|
|
|
|
|
Pulmonary Tumor Thrombotic Microangiopathy by Lung Adenocarcinoma
|
|
|
Ikutarou Furuno1,2, Seiya Tanaka1, Hiromichi Ueno2, Hisaharu Ooe2, Yugo Yoshida3, Takashi Harada1, Yukikazu Awaya3, Hiromi Tasaki1, Tatsuro Shimokama4
From the Department of Cardiology1and Respirology3, Kitakyushu Municipal Yahata Hospital, 4-18-1 Nishihon-machi, Yahatahigashi-ku, Kitakyushu, Japan; The Second Department of Internal Medicine2, School of Medicine, University of Occupational and Environmental Health, Kitakyushu, Japan; and Department of Pathology4, Steel Memorial Yawata Hospital, Kitakyushu, Japan. |
|
|
|
|
|
Corresponding Author:
|
Dr. Seiya Tanaka
Email: seiya-t@med.uoeh-u.ac.jp |
|
|
|
|
|
|
|
|
Received:
11 JUNE 2013 |
Accepted:
21-JUN-2013 |
Published Online:
25-JUL-2013 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
Pulmonary tumor thrombotic microangiopathy, which was established as a disease entity by von Herbay et al, is an uncommon cancer-related complication. The most common disease associated with pulmonary tumor thrombotic microangiopathy is poorly differentiated adenocarcinoma of the stomach, and cancers other than gastric cancers are very rare. We present a case of pulmonary tumor thrombotic microangiopathy caused by lung adenocarcinoma which was found in a 61-year-old Japanese woman. She was taken suffering from general fatigue without any history of cancers. Two-days after admission she suddenly complained of dyspnea and succumbed to pulmonary hypertension. Postmortem autopsy revealed that lung adenocarcinoma with multiple liver metastasis and intimal proliferation of pulmonary small arteries with or without tumor emboli, which were characteristics of pulmonary tumor thrombotic microangiopathy.
|
|
|
|
|
|
Keywords :
|
Adenocarcinoma, Pulmonary Hypertension, Lung Neoplasms, Liver, Dypnea.
|
|
|
|
|
|
|
|
|
|
|
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff547f03000000f001000001001000 6go6ckt5b5idvals|218 6go6ckt5b5idcol1|ID 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
Pulmonary tumor thrombotic microangiopthy (PTTM) is a rare complication of malignant disease, which was first reported by von Hearbay et al [ 1]. An antemortem diagnosis of PTTM is extremely difficult, because the findings on chest computed tomography are very trivial or non-specific, and the patient rapidly deteriorates to death. Its histopathological characteristic is intimal proliferation in pulmonary small arteries and arterioles with or without tumor emboli, resulting in vascular stenosis. The most common disease associated with PTTM is poorly differentiated adenocarcinoma of the stomach, and carcinomas other than gastric carcinomas are very rare. We here report a postmortem autopsy case of PTTM caused by lung adenocarcinoma with multiple liver metastasis.
Case Report
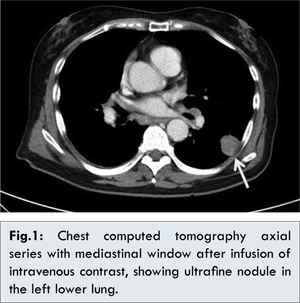
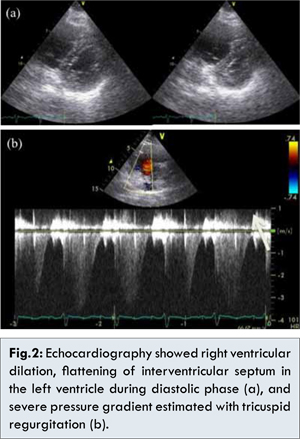
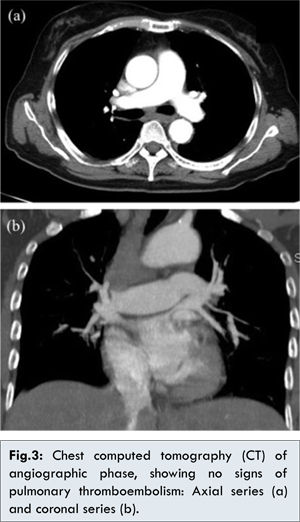
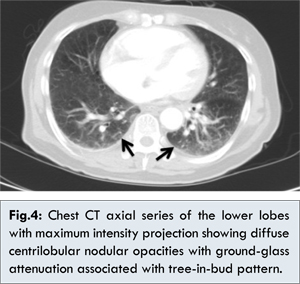
The patient was a 61-year old Japanese woman who presented with general fatigue and loss of appetite lasting for 2 weeks. There was no significant past history. She was suffering from general fatigue with mild hypoxia with 90% of oxygen saturation in the room air. A chest computed tomography (CT) showed a moderate fine nodule attached to the chest wall in the left lower lung [Fig.1]. Laboratory tests revealed that elevated serum carcinoembryonicantigen (CEA) (174.7 ng/mL; range < 5.0) and cytokeratin 19 fragment (CYFRA) (310 ng/mL; range <3.5). A bronchoscopy was planned to be performed. However, 2-days after admission, her respiratory condition suddenly deteriorated with severe hypoxia. No abnormal breath sounds were heard on auscultation of the lung fields. Routine biochemistry tests