|
|
|
|
|
Pathologic Femur Fracture: An Unusual First Clinical Manifestation of Prostate Carcinoma
|
|
|
|
Bijit Lodh, Sholay Kangjam Meitei, Bernard Amer, Rajendra Singh Sinam
From the Department of Urology, Regional Institute of Medical Sciences (RIMS), Imphal, Manipur, India. |
|
|
|
|
|
Corresponding Author:
|
|
Dr. Bijit Lodh
Email: drblodh@yahoo.co.in |
|
|
|
|
|
|
|
|
Received:
26 JUNE 2013 |
Accepted:
22-JULY-2013 |
Published Online:
05-AUG-2013 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
Prostate cancer is one of the most common and slow growing malignancy among older males. Because of its origin in the peripheral zone, the majority of the patients present later in the course. Common symptoms associated with prostate carcinoma include lower urinary tract symptoms (LUTS), back pain and anaemia. The pathologic fracture secondary to prostate carcinoma is relatively rare because of its blastic nature of metastatic deposit. We have presented such case for its atypical presentation and for the requirement of a multidisciplinary approach. A 80 year old male with fracture right femur referred to urology OPD for LUTS. He was found to have prostate cancer with MRI showing heterogenous signal intensity area suggestive of metastatic bony deposit in the proximal aspect of right femur with surrounding soft tissue involvement and subtrochenteric fracture. MRI guided biopsy showed osteoblastic metastasis. The patient was treated in a team approach involving orthopaedic surgeon, urologist and medical oncologist. |
|
|
|
|
|
Keywords :
|
Back Pain, Femoral Fractures, Prostatic Neoplasms, Fractures, Orthopedics.
|
|
|
|
|
|
|
|
|
|
|
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff989e03000000f901000001000a00 6go6ckt5b5idvals|223 6go6ckt5b5idcol1|ID 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
The proportion of prostate cancer (CaP) diagnosed at a loco-regional sage is much higher than the distant stage, and it is 91-93% and 4-6% respectively [ 1]. Therefore, the majority of cases produce few symptoms in the early course, often similar to those of benign prostatic hyperplasia, and may go unnoticed. Nevertheless, prostate cancers do metastasize and bone is the most common site of distant metastasis. The exact incidence of bone metastasis at diagnosis is not known. Norgaard M et al, have reported an incidence of almost 3% [ 2]. In most cases, a difficulty in micturition is the first and only symptom. Back pain, anaemia and disability may also result from metastatic bone disease (MBD). Pathological femur fracture as the first clinical manifestation is very rare, because of the characteristic osteoblastic metastatic deposit. Herein, we report and briefly elaborate on the management of such uncommon presentation.
Case Report
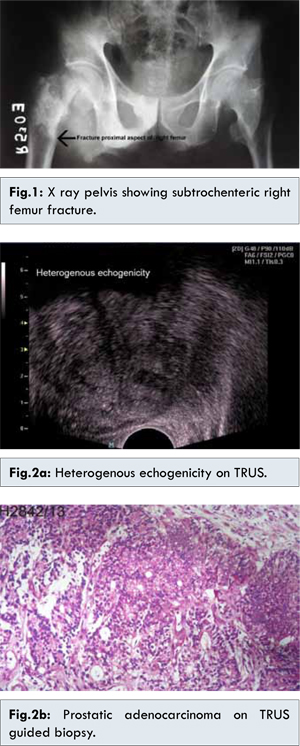
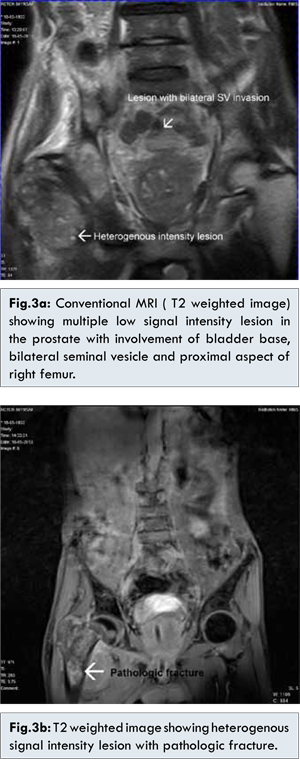
An 80 year old male with a fracture proximal aspect of right femur was admitted in the orthopaedic ward following a minor fall event at home [Fig.1]. He was referred to urology OPD for persistent lower urinary tract symptoms (LUTS). Laboratory investigations showed 8-10 pus cells on urine examination and haemoglobin of 9 gm/dL. Digital rectal examination (DRE) revealed hard nodular prostate with grade III enlargement. On Trans rectal ultrasound (TRUS) prostate volume was 64 ml and heterogeneous echogenicity noticed throughout the prostate [Fig.2a]. The patient was investigated for serum total prostate specific antigen (PSA) and percentage of free PSA, which was 200 ng/ml and 13% respectively. TRUS guided biopsy revealed prostatic adenocarcinoma, Gleason grade 4+3 [Fig.2b]. The patient was staged with whole body MRI, which shows multiple lower signal intensity lesions in the prostate with involvement of bladder base and bilateral seminal vesicle [Fig.3a]. There was also evidence of heterogeneous signal intensity lesion in the proximal aspect of right femur with subtrochanteric femoral fracture and soft tissue involvement [Fig. 3a,3b]. The patient was subjected to MRI guided biopsy of the femoral lesion that