Introduction
Hashimoto’s thyroiditis is one of the commonest causes of primary hypothyroidism. Owing to insidious clinical onset, diagnosis of hypothyroidism in absence of an overt goiter often becomes difficult. An external pressure by goitorous lesion often leads to compression of trachea in hypothyroid conditions. However, near total narrowing of naso- oropharyngeal and laryngeal airway to the extent of causing stridor secondary to myxedema is rare phenomenon. We present a newly diagnosed case of hypothyroidism in an elderly male without neck swelling leading to an acute onset life threatening upper airway obstruction as a result of myxedema of naso-oropharynx and larynx.
Case Report
A 60 year male patient was brought to emergency department with progressive difficulty in breathing and noisy breathing over 2 to 3 days. He was known case of hypertension and ischemic heart disease. There was no history suggestive of hoarseness of voice, difficulty in swallowing, mass or swelling over the neck. History of snoring was present. No positive drug history elicited. On general physical examination at the time of admission he was drowsy, tachypoenic and was having tachycardia. His blood pressure was measuring 180/120 mm Hg. There was puffiness of the face and generalized non pitting edema in the pretibial region of lower extremities. Local examination of oral cavity revealed large dry and coated tongue. Without assisted oxygenation his blood oxygen saturation was dropping below 80%.
The flexible laryngoscopy was suggestive of diffuse edema of the nasopharynx, oropharynx and the supraglottis. Visibility of the vocal cords was poor. The risk of oral endotracheal intubation under general anesthesia was higher considering his uncontrolled hypertension, edema of supraglottis and glottis. Therefore, a decision for emergency tracheotomy under local anesthesia was done to secure the airway.
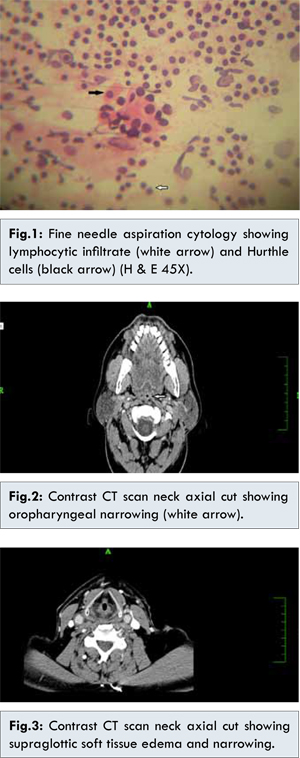
Except for raised TSH and CPK (creatinine phosphokinase) his all other hematological parameters were within normal range. Considering the raised levels of TSH, an USG guided fine needle aspiration cytology of thyroid gland was carried out to rule out possible thyroid pathology. The cytology showed lymphocytic infiltrates along with Hurthle cells, a feature suggestive of Hashimoto’s thyroiditis [Fig.1]. A CT scan of the neck and thorax showed severe nasopharyngeal, oropharyngeal and supraglottic airway narrowing by soft tissue edema [Fig. 2,3]. Posterior third of the tongue was hypertrophied and edematous. Possibility of lingual thyroid was ruled out after radiological visualization of normal thyroid gland in the neck. There was no evidence of growth anywhere in above mentioned areas on endoscopic and radiological investigations.
Patient was started with oral administration of 125 µg of levothyroxine; dosage was increased gradually to 200 µg and continued over 4 weeks with weekly monitoring of TSH levels. The flexible laryngoscopy done after four weeks showed resolution of myxedema changes [Fig. 4]. Decannulation of tracheotomy was done after appearance of satisfactory airway. Patient was monitored further for snoring and any episode of respiratory obstruction.
Discussion
Hypothyroidism is known for its insidious onset and subtle clinical presentations. Only 0.3 % of hypothyroidism showed overt symptomatology in study conducted by Golden SH et al [
1]. Thyroid hormone is one of the important body hormone. Its deficiency is associated with multiple cardiovascular complication, respiratory failure and coma. The spectrum of diseases involvement ranges from mild dyspnea to life threatening respiratory failure. Amongst the various mechanisms claimed in pathophysiology of respiratory failure caused by hypothyroidism the reduction in central respiratory drive, respiratory muscle weakness and sleep related breathing disorders are the crucial one [
2].
Autoimmune (Hashimoto’s) thyroiditis is the commonest cause of hypothyroidism, affecting about 5 to 10% of middle age women. Males are less frequently affected than females, with female preponderance of 10:1 to 20:1. Prevalence of hypothyroidism increases with age. Goiter is the commonest presentation of Hashimoto’s thyroiditis, Hashimoto described in his report patients with goiter and intense lymphocytic infiltration of thyroid gland [
3]. It presents as diffuse firm thyroid enlargement, sometimes accompanied by signs of tracheal or esophageal compression. Presence of circulating autoantibodies against thyroglobulin and thyroid peroxidase leads to progressive depletion of thyrocytes by apoptosis and subsequent replacement of normal thyroid parenchyma by mononuclear cell infiltration and fibrosis. Thus later stage of the disease might manifest itself with minimum residual thyroid tissue without overt thyroid swelling on the neck.
