|
|
|
|
|
Pandemic Influenza A (H1N1) Infection and Subconjunctival Hemorrhage: Report of Three Cases.
|
|
|
|
Nermin Kelebek Girgin, Remzi Iscimen, Mehmet Baykara1, Halis Akalin2, Ferda Kahveci
From the Department of Anaesthesiology and Reanimation; Department of Eye Disease1; Department of Microbiology and Infectious Disease2; School of Medicine; Uludag University Bursa, Turkey. |
|
|
|
|
|
Corresponding Author:
|
|
Dr. Nermin Kelebek Girgin
Email: nerminkelebek@yahoo.com |
|
|
|
|
|
|
|
|
Received:
25 JUNE 2013 |
Accepted:
20-JULY-2013 |
Published Online:
10-AUG-2013 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
Subconjunctival hemorrhage (SCH) is defined as blood between the conjunctiva and the sclera. It can be caused by heavy lifting, coughing, and vomiting or by some infectious diseases. While conjunctivitis due to H1N1 influenza is reported, there is no SCH reported in the literature subsequent to H1N1 infection. We describe SCH in three patients with pandemic influenza H1N1 infection who were treated in intensive care unit (ICU). The first case is a 25-year-old pregnant woman with a 5-day history of runny nose mild cough and unilateral SCH. The second patient is a 37-year-old woman, with the diagnosis of pandemic H1N1 infection and diagnosed with bilateral SCH. Lastly, the third patient, a 49-year-old woman, was admitted to ICU with a 4-day history of cough, sputum and shortness of breath and diagnosed with bilateral SCH after 13 days of stay in ICU. None of these patients complained about visual changes, lacrimation or pain. Any increase in severity of SCH did not occur, and the findings resolved spontaneously within a few days in all patients. These cases suggest that intensivists and ophthalmologists should be aware of ocular manifestation such as subconjunctival hemorrhage in patients with H1N1 infection. |
|
|
|
|
|
Keywords :
|
Influenza A Virus, H1N1 Subtype, Conjunctival Diseases, Conjuctivitis, Eye, Cough.
|
|
|
|
|
|
|
|
|
|
|
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff64a603000000fc01000001000700 6go6ckt5b5idvals|224 6go6ckt5b5idcol1|ID 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
Subconjunctival hemorrhage (SCH) is among the most common eye diseases and characterized by acute appearance of a flat area of bleeding between the conjunctiva and the underlying sclera [ 1]. It is generally a benign disorder with a good visual prognosis. Data from many studies have shown that it can occasionally be caused by sneezing, coughing, vomiting, local trauma, systemic hypertension, medical disorder or drugs causing bleeding or those inhibiting normal clotting [ 1, 2]. Furthermore, several systemic bacterial and viral infections including, leptospirosis, adenovirus, herpes virus, Crimean Congo or Dengue fever are the leading causes of bacterial and viral conjunctivitis causing SCH [ 3- 7]. To our knowledge, while bleeding follicular conjunctivitis, uveitis and optic neuritis due to H1N1 influenza are reported [ 8- 10], there is no document in literature regarding SCH associated with influenza H1N1 infection.
The objective of this report is to share the experience gained through SCH in three patients with pandemic influenza H1N1 infection, who were treated in intensive care unit (ICU).
Case Reports
Case 1: A 25-year-old pregnant woman (para 9, gravida 1) was admitted to ICU at 26 weeks of gestation, with a 5-day- history of runny nose and mild cough. On examination she had bilateral crackles and wheezes. Pandemic H1N1 infection was suspected and oseltamivir was administered. Her oxygen saturation was noted to be low and she had difficulty in breathing. Afterwards, she was intubated and invasive mechanical ventilation (IMV) was started. At the time of admission to ICU, unilateral SCH was diagnosed. She denied any history of trauma or heavy lifting. She had not been taking any anticoagulants or blood thinning products before admission.
Case 2: Having been intubated a 37-year-old woman was transferred to our ICU because of the diagnosis of pandemic H1N1 infection. She had a 3-day-history of cough and sputum, and fever on the last day before admission. Examination revealed bilateral crackles. Oseltamivir and IMV therapies were initiated. Fifteen days following therapies, unilateral SCH was diagnosed.