were normal except for elevated plasma-fibrin degradation products (P-FDP) (123.7 µg/mL; range < 5.0) and strongly positive D-dimer (56.16 µg/mL; range <1.0). Transthoracic echocardiography indicated severe pulmonary hypertension with tricuspid regurgitation; estimated gradient pressure was approximately 60 mmHg [Fig. 2]. Due to clinical suspicion of pulmonary thromboembolism, she underwent contrast-enhanced CT of her chest, pelvis and thighs. Although the angiographic phase did not present any signs of pulmonary thromboembolism, the CT scan showed signs of acute cor pulmonale characterized by increased right heart chamber dimensions [Fig.3]. In the lung window, the CT scan showed diffuse centrilobular nodular opacities with ground-glass attenuation, associated with a tree-in-bud disseminated through her lung [Fig.4]. Her respiratory condition abruptly worsened to the bottom. She died on the third day after admission.
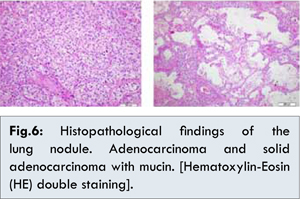
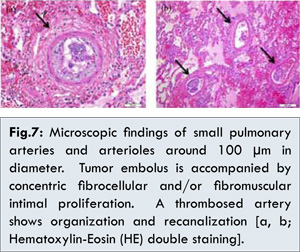
At autopsy gross examination identified a yellowish-white nodule of 2 cm in diameter with pleural invasion in the left lower lobe [Fig.5]. Histopathological examination of the lung nodule showed poorly differentiated solid adenocarcinoma with mucin [Fig.6]. In all the other lung lesions prominent fibromuscular and/or fibrocellular intimal proliferation of small arteries and arterioles around 100 µm in diameter with or without tumor emboli, which caused marked luminal stenosis, was identified [Fig.7]. These characteristics are consistent with PTTM caused by lung adenocarcinoma.

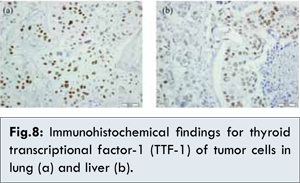
Metastatic adenocarcinoma was identified diffusely in the liver. The immunohistochemical analyses revealed that the tumor cells both in liver and lung were positive for thyroid transcriptional factor -1 (TTF-1) [Fig.8].
 Discussion
Discussion
We here report a case of pulmonary tumor thrombotic microangiopathy (PTTM) caused by lung adenocarcinoma which was found in a 61-year-old Japanese woman. The patient developed rapidly progressive and fatal pulmonary hypertension. Postmortem autopsy revealed that lung adenocarcinoma with multiple liver metastasis and intimal proliferation of pulmonary small arteries with or without tumor emboli, which were characteristics of pulmonary tumor thrombotic microangiopathy.
PTTM is a very rare complication of malignancies commonly detected after death. It was first reported by von Herbay and his colleagues as a diffuse myofibroblast proliferation of small pulmonary arteries that cause severe pulmonary hypertension, leading cardiopulmonary failure and sudden death [ 2- 6]. From the clinical point of view PTTM manifests with signs and symptoms of pulmonary hypertension which indicate progressive dyspnea, cough and hypoxia, as our patient presented. A cardiac evaluation may find signs of right-sided heart failure on electrocardiography and echocardiography. Deterioration inclinical condition occurs rapidly and patient generally expires before diagnostic confirmation and treatment [ 7].
Histopathologically PTTM is characterized by wide spread tumor embolism, microthrombi, and fibrocellular intimal hyperplasia of small pulmonary arteriesand arterioles [ 1, 2]. Diffuse vascular occlusion in patients with PTTM results in increased pulmonary vascular resistance. Diffuse centrilobular nodular and a tree-in-bud pattern on chest CT is caused by the dilation and plugging of small airways by mucus and inflammatory material, which are often seen in patients with small airway disease. This pattern is seen in the present case and also in a few cases with PTTM [ 8, 9]. This pattern might be the sign of a variety of pulmonary vascular abnormalities, including pulmonary tumor embolism and PTTM.
