|
|
|
|
|
Spinal Intramedullary Tuberculoma: Typical, Atypical Presentation on Magnetic Resonance Imaging
|
|
|
|
ML Prakash, Radha Sarwagi, Ramkumar, Prabhakaran, Srilatha K
From the Department of Radio-diagnosis, Mahatma Gandhi Medical College and Research Institute, Pondicherry, India. |
|
|
|
|
|
Corresponding Author:
|
|
Dr. Srilatha K
Email: drksrilatha9@gmail.com |
|
|
|
|
|
|
|
|
Received:
29-AUG-2013 |
Accepted:
15-OCT-2013 |
Published Online:
10-NOV-2013 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
Intramedullary tuberculous granulomas (tuberculomas) are rare in occurrence when compared to pulmonary, extra pulmonary and skeletal tuberculosis in developing countries. Here, we present clinical profile and Magnetic Resonance Imaging (MRI) findings in two intramedullary tuberculoma cases. The Magnetic Resonance Imaging (MRI) findings of intramedullary tuberculoma and its rarity in occurrence are discussed. The emphasis is on atypical presentations of intramedullary tuberculoma and the other intramedullary lesions that can closely resemble to it. |
|
|
|
|
|
Keywords :
|
Tuberculosis, Tuberculoma, Spinal Cord, Magnetic Resonance Imaging, Granuloma.
|
|
|
|
|
|
|
|
|
|
|
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff8871040000002c02000001001500 6go6ckt5b5idvals|259 6go6ckt5b5idcol1|ID 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
CNS tuberculosis occurs secondary to hematogenous spread from a sub clinical or radiologically occult primary, usually in the lungs. Although spinal tuberculosis is fairly common in developing countries, intramedullary spinal tuberculoma is a rare disease.Abercrombie first reported it in 1828 [ 1]. The reported incidence of intramedullary tuberculoma quoted being 2 per 100,000 cases of tuberculosis as cited by Ming Lu MD [ 2].
Case Report:
Case 1
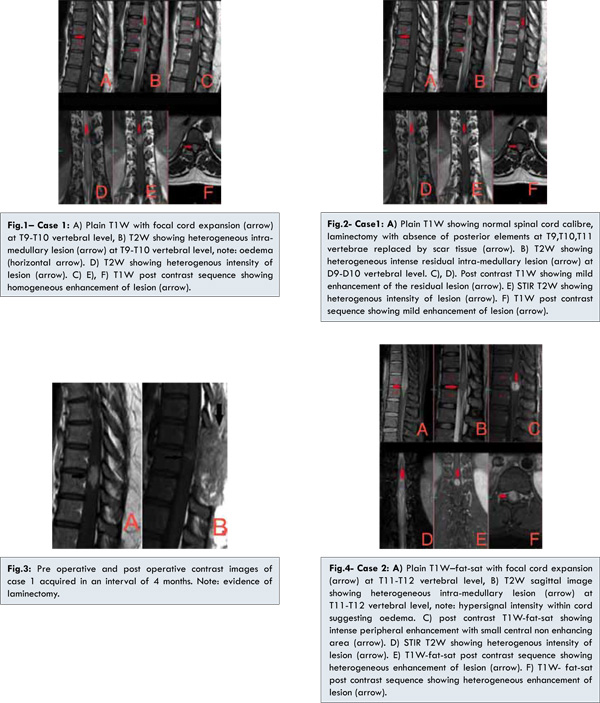
A 31-year-old female was admitted with complaints of intermittent back pain for 1 year, weakness and numbness in left lower limb for 3 weeks. There was no history of trauma or fever. Physical examination revealed mild muscle atrophy, hyporeflexia of the patellar tendon, and decreased sense of joint position in left lower limb. Limping gait was noted in left lower limb. Clinically there were no signs and symptoms suggestive of tuberculosis. Laboratory results including complete hemogram were within normal limits. Chest X-ray and ultrasound abdomen revealed no abnormality. Magnetic Resonance Imaging (MRI) of thoracic spine [Fig.1] showed well defined focal intramedullary oval lesion of size 2.3 (cranio-caudal)x1.0 (anterio-posterior)x1.0 (transverse) cm, involving the thoracic cord at T9 – T10 vertebral level with focal cord expansion at this level. Lesion was isointense to cord on T1-weighted image and hyperintense with central hypointensity on T2-weighted image. On T2-weighted image there was an ill-defined hyperintense signal within the cord extending superiorly upto T2 vertebral level and inferiorly upto conus suggestive of cord oedema. After gadopentetate dimeglumine administration, homogenous moderate enhancement was observed in the lesion on T1-weighted post contrast study. No meningeal enhancement, epidural collections or other focal lesions were seen. The vertebrae exhibited normal marrow signal intensity. With the above imaging characteristics of intramedullary lesion, differential diagnosis of tuberculous granuloma, ependymoma and glioma were suggested. Patient underwent laminectomy with open biopsy. Pathological examination showed multiple epitheloid granulomas with langerhans type giant cells, surrounded by lymphocytes and plasma cells suggesting granulomatous inflammation. Hence patient was started on anti tuberculous therapy. Patient was clinically relieved from back pain with normal power and sensation in left lower limb during the course of antituberculous therapy. Follow up MRI of thoracic spine [Fig.2] done after 4 months showed small residual focal intramedullary lesion at T9-T10 vertebral level, measuring 1.5 (cranio-caudal)x0.7 (anterio-posterior)x0.7 (transverse) cm. Post contrast images showed mild heterogenous enhancement of the lesion [Fig.3]. No other focal lesions or meningeal enhancement were seen.
