6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff44cf040000008102000001001300
6go6ckt5b5idvals|272
6go6ckt5b5idcol1|ID
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Introduction
Fractures of the humerus shaft usually unite satisfactorily with conservative treatment but recently use of compression plates has yielded excellent results. Compression plating provides adequate stability with a high rate of union, particularly when combined with autogenous bone grafting, but it requires an extensive dissection, with consequent risks of infection and neurovascular complication [
1]. Spectrum of treatment of fracture mid-shaft humerus have been proposed ranging from conservative treatment, Sarmeinto’s functional bracing to plate osteosynthesis and intramedullary nailing. The humeral shaft is totally covered with muscles and fracture fragments are well vascularized, while malunions with an angle of less than 20 degrees are functionally and cosmetically well tolerated. Delayed union or non-union of the humerus following a fracture often leads to a painful upper extremity with limited function. The prevalence of humeral shaft nonunion as a complication of both non-operative and operative treatment has been reported to range from 8% to 12% [
2,
3].
In this article, we report a very unusual way of union of 25 year old fracture mid-shaft humerus in a 60 year old female defying all logics of fracture union.
Case Report
60 year old female patient, housewife, right hand dominant came to orthopedics OPD with recent history of fall in bathroom and injury to her left upper limb. Current X-rays revealed that patient had broken implant with fracture and previous non-bridging callus formation without any neuro-deficit [Fig.1]. Patient was a known case of ischaemic heart disease (IHD) with ejection fraction of 15%, uncontrolled diabetes mellitus (DM) on insulin regime with fasting and postprandial blood sugar of 290 mg% and 450 mg% respectively. Patient was also a known case of chronic renal failure on weekly dialysis. Patient had IHD and DM since past 10 years and chronic renal failure disease since last 2 years. Patient had past history of transverse fracture mid-shaft humerus 25 years prior due to road traffic accident. Patient had no history of any neurovascular complications. 25 years prior patient was operated by age old conventional lateral approach using plate osteosynthesis on lateral surface of humerus. Old local stainless steel plates, mechanical screws with single slotted head were used at that time. Later after 4-6 months post-surgery, patient developed pain at fracture site and restriction of functional activities of left upper limb which persisted till the recent trauma. Prior serial X-ray evaluation revealed that patient had developed non–union at fracture site [Fig.2]. Patient was unable to lift anything with left upper limb and had pain, tenderness at fracture site. The fracture had never healed. On enquiring further, patient also gave history that patient was advised repeat surgery with bone grafting 2 years after the first surgery but patient denied any further surgical interventions. 4 years post-surgery patient was given injection of autogenous bone marrow aspirate/fluid at fracture site. But the pain/tenderness at fracture site persisted with inability to lift anything by the fractured limb.
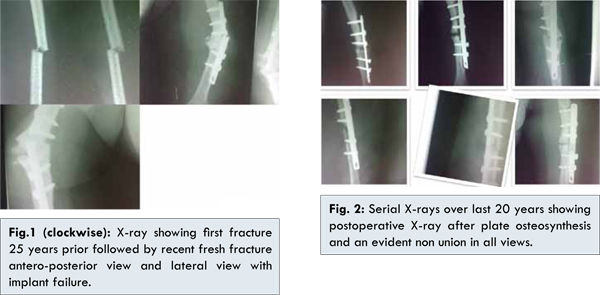
Currently, patient had repeat trauma and refracture at the prior non-union site with implant breakage with no neurovascular deficit. We planned for open reduction, implant removal, freshening of fractured edges, bone grafting and locking compression plate osteosynthesis by posterior or anterolateral approach. Though plan was simple, but removal of the old plate with single slotted mechanical screws from lateral surface of humerus was a great challenge and we were aware of the same. Also as patient was unfit due to her co-morbidities, delay in surgery was expected. Hence, we took her under image intensifier applied U-Brace in acceptable position. Patient took 3 weeks from history of recent trauma to be fit for surgery with controlled sugars.Repeat X-rays were taken at end of 3 weeks after trauma revealed callus uniting the fracture site [Fig.3]. Considering the old age, co-morbidities, less functional demands and recent onset union at the fracture site decision was taken to conserve the patient in U-brace. Fracture at the end of 6 weeks showed good union. 25 years old non-union not healed with surgery neither with autologous marrow fluid aspirate/fluid, got united merely with conservative treatment after recent trauma. This defies all the logic of fracture union and is quite astonishing.

Discussion
Bone is a living biological tissue composed of metabolically active cells that are integrated into a rigid framework. The healing potential of bone, whether in a fracture or fusion model, is influenced by a variety of biochemical, biomechanical, cellular, hormonal, and pathological mechanisms. A continuously occurring state of bone deposition, resorption and remodeling facilitates the healing process. Healing occurs in three distinct but overlapping stages [
4]: (i) early inflammatory stage: hematoma develops within the fracture site during the first few hours and days. Inflammatory cells infiltrate the bone under prostaglandin mediation. This results in the formation of granulation tissue, in-growths of vascular tissue, and migration of mesenchymal cells; (ii) repair stage: fibroblasts begin to lay down astroma that helps support vascular in growths and leads to the formation of a soft callus (iii) late remodeling stage: in which the healing bone is restored to its original shape, structure, and mechanical strength.
