|
|
|
|
|
Dermatomyositis Presenting with Erythroderma
|
|
|
Sameer Saraf, Mohit Mohan Singh
From the Department of Medicine, King George’s Medical University, Lucknow, Uttar Pradesh, India. |
|
|
|
|
|
Corresponding Author:
|
Dr. Sameer Saraf
Email: drsameersaraf@gmail.com |
|
|
|
|
|
|
|
|
Received:
12-JAN-2013 |
Accepted:
24-FEB-2013 |
Published Online:
20-MAR-2013 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
Dermatomyositis is a common autoimmune disorder classified as idiopathic inflammatory myopathy. This predominantly affects the adults and is characterized by both cutaneous and muscle involvement. The characteristic cutaneous feature of this condition includes photosensitivity and the presence of heliotrope erythema and Gottron’s patches. A number of uncommon cutaneous manifestations have been reported worldwide. We report a case of dermatomyositis presenting as erythroderma. |
|
|
|
|
|
Keywords :
|
Dermatomyositis, Autoimmune Diseases, Erythema, Photosensivity Disorders, Myositis.
|
|
|
|
|
|
|
|
|
|
|
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff94a402000000ba01000001000a00 6go6ckt5b5idvals|186 6go6ckt5b5idcol1|ID 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
Dermatomyositis is a common autoimmune disorder classified as idiopathic inflammatory myopathy. This predominantly affects the adults and is characterized by both cutaneous and muscle involvement [1]. The characteristic cutaneous feature of this condition includes photosensitivity and the presence of heliotrope erythema and Gottron’s patches [2]. A number of uncommon cutaneous manifestations have been reported worldwide. We report a male patient who developed generalized erythroderma with diffuse hyperpigmentation and thickening of skin who had not received proper treatment for the disease. Very few case reports are available in the literature from all over the world and rare reports are available from India.
Case Report
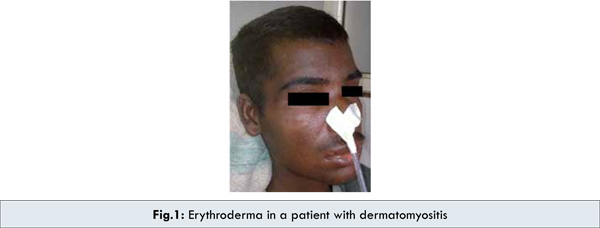
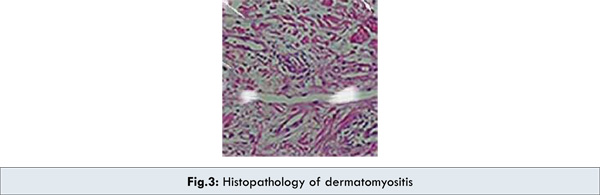
A 21 year old male presented with generalized bodyache and low grade pyrexia along with progressive, predominantly proximal weakness of all limbs for 10 months. He also complained of difficulty in swallowing and generalized rashes with diffuse hyperpigmentation for six months. There was no history of any prolonged over the counter or prescription drug intake. On examination the vitals were stable and there was diffuse hyperpigmentation with focal hypopigmented patches over lips and lower extremities with generalized erythematous rashes with skin thickening [Fig.1,2]. He was conscious, higher mental functions and cranial nerves were intact. Motor examination revealed predominantly proximal weakness of grade 1 and 3 in upper and lower limbs respectively. There was no wasting of muscles. The contracture was noted at left elbow joint. All modalities of sensations were intact. Routine haemogram revealed hemoglobin of 6.9 gm% and Erythrocyte Sedimentation Rate (Westergren) of 110 mm in 1st hour. Total serum creatine kinase was 4500 U/L (39-308). Thyroid function tests were within normal limits. Anti-centromere antibody was negative. Upper GI Endoscopy was uninformative. Biopsy from the involved skin on the dorsal aspect of the right forearm revealed hyperkeratosis, thickened basement membrane, vacuolar degeneration of basal keratinocytes, with fibrosis of the stroma and mild infiltration of chronic inflammatory cells [Fig. 3]. There was no evidence of granuloma, atypical cells or inclusion bodies. Direct immunofluorescence microscopy was negative. The electrodiagnostic studies revealed increased spontaneous activity with high frequency low amplitude polyphasic potentials. The above findings were compatible with chronic myositis changes as in dermatomyositis [3]. The patient showed remarkable improvement in symptoms on oral corticosteroids (prednisolone 60 mg once daily). At one month follow up his bodyache and dysphagia improved and erythematous rashes partially subsided. The dose of steroids was gradually tapered and he is currently maintained at 10 mg daily dose of oral steroids.