Our patient had insidious onset hypothyroidism which went undiagnosed over long period in absence of any obvious external thyroid swelling. Clinical or overt hypothyroidism is a state referred to as TSH greater than 10 IU/L. Symptoms of hypothyroidism becomes more apparent beyond this level. Subtle clinical manifestations of hypothyroidism include tiredness, feeling of cold, hair loss, loss of appetite, constipation, non-pitting edema of the extremities and puffiness over the face. Some of the above said features were present in our patient. The fluid retention in hypothyroidism is known as myxedema. Deposition of hydrophilic mucopolysaccharide and hyaluronic acid in the dermis, tongue, hypopharynx [
4] and other interstitial tissues is responsible for this state leading to non pitting edema.
Association of obstructive sleep apnea (OSA) and hypothyroidism is long debated. Our patient gives history of snoring and day time sleepiness. On this background we tried to investigate role OSA as an etiological factor for causing respiratory obstruction. Remmers JE et al concluded in the study of pathogenesis of upper airway in sleep apnea that patency of upper airway is determined by its compliance and the balance of forces across it [
5]. Various factors determining the upper airway sizes are: obesity, gender and individual variations in the size of mandible, tongue and the soft palate. Series F et al demonstrated hypertrophy in upper airway muscles in patients with OSA [
6]. The overwork done by the pharyngeal dilator muscles during period of wakefulness lead to hypertrophy in these group of muscles. This hypertrophic myopathy may impair ability to dilate the upper airway.
The hypothyroidism induced myopathy is known to affect proximal limb muscles. Our patient showed rise in CPK levels to 490 IU. Petrof BJ et al in a cadaveric study performed on hypothyroid rats suggested alteration in myosin heavy chain profile specifically in the Genioglossus muscle [
7]. The upper airway dilating muscles (Geniohyoid which influences position of hyoid, Genioglossus which holds tongue & tensor palatine which maintains palatal position) helps keeping the airway patent both during sleep and wakefulness. Further Devdhar M et al showed altered regulatory control of pharyngeal dilator muscle because of hypothyroidism induced neuropathy [
8]. All these changes set in vicious cycle thereby increasing the compliance of upper airway in hypothyroidism.
An axial CT scan of the neck in our patient demonstrated multilevel narrowing due to edema of the airway in our patient. Though its difficult to comment solely upon computed tomography scan only, whether the resultant narrowing is because of edema or hypertrophic myopathy of pharyngeal muscle as described by Petrof BJ et al and Devdhar M et al [
7,
8].
Another contrast enhanced axial CT scan of the neck through supraglottis demonstrated narrowing of an entire segment. The airway of featureless supraglottis looked to be reduced by myxedema of the soft tissue. The cadaveric studies by Altman et al demonstrated thyroid hormone receptors in human larynx and hypo pharynx [
9]. Presence of these receptors makes upper airway susceptible to hypothyroid induced myxedema changes.
Conclusion
Hypothyroidism induced myxedema of upper airway and myopathy of pharyngeal dilator muscle lead to an acute upper air way obstruction in our patient. This case report highlights the occurrence of rare event of upper airway obstruction in not so uncommon (hypothyroidism) condition, and hence deems attention amongst clinicians.
Raising its clinical profile is important as the treatment with levo-thyroxine reverted features of hypothyroidism, and hence ruled out obstructive sleep apnea alone as cause of morbid airway obstruction in our patient.
References
- Golden SH, Robinson KA, Saldanha I, Anton B, Ladenson PW. Clinical review: Prevalence and incidence of endocrine and metabolic disorders in United States: a comprehensive review. J Clin Endocrinol Metab.2009;94:1853-1878.
- Duranti R, Gheri RG, Gorini M, Gigliotti F, Spinelli A, Fanelli A, Sanco G. Control of breathing in patients with severe hypothyroidism. Am J Med.1993; 95:29-37.
- Hashimoto H. Zur Kenntniss der lymphomatosen Veranderung der Schilddruse (struma lymphomatosa). Arch Klin Chir; 1912; 97:219.
- Orr WC, Males JL, Imes NK. Myxedema and obstructive sleep apnea. Am JMed.1981;70:1061-1066.
- Remmer JE, deGroot WJ, Sauerland EK, Anch AM. Pathogenesis of upper airway occlusion during sleep. Journal of Applied Physiology. 1978; 44:931-938.
- Series F, Cate C, Simoneau JA, Gelinas Y, St Pierre S, Leclerc et al. Physiological, metabolic and muscle fiber type characteristic of musculus uvulae in sleep apnea hypopnea syndrome and in snorers. Journal of clinical investigation.1995;89:1571-1579.
- Petrof BJ, Kelly AM, Rubinstein NA, Pack AI. Effect of hypothyroidism on myosin heavy chain expression in rat pharyngeal dilator muscles.
- Devdhar M, Ousman YH, Burman KD. Hypothyroidism. Endocrinol Metab Clin North Am. 2007;36:595-615.
- Altman KW, Haines GK, Vakkalanka et al. Identification of thyroid hormone receptor in human larynx. Laryngoscope. 2003;113:1931-1934.