|
|
|
|
|
Effective Pacing Therapy for Syncope with Severe Orthostatic Hypotension and Chronotropic Incompetence
|
|
|
|
Tadashi Hashida, Koichiro Yoshioka1, Yuji Ikari1
From the Department of Cardiology, Tokai University Tokyo Hospital, Tokyo, Japan and Department of Cardiology1, Tokai University School of Medicine, Kanagawa, Japan. |
|
|
|
|
|
Corresponding Author:
|
|
Dr. Tadashi Hashida
Email: hashida@is.icc.u-tokai.ac.jp |
|
|
|
|
|
|
|
|
Received:
9 AUG 2013 |
Accepted:
16-SEP-2013 |
Published Online:
30-SEP-2013 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
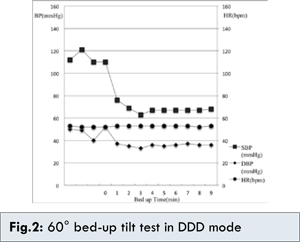
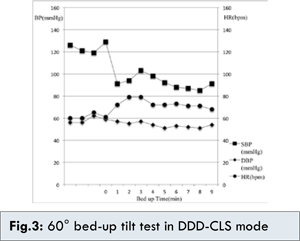
Orthostatic hypotension (OH) occurs during body posture changes from supine to standing within few minutes. There have been several reports that pacemaker therapy improved the symptoms of drug refractory OH. An 83 year old male patient presented to us with recurrent syncopal episodes. The patient was having drug-refractory OH and sinus bradycardia with chronotropic incompetence. TheProtos DR/CLS (Biotronik, Germany) cardiac pacemaker was implanted. This pacemaker has a rate response function of closed loop stimulation (CLS). The CLS function continuously monitors cardiac contraction dynamics through intracardiac local electrical impedance measurement via a ventricular pacing lead, and translates the cardiac contraction dynamics into its pacing rates. We evaluated the effectiveness of the DDD-CLS pacing for the change of his blood pressure (BP) and heart rate (HR) during tilt test comparing to DDD mode. In the DDD mode, after tilt test, the patient’s HR was hold in 46 bpm, and systolic BP was dropped from 110 mmHg to 67 mmHg. The patient developed symptoms of pre-syncope during postural changes. In the DDD-CLS mode, a systolic BP dropped from 129 mmHg to 91 mmHg after tilting, but at almost same time, pacing HR was increased 18 ppm, from 61 ppm to 79 ppm, and the systolic BP was increased to 103 mmHg in 3 minutes. Thereafter, pacing rate was gradually decreased to 65 ppm and systolic BP was maintained at around 95 mmHg. Syncopal recurrence was not exhibited during postural changes setting to the DDD-CLS mode. The rate response function of CLS mode could be suppressed OH patient’s syncopal episode with chronotropic incompetence and improve quality of life of the patient suffering from OH. |
|
|
|
|
|
Keywords :
|
Arrhythmias, Orthostatic Hypotension, Artificial Pacemaker, Syncope, Bradycardia.
|
|
|
|
|
|
|
|
|
|
|
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ffc813040000002c02000001000200 6go6ckt5b5idvals|248 6go6ckt5b5idcol1|ID 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
Orthostatic hypotension (OH) patient refractory to physical therapy and pharmacotherapy accompanies ordinary hypotension symptoms, and has a poor quality of life (QOL). OH is an independent predictor of 4-year all-cause mortality in elderly men [ 1]. In middle-aged individuals, presence of OH increases mortality and coronary event risk. Current recommended treatments for OH therapy are avoidance of rapidly standing up, adequate hydration and salt intake, usage of internal medicines, abdominal binders and/or support stockings, and head-up tilt sleeping [ 2]. During postural change from supine to standing, HR is increased to maintain blood pressure (BP) under the normal response. Severe OH patients with chronotropic incompetence have no adequate response of HR, when the BP falls during postural change. There have been a few reports of cardiac pacing therapy effectively providing good clinical result for drug-refractory OH [ 3- 6]. In the small group study, rate response pacing is effective to keep BP and HR during postural change for OH patients with chronotropic incompetence. Closed loop stimulation (CLS) function is one of rate response function and has been added to cardiac pacemakers. The CLS function continuously monitors cardiac contraction dynamics through intracardiac local electrical impedance measurement via a ventricular pacing lead. By direct assessment of variations in impedance, which reflect the ventricular wall motion in the close vicinity of the pacing electrode, the CLS function translates the cardiac contraction dynamics into its pacing rates [ 7]. We report a case in which syncopal episodes caused by refractory OH with chronotropic incompetence were successfully suppressed by DDD-CLS cardiac pacing therapy.