Discussion
Dermatomyositis is a connective tissue disorder, characterized by cutaneous and muscle involvement. The pathognomic cutaneous manifestations of dermatomyositis include Gottron’s papule and Gottron’ sign [2]. The characteristic cutaneous features are heliotrope erythema, periungual telangiectasia, shawl sign, V sign, and mechanic’s hand lesion [4]. Other features include poikiloderma, malar erythema, and photosensitivity. A number of rare cutaneous manifestations have been reported in patients with dermatomyositis, including acquired ichthyosis; anasarca; erythroderma; facial swelling without erythema; follicular hyperkeratosis; hypertrichosis; lichen planus; lipodystrophy; malakoplakia; cutaneous mucinosis; mucous membrane lesions; nasal septal perforation; panniculitis; perforating skin ulcers; pityriasis rubra; pyoderma gangrenosum; steroid induced acanthosis nigricans; urticaria; cutaneous vasculitis; vesicular and bullous lesions; vulvar changes and scrotal involvement; and zebra like stripes (centripetal flagellate erythema) [5].
We reported a male patient who developed generalized erythroderma with diffuse hyperpigmentation and thickening of skin who had not received proper treatment for the disease. Very few case reports are available in the literature from all over the world and rare reports are available from India. [6]
Systemic corticosteroids are the main stay of therapy and are the first line treatment in patients with dermatomyositis [7]. The earlier the therapy with corticosteroids, the better is the overall prognosis. Our patient responded to steroids therapy (prednisolone 60 mg once daily). Hydroxychloroquine sulfate, and antimalarials can also be used to treat dermatomyositis [8]. Rarely, antimalarials can contribute to muscle weakness by causing a vacuolar myopathy.
Conclusion
Our experience with this case demonstrates that dermatomyositis must be considered in a patient presenting with erythroderma. Cutaneous lesion may precede, occur simultaneously, or occur after the diagnosis of dermatomyositis.
References
- Euwer RL, Sontheimer RD. Dermatomyositis. In: Sontheimer RD, Provost TT, (eds) Cutaneous Manifestations of Rheumatic Diseases. 2nd ed. Philadelphia : Lippincott Williams & Wilkins, , 2004; pp. 79-81.
- Louthrenoo W, Kasitanon N, Mahanuphab P, Bhoopat L, Thongprasert S. Kaposi’s sarcoma in rheumatic disease. Semin Arthritis Rheum. 2003;32:326-333.
- Bohan A, Peter JB . Polymyositis and dermatomyositis (first of two parts). N Engl J Med. 1975;292:344-347.
- Healy CM, Tobin AM, Kirby B, Flint SR. Oral lesions as an initial manifestation of dermatomyositis with occult malignancy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:184-187.
- Tomb R, Stephan F. Perforating skin ulcers occurring in an adult with dermatomyositis. Ann Dermatol Venereol. 2002;129:1383-1385.
- Chander R, Gupta T, Rani S, Nagia A. Erythrodermic Juvenile Dermatomyositis. Pediatric Dermatology. 2009;26:234–235.
- Chen GY, Liu MF, Lee JY, Chen W. Combination of massive mucinosis, dermatomyositis, pyoderma gangrenosum-like ulcer, bullae and fatal intestinal vasculopathy in a young female. Eur J Dermatol. 2005t;15:396-400.
- Ang GC, Werth VP. Combination antimalarials in the treatment of cutaneous dermatomyositis: a retrospective study. Arch Dermatol. 2005;141:855-859.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
Saraf S, Singh MMDermatomyositis Presenting with Erythroderma.JCR 2013;3:92-95 |
|
Saraf S, Singh MMDermatomyositis Presenting with Erythroderma.JCR [serial online] 2013[cited 2025 Dec 14];3:92-95. Available from: http://www.casereports.in/articles/3/1/dermatomyositis-presenting-with-erythroderma.html |

|
|
|
|
|