showed an osteoblastic metastatic deposit. He required a team approach including orthopaedic surgeons, urologist and medical oncologist. Subtrochanteric fracture was treated with internal fixation by Jewett nail-plate followed by immobilization. As a first line treatment for metastatic prostate cancer, we have started androgen deprivation therapy (ADT). In our case, androgen ablation was achieved in combination with GnRH analogue (Inj. leuprolide, 7.5 mg subcutaneous monthly) and antiandrogen (Tab. Bicalutamide, 50 mg once a day). External beam radiotherapy (single fraction of 8 Gy) was considered for bone pain and for prevention of fixation loss. During the one month follow-up period, a drop in serum total PSA value (200 to 167 ng/ml) and satisfactory improvement in general condition was noticed. The patient was planned to follow-up every 3 months for the first year and every 6 months thereafter.
Discussion
Metastatic bone disease (MPD) is associated with poor survival and has a detrimental effect on the quality of life. Even though prostate cancer (CaP) is considered localized; there is a high proclivity for skeletal metastasis, approximately 90% [ 3]. The bone involved most frequently are lower lumbar vertebrae and pelvis with a relatively lower incidence of femur head, rib case and skull involvement [ 4]. Metastatic disease secondary to CaP are characterized by both osteoblastic and osteoclastic, but the relative amount of blastic activity exceeds that of the clastic and dense bone formation is the net result. Again, pure lytic lesions are prone to pathologic fracture in comparing to pure blastic and mixed lytic or blastic lesions. Therefore, bone pain rather than pathologic fracture is the expected presentation of advanced CaP. In our case, patient had minimal symptoms with respect to bone pain and LUTS, but he did not seek medical attention until he manifested with subtrochanteric femur fracture. Traditionally, the 99mTc bone scintigraphy is considered the standard method for detection of skeletal metastases. Isotope scanning is more sensitive than radiography for detection of most metastases, but suffers from a lack of specificity. Thus a positive bone scan may confirm a finding, but a negative scan does not exclude a metastasis [ 5].
MRI is generally considered to be the most accurate imaging method for the local staging of prostate cancer [ 6]. It is also highly sensitive for detecting bone metastasis (BM) in cancer patients. The superiority of MRI lies in its ability to identify BM at an early stage, before host reaction of the osteoblasts becomes visible [ 7, 8]. A meta-analysis of published studies showed that whole-body MRI had a sensitivity and specificity =90% for detection of bone metastases [ 9]. We have used a whole body MRI to stage the disease. Although cost may be a limiting factor in staging the disease with whole body MRI. Treatment of pathologic fracture may greatly differ from normal fracture and depends on the general condition of the patient and pattern of fracture. Internal fixation with an implant is generally preferred, because the underlying lesion may continue to erode the bone without promoting healing. Postoperative external beam radiotherapy (EBRT) can significantly reduce disease progression and subsequent loss of fixation [ 10]. In our case, subtrochanteric fracture was treated with internal fixation by Jewett nail-plate followed by complete immobilization and EBRT. Currently, no treatments can cure advanced CaP. In clinical practice, ADT is recommended as the initial treatment for metastatic disease. However, almost all patients eventually develop castration-resistant prostate cancer (CRPC) and thus chemotherapy becomes the first line of therapy thereafter [ 11, 12]. Hormonal therapy in combination of a GnRH agonist with an antiandrogen is usually preferred over monotherapy [ 13]. In our case androgen deprivation therapy was in accordance with standard protocol. This case, was addressed in a team approach, where orthopaedic surgeon, Urologist ad medical oncologist was involved.
