6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ffb4ec030000002002000001000100
6go6ckt5b5idvals|240
6go6ckt5b5idcol1|ID
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Introduction
Lymph nodes in parotid region are divided into extraglandular and intraglandular [
1,
2]. These in turn drain into the deep cervical nodes. The intra parotid lymph nodes, places the parotid gland at risk for nodal metastasis from various sites. Metastatic disease to the parotid gland is uncommon, and when present it usually arises from a primary in the head and neck or less commonly from an infraclavicular primary (kidney, prostrate, lung, breast, gastro-intestinal) [
3]. The intraparotid nodes could be involved by either direct extension of disease from the adjacent structures (eg: external auditory canal) or by either lymphatic/ haematogenous spread. Metastatic disease to the parotid nodes is mostly caused by squamous cell carcinoma(SCC, but other histologies like adenocarcinoma, have also been described [
2]. Hence, in this case report we would like to highlight this rare clinical presentation and review the literature on intraparotid nodal metastasis from OSCC.
Case Report
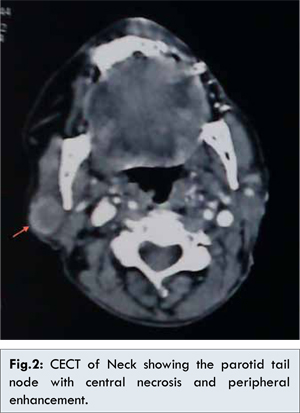
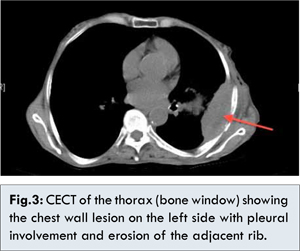
Our patient was a 67 year old female who initially presented with growth in the left side oral cavity for 1 month duration. She had no family history of cancer or history of using any form of tobacco. She was a known case of hypothyroidism on treatment. Oral cavity examination showed an ulcero-proliferative growth involving the left buccal mucosa measuring approximately 3x3 cms extending close to the oral commisure, upper gingivo-buccal sulcus (GBS). The external skin adjacent to the tumor was indurated and appeared congested. The retro-molar trigone, floor of the mouth, lower GBS were free of disease. There were no co-existing oral submucosal fibrosis or leukoplakia and no palpable neck nodes. Biopsy of the growth confirmed the diagnosis of SCC. Contrast enhanced computed tomography (CECT) showed no erosion of the mandible or nodal disease. With the above finding patient was staged as IVA disease (cT4aN0M0, in view of the skin involvement). The patient underwent wide excision of buccal mucosa lesion (along with the skin adjoining the lesion) with selective neck dissection (Levels I-IV). The buccal mucosa defect was reconstructed with free radial artery forearm flap (FRAFF), harvested from the left forearm. Histopathology reported a moderately differentiated squamous cell carcinoma (MDSCC) of the left buccal mucosa, tumor size being 3x2.5 cms, and thickness of 1.2 cms. The skin was involved, and perineural involvement noticed. 4 out of the 26 nodes had metastatic disease with extra-capsular spread (ECS) (pT4aN2bM0). Based on the pathological stage the patient was advised for adjuvant concurrent chemoradiotherapy. She received 60Gy/30 fractions radiotherapy (left side face and neck,60Co ?-rays), with grade II skin and mucosal toxicity, without any treatment break. She did not receive chemotherapy as planned in view of infection of the FRAFF donor site. After completing adjuvant treatment she was kept on regular follow up at two monthly intervals. On her second follow up she presented with swelling on the right side, parotid tail region [Fig.1] (disease free interval{DFI} of 3 and ½ months). There was no lesion on intra oral examination, or nodal disease in the other stations of the neck on both sides of the neck. Fine needle aspiration (FNA) of the swelling reported as metastatic squamous cell carcinoma. CECT of the neck and PNS revealed a right side intraparotid (tail) node [Fig.2], with no disease in the oral cavity or lymphadenopathy elsewhere. A distant metastasis work-up revealed none. Total parotidectomy and modified neck dissection on the right side was performed. The postoperative period was uneventful. The final histopathology showed a poorly differentiated squamous cell carcinoma (PDSCC) in the parotid nodes with the remaining nodes being unremarkable except for some epitheloid granulomas negative for Ziehl-Neelsen (ZN) stain. As the patient received radiotherapy on the left side of the neck alone for her index lesion, she was offered radiotherapy for the right side of the neck covering the right parotid bed. She completed 54Gy/27 fractions radiotherapy (6mV photon Tomotherapy). During follow-up patient developed left sided chest pain intractable to routine analgesics. PET-CT was advised to rule out distant metastasis. PET-CT showed a chest wall lesion on the left side eroding into the adjacent rib, along with hilar nodes. A CT-guided fine needle aspiration (FNA) of this lesion showed pleural involvement by PDSCC (DFI-16 months). There were no other lesions elsewhere in the body. Based on this finding and her poor general condition she was offered palliative RT to the chest wall to reduce pain along with best supportive care.

