6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff847703000000f001000001000c00
6go6ckt5b5idvals|217
6go6ckt5b5idcol1|ID
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Introduction
Chondromyxoid fibroma (CMF) is a rare, benign tumour of cartilaginous origin and perhaps the rarest of all bone tumours [
1]. In 1948, the tumour was first described by Jaffe and Lichtenstein and it should be differentiated from chondrosarcoma and enchondroma [
2]. CMF comprise less than 1% of bone tumours and less than 2% of benign bone tumours. It mainly affects the metaphysis of long bones in children and young adults. It is more frequent in men than in women [
3]. It has a cartilage like matrix of varying proportions of chondroid, fibrous and myxoid areas [
2]. Although it is a benign tumour but rate of recurrence may occur from 10-80% [
4-
6]. We are presenting a case of CMF of 32 year old female involving proximal end of tibia.
Case Report
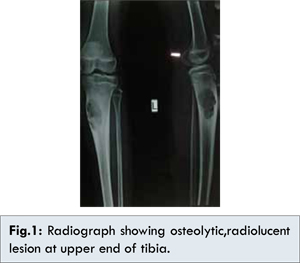
A 32 year old female presented with one and half year history of pain and local swelling of proximal end of tibia. Pain was dull-aching and not aggravated by walking. Knee joint movement was normal. There was no history of previous trauma, any pathological fracture or any operative procedure. Physical examination revealed mild tenderness over the swelling. Laboratory examination was within normal limits including complete blood count, erythrocyte sedimentation rate, rheumatoid factor and C- reactive protein. The X-ray examination showed an eccentric, radiolucent, lobulated lesion with a sclerotic rim and septation in proximal end of tibia with no calcification or periosteal reaction [Fig.1]. From the clinical and radiological findings clinical diagnosis of aneurysmal bone cyst and chondromyxoid fibroma were suspected. Curettage along with bone grafting was done under spinal anaesthesia and tissue sent for histopathological examination.
Gross examination revealed multiple cartilaginous bony bits approximately 10 cc in volume, greyish white in appearance with few haemorrhagic bits.Histopathological examination of multiple serial sections shows lobular pattern with stellate shaped cells in a myxoid and chondroid background. Lobules composed of hypocellular area in centre and hypercellular area in peripheries, and focally located multinuclear osteoclastic giant cells were seen [Fig.2,3,4]. Histopathological examination confirmed the diagnosis of CMF.
Discussion
Chondromyxoid fibroma (CMF) is a rare, benign, although potentially aggressive tumour of cartilaginous origin and accounts for less than 1% of all bone tumour [
2]. The common site of the tumour is the metaphysis adjacent to the epiphyseal growth plate which is consistent with the hypothesis that the tumour arises from remnants of cartilage at these sites [
4].
World Health Organization defined CMF as “a benign tumour characterized by lobules of spindle-shaped or stellate cells with abundant myxoid or chondroid intercellular material separated by zones of more cellular tissue rich in spindle-shaped or round cells with varying number of multinucleated giant cells of different sizes” [
3]. It may be misdiagnosed as other tumours such as chondrosarcoma because of some similarities and it is important to distinguish it by establishing the clinical, radiological and pathological features of CMF. Clinically patients presented with pain, swelling or tenderness and duration may range from weeks to years [
7]. Our patient had similar symptoms.
Radiologically the lesion is single, eccentric, radiolucent with lobulated margin, septations, cortical expansion and a sclerotic rim [
8]. Magnetic resonance imaging (MRI) examination is not helpful to confirm the diagnosis but helps in knowing the extent of spread of tumour [
9]. In our case, MRI was not done.
Diagnosis of CMF is basically depends upon the characteristics histological appearance. The typical histological features of CMF are a lobular pattern with stellate or spindle-shaped cells in a myxoid or chondroid background. Lobules demonstrate hypocellular centres and hypercellular peripheries. Osteoclast like giant cells are often present at the lobular peripheries [
3]. Dahlin stressed that giant cell at the periphery of the chondroid lobules with plump hyperchromatic nuclei are characteristic of CMF [
10]. Similar feature is seen in our case. Differential diagnosis of CMF includes chondrosarcoma, chondroblastoma, aneurysmal bone cyst, enchondroma but the characteristic histological features ruled out these lesions.
Treatment options of CMF include en bloc resection, simple curettage, and curettage with bone grafting or polymethylmethacrylate placement. CMF is a benign tumour but rate of recurrence is high when treated with simple curettage of lesion. But curettage with bone grafting has very low rate of recurrence. Gherlinzoni F et al reported curettage alone was associated with 80% recurrence rate, but when curettage was combined with bone grafting the recurrence rate decreased to 7% [
6]. In our case, patient was treated by curettage along with bone grafting and has no recurrence in a follow-up period of one year.
Conclusion
CMF is a rare benign bone tumour. Clinically and radiologically it may confused with other benign or malignant bone tumours. Histopathological examination is important not only for accurate diagnosis of this rare benign tumour but also for appropriate treatment. Curettage with bone grafting is the choice of treatment with low rate of recurrence.
References
- Yalniz E, Alicioglu B, Yilmaz B. Non specific magnetic resonance features of chondromyxoid fibroma of the iliac bone. J BUON. 2007;12:407-409.
- Jaffe HL, Lichtenstein L. Chondromyxoid fibroma of bone. A distinctive benign tumor likely to be mistaken especially for chondrosarcoma. Arch Pathol. 1948;45:541–551.
- Fletcher CD, Unni KK, Mertens F. World Health Organization classification of tumors. Lyon; IARC Press, 2002: 243-245.
- Rahimi A, Beabout JW, Ivins JC, Dahlin DC Chondromyxoid fibroma: a clinicopathologic study of 76 cases. Cancer. 1972;30:726–736.
- Schajowicz F, Gallardo H. Chondromyxoid fibroma of bone. A clinico-pathological study of thirty-two cases. J Bone Joint Surg Br. 1971;53:198–216.
- Gherlinzoni F, Rock M, Picci P. Chondromyxoid fibroma. The experience at the Instituto Ortopedico Rizzoli. J Bone Joint Surg Am. 1983;65:198–204.
- Zillmer DA, Dorfman HD. Chondromyxoid fibroma of bone: thirty-six cases with clinicopathologic correlation. Hum Pathol. 1989;20:952–964.
- Rouas L, Malihy A, Cherradi N, Lamalmi N, Alhamany Z. Chondromyxoid fibroma of bone. A rare benign bone tumour in children. Rev Med Brux. 2004;25:521-524.
- Sutton D (ed). Textbook of radiology and imaging. 7th ed, Churchill Livingstone, Edinburgh, 2003.
- Dahlin DC, Unni KK. Bone tumors, general aspects and data on 8,542 cases. Charles C. Thomas, Springfield.1986:57–70.