To best of our knowledge, only four cases of PTTM caused by lung carcinoma have been reported [ 1, 10]. The histopathological typing of these cases is adenocarcinoma, as in the present case. Herbay et al reported that 19 of 21 carcinomas with PTTM (90.5%) were adenocarcinomas [ 1]. The reason why PTTM is more frequently associated with gastric cancers than non-gastric cancer and mostly associated with adenocarcinoma is unknown. In our case, bile duct adenocarcinoma is another candidate of diagnosis considering adenocarcinomais spread diffusely in her liver. However, consistency of positive TTF-1 between her lung and liver suggested primary and metastasis of adenocarcinoma.
PTTM rapidly progresses and is in most cases fatal since almost all cases die within a week from onset. It is very important to consider the possibility of PTTM before the appearance of pulmonary hypertension. Katayama et al reported that antemortem diagnosis of PTTM is made prior to the development of pulmonary hypertension which responded to chemotherapy [ 11].
Conclusion
In conclusion, it is important to suspect PTTM as a differential diagnosis for rapidly progressing respiratory failure, not only in patients with cancer, but also in patients without a history of cancer. The early diagnosis of PTTM may lead to appropriate management.
References
- von Herbay A, Illes A, Waldherr R, Otto HF. Pulmonary tumor thrombotic microangiopathy with pulmonary hypertension. Cancer. 1990;66:587-592.
- Chinen K, Tokuda Y, Fujiwara M, Fujioka Y. Pulmonary tumor thrombotic microangiopathy in patients with gastric carcinoma: an analysis of 6 autopsy cases and review of the literature. Pathology, research and practice. 2010;206:682-689.
- Malani AK, Gupta C, Kutty AV, Betlej T. Pulmonary tumor thrombotic microangiopathy from metastatic gallbladder carcinoma: an unusual cause of severe pulmonary hypertension. Digestive diseases and sciences. 2007;52:555-557.
- Sakashita N, Yokose C, Fujii K, Matsumoto M, Ohnishi K, Takeya M. Pulmonary tumor thrombotic microangiopathy resulting from metastatic signet ring cell carcinoma of the stomach. Pathology international. 2007;57:383-387.
- Chinen K, Kazumoto T, Ohkura Y, Matsubara O, Tsuchiya E. Pulmonary tumor thrombotic microangiopathy caused by a gastric carcinoma expressing vascular endothelial growth factor and tissue factor. Pathology international. 2005;55:27-31.
- Chinen K, Fujino T, Horita A, Sakamoto A, Fujioka Y. Pulmonary tumor thrombotic microangiopathy caused by an ovarian cancer expressing tissue factor and vascular endothelial growth factor. Pathology, research and practice. 2009;205:63-68.
- Keenan NG, Nicholson AG, Oldershaw PJ. Fatal acute pulmonary hypertension caused by pulmonary tumour thrombotic microangiopathy. International journal of cardiology. 2008;124:e11-13.
- Tack D, Nollevaux MC, Gevenois PA. Tree-in-bud pattern in neoplastic pulmonary emboli. AJR American journal of roentgenology. 2001;176:1421-1422.
- Franquet T, Gimenez A, Prats R, Rodriguez-Arias JM, Rodriguez C. Thrombotic microangiopathy of pulmonary tumors: a vascular cause of tree-in-bud pattern on CT. American journal of roentgenology. 2002;179:897-899.
- Uruga H, Morokawa N, Enomoto T, Takaya H, Miyamoto A, Kishi K, et al. A case of pulmonary tumor thrombotic microangiopathy associated with lung adenocarcinoma diagnosed by CT-guided lung biopsy. Nihon Kokyuki Gakkai zasshi = the journal of the Japanese Respiratory Society. 2008;46:928-933.
- Kayatani H, Matsuo K, Ueda Y, Matsushita M, Fujiwara K, Yonei T, et al. Pulmonary tumor thrombotic microangiopathy diagnosed antemortem and treated with combination chemotherapy. Intern Med. 2012;51:2767-2770.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
Furuno I, Tanaka S, Ueno H, Ooe H, Yoshida Y, Harada T, Awaya Y, Tasaki H, Shimokama TPulmonary Tumor Thrombotic Microangiopathy by Lung Adenocarcinoma.JCR 2013;3:232-236 |
|
Furuno I, Tanaka S, Ueno H, Ooe H, Yoshida Y, Harada T, Awaya Y, Tasaki H, Shimokama TPulmonary Tumor Thrombotic Microangiopathy by Lung Adenocarcinoma.JCR [serial online] 2013[cited 2025 Oct 16];3:232-236. Available from: http://www.casereports.in/articles/3/2/pulmonary-tumor.html |

|
|
|
|
|