The density, geometry, thickness, and trabecular orientation of bone can change depending on the mechanical demands of thegraft. In 1892, Wolff first popularized the concept of structural adaptation of bone, noting that bone placed under compressive or tensile stress is remodeled. Bone is formed where stresses require its presence and resorbed where stresses do not require it [
5]. In our case, patient already had undergone previous surgery and had landed in non-union. With non-union and implant failure normal process of fracture union is not ensued but it seems it healed by the normal bone union process astonishingly after recent trauma and implant breakage.
Autologous bone-grafting is useful for treatment of delayed union and non-union. Besides being osteo-inductive and osteo-conductive it is histocompatible and lacks immunogenicity. Furthermore, there is no risk of an autologous graft transmitting occult disease or infection. There is reasonable surgical access to the iliac crest and an ample amount of graft material [
6,
7]. It is also important to correct angular deformities and achieve good axial and joint alignment. A stable construct provides an advantageous mechanical environment and is a prerequisite for successful bone-healing [
8]. The medullary canal of both the proximal and the distal fragment is often sealed by fibrous tissue or a sclerotic-osseous end-cap. We believe that the canal should be drilled to allow rapid neovascularization and migration of osteogenic cells. Careful intrafocal débridement is a key to ensuring optimal cortex-to-cortex stability, which facilitates neovascularization and migration of osteogenic cells and prepares the host environment for successful graft integration [
9]. Hence, for delayed unions and non-union appropriate fixation with autogenous bone grafting along with debridement of fracture edges and opening medullary canal is preferred mode of treatment. But in our case, despite the same plan we had to conserve the patient due to co-morbidities and unexpectedly callus formation occurred with good union after the recent trauma.
Percutaneous bone marrow injection is safe, easy, practical, and time-saving. It is economical and involves minimal trauma. It avoids donor site problems and can be repeated easily. It can be done under local anesthesia and avoids the risks of general anesthesia, infection and surgery [
10]. Though it has been proved useful in several cases of delayed union and non-union, in our case it did not promote any bone healing.
Parameters deemed acceptable for fracture reduction of mid shaft humerus fracture in adults are 30 degrees of varus angulation, 20 degrees of anterior bowing, and up to 15 degrees of internal rotation. Basic AO/Orthopaedic Trauma Association principles should be applied when performing plate fixation of humeral shaft fractures including restoration of anatomic alignment, avoidance of soft-tissue stripping to preserve vascularity to the fracture fragments, and provision of stable rigid fixation to allow for early range of motion and optimal functional recovery. Plate osteosynthesis, intramedullary nailing and conservative treatment-Sarmeinto’s bracing have been viable option for fresh fractures [
11]. Though conservative treatment has proved its efficacy, but till now it has been used for fresh fractures of humerus and never for non-union with implant failure as in our case. Also we had achieved acceptable alignment of humerus as per above criteria and has yielded good results too.
To conclude, we would like to say that there are many things with Mother Nature which has no rational reasoning. Union of this 25 year old fracture non-union by conservative method was a mystery for us. If thought rationally only theory supporting union was the sole presence of plate and its forces which might be in distraction hampered the union. But on first immediate post-operative X-ray, it didn’t look like the plate was applied in distraction. Repeat trauma and implant failure incited the normal process of fracture union with new hematoma formation and revascularization which lead to good callus formation and later union with good functional results.
References
- Klestil T, Rangger C, Kathrein B, Huber B, Waldegger M. Sarmiento bracing of humeral shaft fractures — a comparative study.SOT.1997;20.
- Rubel IF, Kloen P, Campbell D, Schwartz M, Liew A, Myers E et al. Open reduction and internal fixation of humeral nonunions: a biomechanical and clinical study. J Bone Joint Surg Am. 2002;84:1315-1322.
- Marti RK, Verheyen CC, Besselaar PP. Humeral shaft nonunion: evaluation of uniform surgical repair in fifty-one patients. J Orthop Trauma. 2002;16:108-115.
- Kalfas IH. Principles of bone healing. Neurosurg. 2001;10:1-10.
- Wolff JP, Furlong R. Berlin: The Law of Bone Remodeling. Translated by Maquet Springer-Verlag, 1986.
- Helfet DL, Kloen P, Anand N, Rosen HS. Open reduction and internal fixationof delayed unions and nonunions of fractures of the distal part of the humerus. J Bone Joint Surg Am. 2003;85:33-40.
- Chapman PG, Villar RN. The bacteriology of bone allografts. J Bone Joint Surg Br. 1992;74:398-399.
- Sommer C, Gautier E, Muller M, Helfet DL, Wagner M. First clinical results of the Locking Compression Plate (LCP). Injury. 2003;34 Suppl 2:B43-54.
- Christian Hierholzer, Domenico Sama, Jose B. Toro, Margaret Peterson, David l. Helfet-plate fixation of ununited humerus shaft fractures-effect of type of bone grafting and jealing. Journal of Bone & Joint Surgery Am. 2006;88(7):1425-1430.
- Garg NK, Gaur S, Sharma S. Percutaneous autogenous bone marrow grafting in20 cases of ununited fracture. Acta Ofthop Scand. 1993;64 (6):671-672.
- Matt Walker, Brian Palumbo, Brian Badman, Jordan Brooks, Jeffrey Van Gelderen, Mark Mighell, Humeral shaft fractures: a review. J Shoulder Elbow Surg. 2011;20:12-20.