Case 3: A 49-year-old woman was admitted to ICU due to a 4-day- history of cough, sputum and shortness of breath. She had bilateral crackles, and we thought that these symptoms were caused by H1N1 infection. Her peripheral oxygen saturation was 92% by oxygen mask at a rate of 6L/minute. At that time, her external ocular examination was unremarkable; there were no lesions seen externally on the eyelids. Non-invasive mechanical ventilation was applied for two days, subsequently the patient was intubated, and IMV therapy was initiated. Thirteen days after her having stayed in ICU, the diagnosis of bilateral SCH was established [Fig.1].
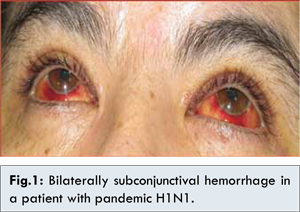
The definitive diagnosis of H1N1 infection was based on typical clinical and epidemiological findings and detection of H1N1 by serological analysis. Even though the diagnosis of SCH was made through ocular examinations none of the patients complained about visual changes, lacrimation or pain. There was no evidence for bleeding from other sites. They had no history of bleeding episodes in the past, and neither family history for such complaints was present. The patients had no thrombocytopenia. Demographic, laboratory and ICU data of these patients are seen in Table 1.
No increase in severity of SCH occurred during the hospital stay. The findings of these patients resolved spontaneously within a few days completely. During one month follow up no evidence for bleeding was noted in the second and third cases. The second and third cases were discharged from ICU at 16 and 17 days in good condition, respectively. The first case died of multiple organ failure in twenty-second day in the ICU.
Discussion
This article reports manifestations of SCH developing during the course of H1N1, in the absence of coagulopathy or trauma. The pathogenesis of SCH due to infections remains to be understood. Viruses may cause pathologic changes both in the ocular structures and in the ocular surface through direct invasion either by the virus, or through induction of a secondary inflammation and alteration of autoimmune mechanisms [ 6]. It has been known that infection of the endothelium plays an important role in pathogenesis of some viral diseases and that capillary fragility is a common feature [ 3, 5, 6, 11]. Impairment of endothelial cell function has been suggested to cause a wide range of vascular effects that lead to changes in vascular permeability or hemorrhage. The endothelium can be targeted in two ways: indirectly by viral factors or virus-mediated host-derived soluble factors that cause endothelial activations and dysfunction, and /or directly by virus infection and replication in endothelial cells [ 5, 11].
Some viral infectious agents can cause conjunctivitis and then weaken the walls of small blood vessels under the conjunctiva [ 3- 5, 12]. Subconjunctival hemorrhage was found to occur early in most patients with hemorrhagic adenoviral kerato-conjunctivitis by Chang et al [ 3]. In their study, the authors have shown that there are some indicators of conjunctiva inflammation, such as cytokines and chemokines secreted by infected conjunctiva or infiltrating immune cells [ 3]. While conjunctivitis following infection with H5N1 or human influenza viruses is rarely seen, most human infections associated with H7 subtype viruses have resulted in ocular diseases [ 12]. The properties contributing to an apparent ocular tropism of some influenza viruses have not yet been well understood. Some authors have thought that influenza viruses could be an infection of endothelium, some of which have endotheliotropism [ 8, 13]. Chan et al. [ 14] reported that the tissue tropism of the H1N1 virus of swine-origin and human seasonal H1N1 virus in primary in vitro and ex vivo cultures of the human respiratory tract was similar except that only H1N1 virus of swine-origin infected and replicate in human conjunctiva. The authors also suggested that the conjunctival tropism was dependent on the cell surface sialic acids.
Subconjunctival hemorrhage is thought to result from straining during sneezing, coughing (pertussis, pertussis coughing), retching, and excessive vomiting that lead to a rise in intraocular pressure and subsequent rupture of the small vessels in the conjunctiva [ 1, 3]. Neither history of nausea nor vomiting was present in our cases. Although coughing was the common symptom at the beginning of the disease in all patients, the time elapsed between the first appearance of symptoms of H1N1 infection and ocular findings was 13 to 15 days in two patients. During that time, the patients did not have coughing. The third patient had hypertension. Some authors suggest that, even if hypertension is controlled with drugs, patients with hypertension are more likely to have micro vascular damage (such as SCH) than healthy subjects [ 3]. Hypertension may facilitate development of SCH.