Conclusion
Although unusual, metastatic bone disease secondary to prostate carcinoma must be considered as an antecedent cause of femur fracture sustained following the minor fall event. Nevertheless, multidisciplinary approach is the key to success in this group of patient.
References
- Howlader N, Noone AM, Krapcho M, et al., eds.: SEER Cancer Statistics Review, 1975-2009 (Vintage 2009 Populations). Bethesda, Md: National Cancer Institute, 2012. Also available online. Last accessed May 23, 2013.
- Norgaard M, Jensen AO, Jacobsen JB, Cetin K, Fryzek JP, Sorensen HT. Skeletal related events, bone metastasis and survival of prostate cancer: a population based cohort study in Denmark (1999 to 2007). J Urol. 2010;184:162-167.
- Robert LV, Eva C. Targeting Factors Involved in Bone Remodeling as Treatment Strategies in Prostate Cancer Bone Metastasis. Clin Cancer Res. 2006;12:6285s.
- David E. The prostate and seminal vesicle. In: William NS, editor. Bailey & Love’s Short Practice of Surgery, 25th ed. London: Edward Arnold Ltd; 2008. pp.1355.
- Rybak LD, Rosenthal DI. Radiological imaging for the diagnosis of bone metastases. Q J Nucl Med. 2001;45:53-64.
- Futterer JJ. MR imaging in local staging of prostate cancer. Eur J Radiol. 2007;63:328–334.
- Eustace S, Tello R, DeCarvalho V, Carey J, Wroblicka JT, Melhem ER, et al. A comparison of whole-body turboSTIR MR imaging and planar 99mTc-methylene diphosphonate scintigraphy in the examination of patients with suspected skeletal metastases. American Journal of Roentgenology. 1997;169:1655–1661.
- Gosfield E, Alavi A, Kneeland B. Comparison of radionuclide bone scans and magnetic resonance imaging in detecting spinal metastases. Journal of Nuclear Medicine. 1993;34: 2191–2198.
- Wu LM, Gu HY, Zheng J, Xu X, Lin LH, Deng X, et al. Diagnostic value of whole-body magnetic resonance imaging for bone metastases: a systematic review and meta-analysis. J Mag Reson Imaging. 2011;34:128–135.
- Jacofsky DJ, Haidukewych GJ. Management of pathologic fractures of the proximal femur: state of the art. J Orthop Trauma. 2004;18:459-469.
- Carles J, Castellano D, Climent MÁ, Maroto P, Medina R, Alcaraz A. Castration-resistant metastatic prostate cancer: current status and treatment possibilities. Clin Transl Oncol. 2012;14:169-176.
- Shore ND, Abrahamsson PA, Anderson J, Crawford ED, Lange P. New considerations for ADT in advanced prostate cancer and the emerging role of GnRH antagonists. Prostate Cancer Prostatic Dis. 2013;16:7-15.
- Trachtenberg J. Emerging Pharmacologic Therapies for Prostate Cancer. Rev Urol. 2001;3:23–28.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
Lodh B, Meitei SK, Amer B, Sinam RSPathologic Femur Fracture: An Unusual First Clinical Manifestation of Prostate Carcinoma.JCR 2013;3:254-258 |
|
Lodh B, Meitei SK, Amer B, Sinam RSPathologic Femur Fracture: An Unusual First Clinical Manifestation of Prostate Carcinoma.JCR [serial online] 2013[cited 2026 Jan 2];3:254-258. Available from: http://www.casereports.in/articles/3/2/pathologic-femur-fracture.html |

|
|
|
|
|