6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ffa4c5030000000202000001000700
6go6ckt5b5idvals|232
6go6ckt5b5idcol1|ID
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Introduction
Systemic sclerosis is a rare connective tissue disease of unknown etiology characterized by increased collagen deposition leading to fibrosis and subsequent degeneration of the skin and internal organs. It accounts for an incidence of 4-12 individuals per million population. Females are affected three to four times more frequently than males. There is no racial predilection. Progressive systemic sclerosis is most commonly occurs between 30 and 50 years of age [
1]. The most prominent clinical observation is thickened, hidebound skin especially around the fingers and hands (sclerodactyly). Others include Raynaud’s phenomenon, telangiectasia, calcinosis, myositis, arthritis, tenosynovitis, renal failure, esophageal hypomotility, pulmonary fibrosis, and heart failure [
1]. A more localized variant of systemic sclerosis is termed the CREST syndrome (calcinosis, Raynaud’s phenomenon, esophageal dysmotility, sclerodactyly and telangiectasia) [
2]. Oral involvement is one of the features which are characterized by trismus, burning sensation, mucosal changes with palpable fibrous bands.
The aim of this article is to report a classical case of progressive systemic sclerosis (PSS) in a middle aged female patient with typical oral manifestations and radiologic findings along with rare radiographic changes like resorption of angle, posterior and inferior border of body of ramus and coronoid process.
Case Report
A 30 year old female patient diagnosed as progressive systemic sclerosis was referred from department of dermatology for her oral symptoms. On interviewing she complained of difficulty in mouth opening associated with burning sensation, dryness of mouth and paresthesia of finger tips, toes, lips and tongue since 2 months. She also had dysphagia, repeated history of heartburn, nausea and vomiting with diarrhea since 6 months, with a long history of increase in skin pigmentation, progressive difficulty in straightening her fingers and digital ulcers since 2 years. There was no history of joint pain or oliguria.
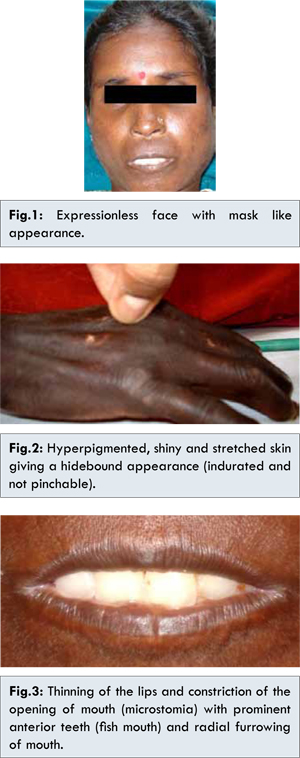
General physical examination revealed pallor and dystrophy of finger and toe nails. Patient had an expressionless face which gave a mask like appearance [Fig.1]. Skin appeared hyperpigmented, shiny and stretched giving a hidebound appearance (indurated and not pinchable) [Fig. 2]. There was loss of normal facial (skin folds) lines, presence of small and sharp (beak shaped) nose, thinning of the lips and constriction of the opening of mouth (microstomia) with prominent anterior teeth (fish mouth) and radial furrowing of mouth [Fig.3]. Acrosclerosis was noted with pitted scars present at the finger tips. There were few depigmented macules over the upper extremities [Fig.4]. On intraoral examination, restricted mouth opening of about 1.5 cm was noted [Fig.5]. There was diffuse fibrosis of buccal mucosa with loss of normal elasticity of mucosa. Palpable bands were present on right and left buccal mucosa. Depapillation of tongue and xerosis was noted.
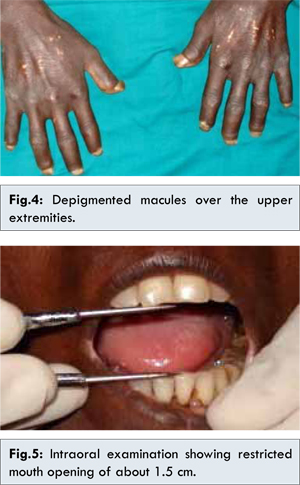
Patient was then subjected to radiographic examinations and OPG radiograph showed generalized widening of the periodontal ligament space, with bony resorption (irregular) on posterior border of coronoid process on both right and left side and resorption of inferior border, posterior border of ramus and angle of mandible on right side [Fig. 6,7]. Hand wrist radiograph showed resorption of bone which has caused dissolution of terminal phalanges of fingers [Fig. 8].
