]. Because of the rarity of MFH in children no significant data in the literature on long term outcome is available.
In conclusion, malignant fibrous histiocytoma follows less aggressive course in children. Cure can be achieved in this subset of patients with margin negative surgical resection with or without adjuvant therapy. Long term follow up is required to ensure cure.
Consent
Documented consent was obtained from the patient for publication of this case report and figures.
References
- Ozzello L, Stout AP, Murray MR. Cultural characteristics of malignant histiocytomas and fibrous xantomas. Cancer. 1963; 16:331-344.
- Bid HK, Houghton PJ. Targeting angiogenesis in childhood sarcomas. Sarcoma. 2011;601-614.
- Rouhani P, Fletcher CD, Devesa SS, Toro JR. Cutaneous soft tissue sarcoma incidence patterns in U.S. : an analysis of 12,114 cases. Cancer 2008; 113(3):616-627.
- Corpron CA, Black CT, Raney RB, Pollock RE, Lally KP, Andrassy RJ. Malignant fibrous histiocytoma in children. J Pediatr Surg. 1996; 31(8):1080-1083.
- Cole CH, Magee JF, Gianoulis M, Rogers PC. Malignant fibrous histiocytoma in childhood. Cancer. 1993; 4077-4083.
- Koseoglu V, Kurekci AE, Kul M, Ozturk H, Gunhan O et al. Malignant fibrous histiocytoma in a child. A case report and review of literature. Turk J Pediatr. 2000; 42(1):72-75.
- Fanburg-Smith JC, Miettinen M. Angiomatoid “malignant fibrous histiocytoma”; a clinicopathologic study of 158 cases and further exploration of the myoid phenotype. Hum Pathol. 1999; 30(11):13336-13343.
- Kotilingam D, Lev DC, Lazar AJ, Pollock RE. Staging soft tissue sarcomas; Evaluation and changes. Cancer J Clin. 2006; 56:282-291.
- Yucel A, Yazar S, Demirkesen C, Durak H, Dervisoglu S, Altintas, M. An unusual long term complication of burn injury: malignant fibrous histiocytoma developing in chronic burns scar. Burns. 2000; 26(3):305-310.
- Cha C, Antonescu CR, Quan ML, Maru S, Brennan MF. Long term results with resection of radiation induced soft tissue sarcomas. Ann Surg. 2004; 239(6):903-910.
- Park K, van Rijn R, McHugh K. The role of radiology in paediatric soft tissue sarcomas. Cancer Imaging. 2008; 8(1):102-115.
- Pobirci DD, Bogdan FL, Pobirci O, Petcu CA, Rosca E. Study of malignant fibrous histiocytoma: Clinical statistics and histopathological interrelation. Rom J Morphol Embryol. 2011; 52(1): 385-388.
- Joshi H, Rayappa CS. Malignant fibrous histiocytoma of the mandible and infratemporal fossa. A case report. Int J Surg Case Rep. 2011; 2(6):134-137.
- Liarmakopoulos E, Lampropoulos P, Markakis C, Manoloudaki K, Manoloudaki K, Chatzimarkou A et al. Soft tissue parasternal inflammatory malignant fibrous histiocytoma presenting as a lumbar abscess. Case Rep Oncol. 2011; 4(2):342-349.
- Caglar K, Gungor S, Akansoy S, Sakalli U, Orhan D, Caglar M. Successful treatment of retroperitoneal giant cell type malignant fibrous histiocytoma in a 5 year old boy. Turk J Pediatr. 2007; 49(3):307-311.
- Shah SJ, Craver RD, Yu LC. Primary malignant fibrous histiocytoma in a child: a case report and review of literature. Padiatr Hematol Oncol. 1996;13(6):531-538.
- Donaldson SS. The value of adjuvant chemotherapy in the management of sarcomas in children. Cancer. 1985;55(9):2184-2197.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
UM Tela, BM Ibrahim, MB Tahir, HA NggadaRecurrent Childhood Abdominoperineal Malignant Fibrous Histiocytoma.JCR 2012;2:63-66 |
|
UM Tela, BM Ibrahim, MB Tahir, HA NggadaRecurrent Childhood Abdominoperineal Malignant Fibrous Histiocytoma.JCR [serial online] 2012[cited 2024 Apr 20];2:63-66. Available from: http://www.casereports.in/articles/2/2/recurrent-childhood.html |

|
|
|
|
|