Conclusion
Intensivists and ophthalmologists should, thus, be aware of ocular manifestations including, subconjunctival hemorrhage, which may be temporary and harmless in patients with H1N1 infection, furthermore, the patients with H1N1 should be examined for bleeding within the eye.
References
- Mimura T, Usui T, Yamagami S, Funatsu H, Noma H, Honda N, et al. Recent causes of subconjunctival hemorrhage. Ophthalmology. 2010; 224:133-137.
- Leiker LL, Mehta BH, Pruchnicki MC, Rodis JL. Risk factors and complications of subconjunctival hemorrhages in patients taking warfarin. Optometry. 2009;80:227-231.
- Chang C, Sheu M, Lin K, Chen C. Hemorrhagic viral keratoconjunctivitis in Taiwan caused by adenovirus types 19 and 37: applicability of polymerase chain reaction-restriction fragment length polymorphism in detecting adenovirus genotypes. Cornea. 2001;20:295-300.
- Kapoor HK, Bhai S, John M, Xavier J. Ocular manifestations of dengue fever in an East Indian epidemic. Can J Ophthalmol. 2006;41:741-746.
- Engin A, Erdogan H, Ozec AV, Elaldi N, Toker MI, Bakir M, et al. Ocular findings in patients with Crimean-Congo hemorrhagic fever. Am J Ophtalmol. 2009;147:634-638.
- Najjar DM, Youssef OH, Flanagan JC. Palpebral subconjunctival hemorrhages in herpes zoster ophthalmicus. Ophthal Plast Reconstr Surg. 2008;24:62-64.
- Rathinam SR. Ocular manifestations of leptospirosis. J Postgrad Med. 2005;51:189-194.
- Lopez-Prats MJ, Sanz Marco E, Hidalgo-Mora JJ, Garcia-Delpech S, Diaz-Llopis M. Bleeding follicular conjunctivitis due to Influenza H1N1 virus. J Ophthalmol. 2010; 2010:423672.
- Khairallah M, Kahloun R, Ben Yahia S, Jelliti B, Messaoud R. New infectious etiologies for posterior uveitis. Ophthalmic Res. 2013;49:66-72.
- Mansour DE, El-Shazly AA, Elawamry AI, Ismail AT. Comparison of ocular findings in patients with H1N1 influenza infection versus patients receiving influenza vaccine during a pandemic. Ophthalmic Res. 2012;48:134-138.
- Klenk HD. Infection of the endothelium by influenza viruses. Thromb Haemost. 2005; 94:262-265.
- Writing Committee of the Second World Health Organization Consultation on Clinical Aspects of Human Infection with Avian Influenza A (H5N1) Virus: Abdel-Ghafar AN, Chotpitayasunondh T, Gao Z, Hayden FG, Nguyen DH, de Jong MD, et al. Update on Avian influenza A (H5N1) virus infection in humans. N Engl J Med. 2008; 358:261-273.
- Bingham J, Green DJ, Lowther S, Klippel J, Burggraaf S, Anderson DE, et al. Infection studies with two highly pathogenic avian influenza strains (Vietnamese and Indonesian) in Pekin ducks (Anas platyrhynchos), with particular reference to clinical disease, tissue tropism and viral shedding. Avian Pathol. 2009;38:267-278.
- Chan MC, Chan RW, Yu WC, Ho CC, Yuen KM, Fong JH, et al. Tropism and innate host responses of the 2009 pandemic H1N1 influenza virus in ex vivo and in vitro cultures of human conjunctiva and respiratory tract. Am J Pathol. 2010;176:1828-1840.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
Girgin NK, Iscimen R, Baykara M, Akalin H, Kahveci FPandemic Influenza A (H1N1) Infection and Subconjunctival Hemorrhage: Report of Three Cases..JCR 2013;3:262-266 |
|
Girgin NK, Iscimen R, Baykara M, Akalin H, Kahveci FPandemic Influenza A (H1N1) Infection and Subconjunctival Hemorrhage: Report of Three Cases..JCR [serial online] 2013[cited 2025 Dec 16];3:262-266. Available from: http://www.casereports.in/articles/3/2/pandemic-influenza.html |

|
|
|
|
|