Haematological investigations showed hemoglobin 9 gms%, ESR 39 mm/hour, altered Albumin : Globulin ratio 2:5.9 (normal range 2:1) with positive ANA. Skin biopsy from back region revealed thickening of dermal collagen, eccrine glands appeared to be high up in the dermis and surrounded by collagen. Mild lymphocytic infiltration was seen around appendages. A few melanophages were seen in the upper dermis.
Patient was treated in dermatology department with pulse therapy by injection Cyclophosphamide 500 mg and injection Dexamethasone 100 mg in 500 ml of 5% Dextrose slow intravenously over 4 hours with continuous monitoring of pulse rate and blood pressure for 5 consecutive days and was discharged with the maintenance drugs like Cyclophosphamide 50 mg (OD), Ranitidine 150 mg (BID), Omeprazole 20 mg (OD).
Discussion
Systemic sclerosis (Scleroderma) is a multisystem chronic connective tissue disease of unknown etiology that involves hardening of skin and mucosae with smooth muscle atrophy and fibrosis of internal organs. There will be characteristic appearance of circumscribed or diffuse, hard, smooth, ivory colored areas that are immobile upon the underlying tissue that gives the characteristic hidebound skin. Classical facial appearance with expressionless face (mask like); stretched, shiny and not pinchable skin; sunken eyes; with parrot beaked nose. Since oral involvement is one of the features characterized by trismus, burning sensation and classical facial appearance, role of a dentist to identify this condition which shares similar features with other oral diseases like oral submucous fibrosis is important.
The precise etiology of PSS is unknown; however several factors seem to play a key role. Immunologic studies suggest that the possible pathogenesis could be autoimmune response directed against endothelium. Few others have shown coagulation abnormalities that result in thrombosis, occlusion, and extensive ischemic tissue damage [
3]. Fibroblast tissue culture studies have confirmed increased secretion of collagen proteins due to an overexpression at the transcriptional level hence suggesting fibroblasts growth abnormality [
4].
Taveras reported the first documented case of osteolysis of the mandibular angle and condyle [
5]. The etiology of the osteolysis is unknown. However, Taveras and Pogrel have proposed the following hypothesis: (i) Tightening of the facial skin may exert excessive pressure on the mandible and induce the bone loss. (ii) The vasculopathy associated with this disease may diminish the blood supply to the mandible resulting in ischemia and bone necrosis. (iii) Atrophy of the muscles of mastication such as the masseter muscle may lead to bone resorption. It is interesting to note that all bone resorption occurs in areas of muscle attachment [
5,
6].
Oral radiographic examination of these patients often reveals generalized enlargement of the periodontal ligament space which is caused by excess deposition of collagen and oxytalan fibres and subsequent resorption of alveolar crest bone surrounding the roots [
7,
8]. Stafne and Austin were the first to report involvement of the periodontal membrane in 9 of 127 (7.1%) with scleroderma [
9]. White et al documented thickened periodontal ligament space in 13 of 35 (37%) adult patients [
10]. Posterior teeth were affected more frequently than anterior teeth. The oral mucosa may undergo changes similar to those found in the skin. Mild edema followed by gradual atrophy and induration of the mucosal tissues. Also the color of the mucosa may change to more whitish tinge [
11]. About 26% of patients may develop lingual and buccal mucosal crenation (fissures /folds) and 16% may develop focal gingival recession. The gingival recession attributed to fibrotic stricture along the mandibular mucobuccal fold, thus causing stripping of the attached buccal gingiva [
12].
Due to the various forms and extent of systemic involvement, the prognosis in PSS is difficult to predict. In a study of 237 adult patients with PSS over 11 years, the mortality rate was 25.7%. The overall 3, 6, and 9 year survival rates of PSS were 86%, 76% and 61% respectively. Pulmonary manifestation was the most frequent cause of death. However, adverse prognostic factors include renal, cardiac, and pulmonary involvement in decreasing order of importance [
13].
Radiographically, this patient showed generalized widening of periodontal ligament space, with bony resorption (irregular) on posterior border of coronoid process on both right and left side and resorption of inferior border, posterior border of ramus and angle of mandible on right side. Hand wrist radiograph showed resorption of bone which as caused dissolution of terminal phalanges of fingers.