Case Report
The patient was an 83 year old male with wheelchair-dependent active daily life. Drug-refractory OH was diagnosed in our outpatient clinic so tablets of amezinium methylsulfate and fludrocortisone acetate had been orally administered and the progress of the symptoms was monitored, but the patient repeatedly had syncopal episodes while changing posture in bed or transferring into a wheelchair. This time, because he had a syncopal spell and loss of consciousness for a few minutes when transferring into a wheelchair, he was carried by ambulance to the emergency department of our hospital and admitted for the purpose of detailed examination of syncope. After hospitalization, progress was monitored with therapy of orally internal use of amezinium methylsulfate and fludrocortisone acetate tablets, wearing elastic stockings, and strictly observing abundant water consumption but the symptoms did not improve and he had recurrently developed syncopal episodes during postural change.
In the resting supine position, systolic and diastolic pressures were 110 and 66 mmHg, pulse rate 46 beats per minute, regular rhythm, and body temperature was 36.2°C. Physical inspection found no noteworthy findings. Blood count and biochemistry examinations did not reveal any clearly abnormal values. Catecholamine concentration in the blood had a normal value. TSH, FT3 and FT4 were within normal ranges. Chest X-ray examination showed no distinct abnormal findings. The surface 12 standard lead ECG depicted sinus bradycardia of heart rate 46 bpm and complete left bundle branch block. Ultrasonic echocardiography demonstrated good left ventricular wall motion, ejection fraction of 72% with no valvular disease or other abnormal findings in cardiac morphology. Doppler study on the neck ruled out stenosis in the carotid arteries. Head MRI Brain and Electroencephalography also gave no distinct findings of abnormality. Coronary angiography revealed no finding of significant stenosis. Electrophysiological study was conducted to evaluate sinus function. Basic heart rate was 48 bpm with sinus rhythm, no anomaly observed in atrioventricular conduction, and sinoatrial conduction time and sinus node recovery time as examined by atrial overdrive stimulation were normal.
During hospitalization, the patient recurrently developed syncopal spells in sitting position in bed every time while taking a meal. At the time of the episodes, systolic BP measured in the palpation method dropped to 60 mmHg and HR on a continuous ECG monitor remained constant at 46 bpm. We treated the patient with pacemaker therapy, because of Rubenstein type I sinus node dysfunction and OH with chronotropic incompetence. A pacemaker (Protos DR-CLS, Biotronik, Germany) was implanted. During the first 6 postoperative days the pacemaker was set to DDD mode and on the 7th postoperative day it was changed to DDD-CLS mode.
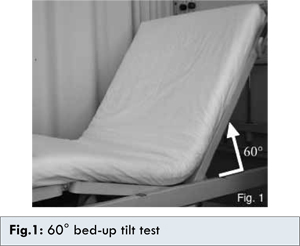
The standard head-up tilt test could not be implemented, because the patient could not keep standing by himself. Instead, posture was changed to elevate the head by putting the bed up and variations in heart rate were measured in a time series to assess syncopal symptoms. Hereafter, this will be referred to as bed-up tilt test. On the 10th postoperative day, the bed-up tilt test [Fig.1] was conducted with the conditions that the patient’s own HR were expected to be observed in the setting of DDD mode (basic pacing rate 40 ppm) and the paced rhythm was to be seen in DDD-CLS mode (basic pacing rate 60 ppm). In both conditions the variations in BP and HR were measured sequentially in order to evaluate syncopal symptoms.
We diagnosed the following symptoms as OH: when the posture was changed from supine position to sitting position, (i) systolic blood pressure dropped more than 20 mmHg within 3 minutes after sitting up, (ii) absolute value of systolic pressure dropped to 90 mmHg or less, or (iii) diastolic pressure dropped more than 10 mmHg. When intrinsic heart rate was seen in DDD mode, immediately after tilting the bed, systolic BP dropped from 110 to 67 mmHg and OH was observed [Fig.2]. Heart rate did not change before and after bed-up tilt and remained at an intrinsic rate of 52 bpm. Three minutes after the start of the bed-up tilt test, syncopal spell was seen. In DDD-CLS mode, systolic pressure dropped 38 mmHg, from 129 to 91 mmHg, after tilting the bed but at almost the same time, pacing rate increased 18 ppm, from 61 to 79 ppm, and the systolic BP, which had dropped to 91 mmHg, increased to 103 mmHg in 3 minutes [Fig.3]. Thereafter, pacing rate gradually decreased to 65 ppm and systolic BP was maintained at around 95 mmHg. After the bed-up tilt test, OH was observed but syncope was not observed.