Discussion
Development of parotid glands starts during sixth week of gestation as outpouchings from the oropharyngeal ectoderm. During this period, regional mesoderm gives rise to the lymphatic system of the head and neck. These lymphatic tissues get embedded within the parotid fascia and substance of the parotid tissue, as the encapsulation of the parotid gland occurs late during development[
4].The parotid nodes are about 15-20 in number, scattered in (intraglandular) and around the gland within the parotid fascia (extraglandular). The extraglandular nodes lie over the superficial aspect of the parotid gland (pre-auricular) and adjacent to the retromandibular vein in the lower pole of the gland (infra-auricular). The intraglandular node is predominantly within the substance of the gland spread in both the superficial and deep lobes [
5].Haagensen [
5] and Harada et al [
6] described that it is possible for the buccal mucosa to drain directly to parotid (infra-auricular) node. The first nodal station for drainage from oral cavity is to levels I-III, second drainage station being the parotid nodes and levels IV-V. SCC of the UADT with parotid metastasis most often arises from the oral cavity. There are very few studies (small case series with few patients) in literature mentioning these findings [
3,
6,
7]. Parotid node metastasis may develop initially during presentation of the index cancer or may develop as delayed metastasis subsequent to the treatment of this index cancer.
Metastasis to the parotid node commonly is from the cutaneous malignancies of the head and neck. In upto 2.5% of OSCC patients the ipsilateral side parotid nodes are involved, when there are nodal metastases at other nodal stations [
6]. In the study by Oslen et al [
7] they showed that parotid metastasis predominantly developed as recurrent, rather than initial, disease. Harada, et al [6] showed that the incidence of parotid node metastasis in HNSCC was 4.0% overall, and 2.9% for oral SCC. The parotid metastases from oral cancer occurs more commonly after normal cervical lymphatic flow has been disrupted by the previous treatment, especially in the form of surgery [
8]. Alternatively, these nodal metastases may have been present as unrecognized microscopic metastasis at the time of initial tumor presentation. Ord et al.[
9] reported 2 cases of parotid gland recurrences from previously treated oral cavity SCC. But in our case, the patient developed a delayed parotid nodal metastasis on the opposite side of the index cancer. After a through work-up to rule out another primary and distant metastasis, we realized that this was indeed a case of delayed parotid nodal disease on the contralateral side, without involvement of other nodal stations on either side of the neck. To the best of our knowledge, a through literature search in this regard revealed no study or a case report of a similar nature, though there are case series of parotid nodal disease on the ipsilateral side. This case report and the various case series, suggests the importance of a careful clinical and radiographic evaluation of the parotid region while examining patients with UADT SCC, especially oral cavity malignancies when presenting initially with nodal disease.
When a neck dissection is performed as part of the treatment for the above subset of patients a thorough examination of the parotid should be done on table to look for any nodal disease, especially the parotid tail. Though resection of part of the parotid as part of the neck dissection routinely has been described, its justification and how much of the tail parotid should be removed has not been adequately explained in the literature. Harda, et al have described the extent and method of tail parotid resection. In general they have recommended removing the parotid gland below the marginal mandibular branch of the facial nerve [
6]. If any suspicious nodes are seen or felt in the parotid tail they must be removed. At least superficial parotidectomy or preferably a facial nerve preserving total parotidectomy must be performed, whenever a metastatic parotid node is identified [
7,
10].
Conclusions
UADT SCC, especially of the oral cavity, tend to metastasize to the parotid nodes (infra-auricular nodes), particularly in node positive neck. Hence, it is pertinent to examine the parotid region also for nodal disease and treat them appropriately. Delayed nodal metastasis to the contralateral tail parotid has not been reported prior to this report to the best of our knowledge, hence highlighting the possibility of this clinical situation.
References
- Batsakis JG. Pathology consultation. Parotid gland and its lymph nodes as metastatic sites. Ann. Otol. Rhinol. Laryngol. 1983;92:209–210.
- Conley J, Arena S. Parotid gland as a focus of metastasis. Arch. Surg. Chic. Ill 1960. 1963;87:757–764.
- Pisani P, Krengli M, Ramponi A, Guglielmetti R, Pia F. Metastases to parotid gland from cancers of the upper airway and digestive tract. Br J Oral Maxillofac. Surg. 1998;36:54–57.
- Nuyens M, Schüpbach J, Stauffer E, Zbären P. Metastatic disease to the parotid gland. Otolaryngol. Head Neck Surg.2006;135:844–848.
- Haagensen C. The lymphatics in cancer. 1st ed. Philadelphia: W.B. Saunders; 1972.
- Harada H, Omura K. Metastasis of oral cancer to the parotid node. Eur. J. Surg. Oncol. 2009;35:890–894.
- Olsen SM, Moore EJ, Koch CA, Kasperbauer JL, Olsen KD. Oral cavity and oropharynx squamous cell carcinoma with metastasis to the parotid lymph nodes. Oral Oncol. 2011;47:142–144.
- Fisch UP. Cervical lymph flow in man following radiation and surgery. Trans. - Am. Acad. Ophthalmol. Otolaryngol. 1965;69:846–868.
- Ord RA, Ward-Booth RP, Avery BS. Parotid lymph node metastases from primary intra-oral squamous carcinomas. Int. J. Oral Maxillofac. Surg. 1989;18:104–106.
- Pisani P, Ramponi A, Pia F. The deep parotid lymph nodes: an anatomical and oncological study. J. Laryngol. Otol. 1996;110:148–150.