These patients often suffer from severe flexion deformities of their fingers and other body joints and thus have reduced manual dexterity. Maintenance of oral hygiene may be difficult due to the patient’s inability to grip and manipulate a toothbrush. A larger-handled toothbrush or flossing aids may allow easier grasping and facilitate maintenance of good oral hygiene [
14]. Our patient managed to keep her oral hygiene level quite high despite serious digital abnormalities.
Intraoral examination and intraoral procedures such as exposure of intraoral radiographs and extractions are difficult to perform due to tightening of skin, reduced inter-incisal distance, and diminished oral aperture. Surgical intervention such as bilateral commissurotomies can correct the microstomia [
15]. Naylor et al proposed nonsurgical alternative which involves cheek and mouth stretching exercises and tongue depressor exercises to increase inter-incisal distance to facilitate oral hygiene, mastication, and dental access [
16].
Conclusion
Progressive systemic sclerosis presents in variety of forms ranging from the most aggressive PSS to less aggressive and localized forms like CREST, morphea and linear scleroderma. Appropriate dental hygiene management of patients with this autoimmune disorder requires an understanding of clinical characteristics, the recognition of oral facial involvement, treatment considerations and pharmacological interventions so as to provide compassionate, safe and effective dental hygiene management and care to patients.
References
- Jimenez S, Varga J. Systemic sclerosis. In: Internal Medicine for Dentistry, 2nd Ed. Rose LF, Kaye D EDS. Toronto: The CV Mosby Co, 1990; pp. 50-55.
- Medsger TA Jr. Systemic sclerosis and localized scleroderma. In: Primer on the Rheumatic Diseases, 9th Ed. HR Schumacher, JH Klippel, DR Robinson, (eds). Atlanta: Arthritis Foundation, 1988;pp. 111-116.
- LeRoy EC. A brief overview of the pathogenesis of scleroderma (systemic sclerosis). Ann Rheum Dis. 1992;51:286-288.
- Potter SR, Bienenstock J, Lee P, Wilkinson S, Buchanan WW. Clinical associations of fibroblast growth promoting factor in scleroderma. J Rheumatol. 1984;11:43-47.
- Taveras JM. The interpretation of radiographs. In: Disorders of the Temporomandibular Joint, L Schwartz ED. Philadelphia: WB Saunders Co, 1959; pp 159-160.
- Pogrel MA. Unilateral osteolysis of the mandibular angle and coronoid process in scleroderma. Int J Oral Maxillofac Surg. 1988;17:155-156.
- Shafer WG, Hine MK, Levy BM. A textbook of Oral Pathology 4th Ed. Toronto: WB Saunders Co,1983; pp. 845-847.
- Wood RE, Lee P. Analysis of the oral manifestations of systemic sclerosis. Oral Surg Oral Med Oral Pathol. 1988;65:172-178.
- Stafne EC, Austin TL. A characteristic dental finding in Acrosclerosis and diffuse scleroderma. Am J Orthod & Oral Surg: sec Oral Surg. 1944;30:25-29.
- White SC, Frey NW, Blaschke DD, Ross MP, Clements PJ, Furst DE et al. Oral radiographic changes in patients with progressive systemic sclerosis (scleroderma). J Am Dent Assoc. 1977; 94:1178-1182.
- Parma Benfenati S, Fugazzotto PA, Berdichevsky M, Ferriera P, Calura G, Ruben MP. Progressive systemic sclerosis: Oral –mucosal changes. Gen Dent. 1986; 34:107-112.
- Eversole LR, Jacobsen PL, Stone CE. Oral and gingival changed in systemic sclerosis (scleroderma). J Periodontol. 1984; 55:175-178.
- Lee P, Langevitz P, Alderdice CA, Aubrey M, Baer PA, Baron M, et al. Mortality in Systemic Sclerosis (scleroderma). Q J Med. 1992; 82:139-148.
- Naylor WP. Oral management of the scleroderma patient. J Am Dent Assoc. 1982; 105:814-817.
- Springer PS. Dental correlations: Systemic sclerosis. In: Internal medicine for Dentistry, 2nd Ed. LF Rose, D Kaye EDS. Toronto: CV Mosby Co,1990; pp. 94-95.
- Naylor WP, Douglass CW, Mix E. The nonsurgical treatment of microstomia in scleroderma: A pilot study. Oral Surg Oral Med Oral Pathol. 1984;57:508-511.