Case 2
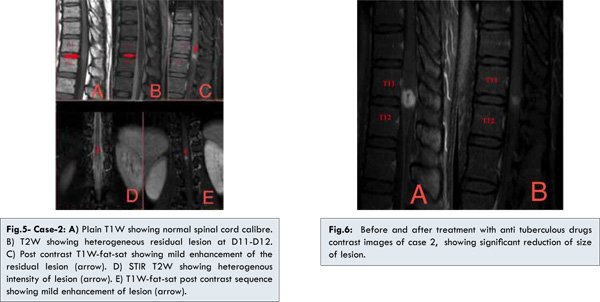
A 31-year-old male was admitted with complaints of intermittent back pain for four months. There was no history of weakness in lower limbs, trauma or fever. Physical examination showed only mild tenderness in lower segment of thoracic spine. All the four limbs showed normal reflexes without any muscle atrophy. Clinically there were no signs and symptoms suggestive of tuberculosis. Laboratory results including complete hemogram were within normal limits. Chest X-ray and ultrasound abdomen revealed no abnormality. Magnetic Resonance Imaging (MRI) of thoraco-lumbar spine showed a well-defined rounded intramedullary lesion, in distal thoracic cord near conus medullaris at T11-T12 level [Fig.4]. It measured 1.3 (cranio-caudal)x1.3 (anterio-posterior)x1.1 (transverse) cm in size. Lesion was iso-intense to cord on T1-weighted image, hyperintense with central hypointensity on T2-weighted image with perilesional edema in the distal cord extending from T10 to conus. After gadopentetate dimeglumine administration, intense peripheral enhancement with small central non-enhancing area was observed in the lesion on T1-weighted post contrast image. Mild leptomeningeal enhancement was also noted around the distal cord and conus. With the above imaging characteristics of intramedullary lesion and leptomeningeal enhancement, diagnosis of tuberculous granuloma was suggested. Patient was started on anti tuberculous treatment. Patient was clinically relieved from back pain within six weeks. Follow- up MRI study done two months after first study, revealed significant reduction in size of the intramedullary lesion to 0.8 (cranio-caudal)x0.7 (anterio-posterior)x0.6 (transverse) cm, as compared to previous study [Fig.5]. Post contrast images showed mild heterogenous enhancement of the lesion with resolution of perilesional edema and no abnormal meningeal enhancement [Fig.6].
Discussion
Intramedullary tuberculoma usually occurs at young age, with most common location in thoracic spinal cord [ 3]. Intramedullary tuberculoma has been described in young immunocompromised as well as immunocompetent individuals [ 4, 5]. Intramedullary tuberculoma patients often have a history of contact to patients with tuberculosis or an extracranial focus of tuberculosis [ 1]. Intramedullary tuberculoma can also occur solely, in absence of extra cranial focus or pulmonary involvement. In the series of intramedullary tuberculomas reported by Mac Donnel et al., [ 6] 38% of the patients had no evidence of tuberculous disease elsewhere. Most frequently patient presents clinically with signs of subacute spinal cord compression. Depending on location and extent of cord involvement, patient may present with focal pain, paraplegia, brown-sequard syndrome etc.
