Introduction
Anorectal malformations comprise a wide spectrum of diseases, which can affect both genders, and involve the distal anus and rectum as well as the urinary and genital tracts. They occur in approximately 1 in 5,000 live births and are more common in females [1]. Adult presentation of this condition is rare since most cases are diagnosed and corrected at birth with increasing awareness and advances in pediatric surgery. The delayed diagnosis of such malformations can be associated with development of intractable constipation or there could be social and psychological morbidity due to lack of control over defecation and passage of flatus and difficulties in sexual functioning.
Case Report
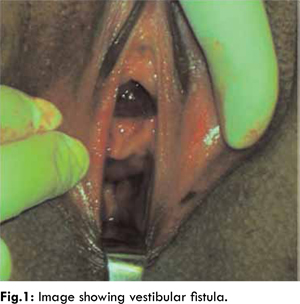
A 24 years old female presented with complaints of constipation. She was diagnosed with low anorectal malformation at birth and had undergone right transverse colostomy for same with a plan of staged anorectoplasty. However, colostomy closed spontaneously and patient continued to pass stools through the vestibular fistula. On general examination, her weight was 35 kg, and no other congenital abnormalities were found. Respiratory and cardiac examinations revealed normal findings. On per abdominal examination, scar of the right transverse colostomy was found, while the abdomen was soft without any abnormality. Local examination revealed absence of anal opening at the normal site, and presence of an anomalous anal opening in the vestibule. The fistulous opening was small in size. The urethral opening was normal, and on per vaginal examination, the uterus was normal in size and anteverted in position [Fig.1]. Routine hematological and biochemical investigations were normal with no abnormality noticed on ultrasonography of abdomen.
Pre-operatively, a thorough bowel preparation was done. Anterior sagittal anorectoplasty was performed in lithotomy position after placing a urethral catheter. The vestibular fistulous opening was dissected, after placing stay sutures all around the fistulous opening. A plane was created between the vagina and the rectum by meticulous dissection. Perineal body reconstruction was done, and a neo-anus was created. A continent neo-anus with an excellent functional and aesthetic improvement was the result [Fig.2]. The patient was managed post-operatively with intravenous fluids and antibiotics for 7 days. Oral feeding was started on the 7th day post-operatively.
The patient was discharged on the 10th day post-operatively, on full diet, a mild laxative and local wound care and neo-anal dilatation. Follow-ups were done at one month, three months and one year after the surgical reconstruction of neoanus. Excellent anorectal function with aesthetic improvement was the result.
Discussion
All significant anorectal malformations are readily apparent on routine neonatal examination. For newborns with an anorectal anomaly, early treatment is crucial. However, illiteracy, lack of neonatal care and inappropriate medical facilities may lead to the persistence of this condition to adulthood or neglect of female child.
This patient was treated with a plan of staged surgical repair and a right transverse colostomy was done at birth. Due to illiteracy of her parents, she lost follow-up and continued to decompress through the vestibular fistula. With advancing age, she started getting constipation and presented for surgical reconstruction. Also an element of future normal sexual activity and reproduction was added at the time presentation for surgical correction. Menstrual history was normal. After investigations, anterior sagittal anorectoplasty was done creating neo-anus. Patient was taught local hygiene and was advised to avoid constipation with the help of dietary modifications and laxatives for three months. First follow-up after three months and second follow-up after one year revealed a continent supple neoanus of adequate size and normal bowel habits.
Patients of anorectal malformation have to cope up with long lasting physical, mental and social health domains. A female preponderance is observed. Degree of continence and psycho-social problems like sexual functioning are the two most important factors which determine the quality of their life [2]. Degree of continence can vary from diarrhea to constipation. Studies have shown that 60% have good continence, 24% have minor aberrations in anal function like occasional and/or slight smearing and 13% have difficulties in sexual function after reconstructive surgery [3].
Constipation is the major problem due to the late age at presentation and the consequent mega colon and mega rectum. However, with the proper use of laxatives and motivation, patients can achieve good anorectal function. It also leads to recurrent genital and urinary tract infections and may even lead to infertility. Delayed presenters also have inadequate weight gain and increased parental anxiety for a greater period of time [4,5]. Anterior or posterior sagittal anorectoplasty has been the operation of choice in terms of long-term anorectal function [6].
Conclusion
This case is a classical example of delayed presentation due to illiteracy and lack of access to advanced health care in rural areas. Careful neonatal examination at birth with early referral to advanced health care centers is very important as all low anorectal malformations can be managed in single stage, ideally by the age of six months, by anterior or posterior sagittal anorectoplasty. Correction of deformity beyond adolescence carries a bad influence on psycho-social and emotional functioning in these patients. Educating parents about the anomaly is an integral part of patient management.
References
- Rintala RJ. Congenital anorectal malformations: anything new? J Pediatric Gastroenterol Nutr 2009;48:S79-82.
- Pena A, De Vries PA. Posterior sagittal anorectoplasty: Important technical considerations. J Paediatric Surgery 1982;17:796-811.
- Sham M, Singh D, Phadke D. Anorectal malformations: Definitive management during and beyond adolescence. JIAPS 2012;17(3):120-123.
- Kim HL, Gow KW, Penner JG, Blair GK, Murphy JJ, Webber EM. Presentation of low anorectal malformations beyond the neonatal period. Pediatrics 2000;105:E68.
- Haider N, Fischer R. Mortality and morbidity associated with late diagnosis of anorectal malformations in children. Surgeon 2007;5:327-330.
- Husberg B, Rosenborg M, Frenkner B. Magnetic resonance imaging of anal sphincters after reconstruction of high or intermediate anorectal anomalies with posterior sagittal anorectoplasty and fistula-preserving technique. J Paediatric Surgery 1997;32:1436-1442.