Discussion
Prognosis of orthostatic hypotension (OH) depends on the underlying diseases and aging-related complications of diseases exacerbate the prognosis. It is believed that OH is an independent risk factor in causes of death and it correlates with degree of low BP. With aging, ischemic organic disorders accompanied by hypotension are prone to develop. Particularly, the mortality rate increases in OH cases. It has also been reported that development rate of stroke and ischemic heart diseases increases in OH cases [ 8, 9]. An effective therapy for drug-refractory OH has not been established. It has been reported that cardiac pacing improved the symptoms in drug-refractory patients with chronotropic incompetence [ 5]. This patient could not appropriately respond to fall the BP at the time of postural change so syncope or presyncopal state is exhibited. There have been some reports of attempting atrial-pacing therapy to increase heart rate and thereby increase cardiac output in order to improve hypotension in OH patients [ 3- 6]. A mechanism of OH improvement by atrial overdrive pacing has not been made clear. However, it has been reported that suppression of BP drop by atrial overdrive pacing was recognized and thereby improvement of QOL was observed. Moss AJ reported that they provided postural hypotension patients with atrial pacing at a rate of 100 ppm and after the follow-up period of 10 months they recognized significant improvement in symptoms of OH [ 10]. In this case, we used a cardiac pacemaker with CLS function and evaluated its effectiveness in treatment for OH. A pacemaker with CLS function feeds the local electrical impedance variations in the close vicinity of the ventricular pacing electrode back into its pacing rate. CLS function continuously monitors cardiac contraction dynamics by measuring the intracardiac local electrical impedance variations, which directly reflect the variations of ventricular wall motion in the close vicinity of the ventricular pacing lead tip electrode. It translates those inotropic signals into individual pacing rates. Therefore, CLS function can physiologically control its pacing rate via the pacemaker to adapt to the natural heart rate response demands. A drop of BP is stimulating the medullary circulatory center via the baroreceptors and therefore generates variations in inotropy in the myocardium and chronotropy in the sinus node to respond to the blood pressure drop. In patients with chronotropic incompetence responsiveness, this function of their own closed-loop feedback system fails and makes BP recovery difficult. A pacemaker with CLS function can be integrated into a failed cardiovascular system to re-establish the closed-loop circulation regulatory system. Therefore, the CLS function is considered to provide more appropriate and physiological cardiac pacing.
Conclusion
In a drug-refractory OH patient with chronotropic incompetence, the CLS function of the implanted pacemaker effectively suppressed syncope. Although OH was recognized, the heart rate increased swiftly, thereby recovering BP earlier and preventing syncope. After setting DDD-CLS mode, the syncope accompanying postural change improved with reproducibility and the patient’s ADL was increased, thereby markedly improving his QOL. A large-scale clinical study is needed to further verify the effectiveness of CLS in suppressing syncope.
References
- Masaki KH, Schatz IJ, Burchfiel CM, Sharp DS, Chiu D, Foley D, et al. OH predicts mortality in elderly men: The Honolulu Heart Program. Circulation. 1998; 98:2290– 2295.
- Moya A, Sutton R, Ammirati F, Blanc JJ, Brignole M, Dahm JB, et al. Guidelines for the diagnosis and management of syncope (version 2009): The Task Force for the Diagnosis and Management of Syncope of the European Society of Cardiology (ESC). European Heart Journal. 2009;30:2631-2671.
- Abe H, Numata T, Hanada H, Kohshi K, Nakashima Y. Successful treatment of severe OH with cardiac tachypacing in dual chamber pacemakers. Pacing Clin Electrophysiol. 2000;23:137-139.
- Kohno R, Abe H, Oginosawa Y, Nagatomo T, Otsuji Y. Effects of atrial tachypacingon symptoms and blood pressure in severe OH. Pacing ClinElectrophysiol. 2007; 30 Suppl 1:S203-206.
- Tse HF, Lau CP, Park E, Bornzin GA, Yu C, Benser ME, Bloomfield DM, Padeletti L. Transient overdrive pacing upon standing prevents OH in elderly pacemaker patients with chronotropic incompetence. Pacing Clin Electrophysiol. 2007;30:188-192.
- Grubb BP, Wolfe DA, Samoil D, Hahn H, Elliott L. Adaptive rate pacing controlled by right ventricular preejection interval for severe refractory OH. Pacing Clin Electrophysiol. 1993;16:801–805.
- Candinas R, Jakob M, Buckingham TA, Mattmann H, Amann FW. Vibration, acceleration, gravitation, and movement: activity controlled rate adaptive pacing during treadmill exercise testing and daily life activities. Pacing Clin Electrophysiol. 1997;20:1777–1786.
- Luukinen H, Koski K, Laippala P, et al. Prognosis of diastolic and systolic hypotension in older persons. Arch Intern Med. 1999;159:273-280.
- Eigenbrodt ML, Rose KM, Couper DJ, Arnett DK, Smith R, Jones D, et al. Orthostatic hypotension as a risk factor for stroke: the atherosclerosis risk in communities (ARIC) study, 1987-1996. Stroke. 2000; 31:2307-2313.
- Moss AJ, Warren Glaser, Eric Topol. Atrial Tachypacing in the Treatment of a Patient with Primary Orthostatic Hypotension. N Engl J Med. 1980; 302:1456-1457.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
Hashida T, Yoshioka K, Ikari YEffective Pacing Therapy for Syncope with Severe Orthostatic Hypotension and Chronotropic Incompetence.JCR 2013;3:353-357 |
|
Hashida T, Yoshioka K, Ikari YEffective Pacing Therapy for Syncope with Severe Orthostatic Hypotension and Chronotropic Incompetence.JCR [serial online] 2013[cited 2025 Dec 26];3:353-357. Available from: http://www.casereports.in/articles/3/2/Effective-Pacing-Therapy-for-Syncope-with-Severe-Orthostatic-Hypotension-and-Chronotropic-Incompetence.html |

|
|
|
|
|