Typical Magnetic Resonance Imaging (MRI) characteristics of intramedullary tuberculoma are hypo or isointense to cord in T1-weighted sequence with only an indirect sign of focal cord expansion and heterogenous intensity on T2-weigted image with central hypointensity and peripheral hyperintensity, which is described as target sign.Peripheral enhancement is characteristic feature of tuberculomaon post contrast images [ 7, 8].The central hypointensity on T2- weighted image is suggestive of caseating necrosis. Occasionally the lesion may show central hyperintensity with peripheral hypointense ring, depending on protein content within the caseating necrosis or liquefaction.Perilesional edema is usually associated showing hypersignal intensity on T2-weighted image.Associated meningeal enhancement, tracking epidural collections, extradural involvement and skip lesions may coexist. Intra medullary tuberculoma can occur in combination with tuberculous spondylodiscitis and tuberculous arachnoiditis. Pulmonary and other extra pulmonary sites are to be evaluated for primary source of infection. In both our cases, chest X-ray and abdominal ultrasound were normal. Both the patients are immunocompetent. The second case had typical MRI characteristics of ring enhancement, T2 target sign and associated meningeal enhancement favoring intramedullary tuberculoma. In the first case the lesion was not showing signal characteristics of tuberculoma, with atypical features leading us to consider granulomatous lesion, ependymoma and glioma as possible differential diagnosis. Though a typical MRI imaging features like homogenous post contrast enhancement, common in immuno-compromised patients [ 9], they may also occur in immuno-competent patient as in our case and also reported in other case reports [ 10, 11]. Imaging characteristics of intramedullary tuberculoma, T2 Target sign, ring enhancement or homogenous enhancement may vary depending on immune response more than immune status. Syrinx formation secondary to inflammation in intramedullary tuberculoma is rare in occurrence where the literature is scanty. Hemorrhagic association of intramedullary tuberculomas not been reported so far. MRI is the best diagnostic tool to determine the location, number, and size of the lesions and to assess response to antituberculous chemotherapy in follow up imaging. In cases manifesting with typical MR imaging features, ATT and follow up imaging can avoid other intervention procedures. In absence of typical imaging characteristics, biopsy and histopathological correlation is essential.Optimum neurologic outcome is possible with microsurgical technique in patients with significant cord compression symptoms or neurological deficit. In addition to surgical treatment, chemotherapy with antituberculous drugs should be instituted as soon as the diagnosis is made to achieve the best neurologic outcome.
When intramedullary tuberculomas are found solely, and in particular with absence of pulmonary or extra cranial source of infection, and typical magnetic resonance imaging features, mimic closely to other intramedullary lesions. Ependymoma, Glioma or Intramedullary abscess caused by fungal organisms (eg: blastomycosis, histoplasmosis, candidiasis) may mimic intramedullary tuberculoma. Toxoplasmosis and lymphoma are common differential diagnosis of intramedullary tuberculoma in immunocompromised patients [Table 1].
Conclusion
Imaging characteristics of tuberculosis vary with immune response of individual, so typical MRI signal characteristics may not be seen in all individuals. Intramedullary tuberculoma is to be considered while imaging intramedullary lesion even in absence of pulmonary and other extra cranial manifestations.
References
- Li H, You C, Yang Y, He M, Cai B, Wang X, et al. Intramedullary spinal tuberculoma: report of three cases. Surg Neurol 2006;65:185–188.
- Ming LU. Imaging diagnosis of spinal intramedullary tuberculoma: Case reports and literature review. J Spinal Cord Med. 2010;33:159-162.
- Nussbaum ES, Rockswold GL, Bergman TA, Erickson DL, Seljeskog et al. Spinal tuberculosis: A diagnostic and management challenge. J Neurosurg. 1995;83:243–247.
- Alessi G, Lemmerling M, Nathoo N. Combined spinal subdural tuberculous empyema and intramedullary tuberculoma in an HIV-positive patient. Eur Radiol. 2003;13:1899-1901.
- Chagla AS, Udayakumaran S, Balasubramaniam S. Cervical intramedullary tuberculoma in an infant. J Neurosurg. 2007;106:243.
- Macdonnell AH, Baird RW, Bronze MS. Intramedullary tuberculomas of the spinal cord: Case report and review. Rev Infect Dis. 1990;12:432-439.
- Chang KH, Han MH, Roh JK, Kin IO, Han MC, Kim CW. GD-DTPA enhanced MR imaging in intracranial tuberculosis. Neuroradiology. 1990;32:19–25.
- Gupta VK, Sharma BS, Khosla VK. Intramedullary tuberculoma: report of two cases with MRI findings. Surg Neurol. 1995;44:241–244.
- Mohit AA, Santiago P, Rostomily R. Intramedullary tuberculoma mimicking primary CNS lymphoma. J Neurol Neurosurg Psychiatry. 2004;75:1636-1638.
- Tyagi DK, Balasubramaniam S, Purandare HS, Savant HV. Intramedullary tuberculoma in a six year old. Neurology India. 2010;58:736-738.
- Tanriverdi T, Kizilkiliç O, Hanci M, Kaynar MY, Unalan H, et al. Atypical intradural spinal tuberculosis: Report of three cases. Spinal cord. 2003;41:403-409.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
Prakash ML, Sarwagi R, Ramkumar, Prabhakaran, K SrilathaSpinal Intramedullary Tuberculoma: Typical, Atypical Presentation on Magnetic Resonance Imaging.JCR 2013;3:404-409 |
|
Prakash ML, Sarwagi R, Ramkumar, Prabhakaran, K SrilathaSpinal Intramedullary Tuberculoma: Typical, Atypical Presentation on Magnetic Resonance Imaging.JCR [serial online] 2013[cited 2025 Dec 15];3:404-409. Available from: http://www.casereports.in/articles/3/2/Spinal-Intramedullary-Tuberculoma-Typical-Atypical-Presentation-on-Magnetic-Resonance-Imaging.html |

|
|
|
|
|