|
|
|
|
|
IgG4 Related Disease-The Great Masquerade
|
|
|
Tony Ete, Sumantro Mondal, Debanjali Sinha, Kaushik Bhar, Shingamlung Kamei, Abhirup Bhunia, Sattik Siddhanta, Jyotirmoy Pal, Alakendu Ghosh
From the Department of Medicine, Institute of Post Graduate Medical Education and Research, Kolkata, India. |
|
|
|
|
|
Corresponding Author:
|
Dr. Tony Ete
Email: tetepete@gmail.com
|
|
|
|
|
|
|
|
|
Received:
05-MAR-2014 |
Accepted:
26-MAR-2014 |
Published Online:
30-APR-2014 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
IgG4 related disease is an uncommon disease that presents with diverse clinical manifestations. Interestingly the disease is a great masquerade of many other autoimmune and malignant conditions. Rare occurrence and varied clinical phenotype makes this disease a challenging one for the clinicians. Here we present a case of IgG4 related disease in a 50 year old female, who initially presented with low grade fever, sicca symptoms, eyelid swelling with proptosis along with bilateral salivary gland enlargement. Final diagnosis was made from characteristic histopathological finding and markedly elevated serum IgG4 level.
|
|
|
|
|
|
Keywords :
|
Autoimmune diseases, Immunoglobulin G, Salivary Glands, Exompthalmos, Phenotype.
|
|
|
|
|
|
|
|
|
|
|
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff8cc1050000002602000001000a00 6go6ckt5b5idvals|313 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
IgG4 related disease is a fibro-inflammatory condition with multisystem involvement. It is characterized by lympho-plasmacytic infiltrations in the affected organ with tumefactive lesions, storiform fibrosis, and, often but not always elevated serum IgG4 concentrations. The disease was not considered as a systemic condition until 2003. A lot many medical conditions that have long been viewed as conditions confined to single organs are now part of the spectrum of IgG4-related disease like Kuttner’s tumour, Riedel’s thyroiditis and Mikulicz’s syndrome depending on the key pathological feature present and perhaps this provides more insight into the pathophysiology. The disease usually occurs after 50 years of age and is seen predominantly in male.
Case Report
A 50 years old female without any history of diabetes or hypertension, presented with complaints of periorbital swelling bilaterally and bulging out of both eyes along with swelling in both sides of neck for five years. She had complaints of dryness of mouth and eyes for the last four years with a history of gritty sensation in eyes. The patient was also suffering from polyarthralgia for the last four years and low grade fever intermittent in nature for the last three years. The swelling around her eye was insidious in onset and slowly progressive in nature. Gradually she observed that there was prominence of white part of her eye due to bulging of both eyes. However, she had no difficulty in vision. The swelling around both side of the neck started insidiously and it was slowly progressive and painless. There was no history of significant loss of weight. She had no history of tuberculosis in the past. Examination revealed bilateral conjunctival injection, bilateral proptosis. There was no extraoccular muscle weakness, restriction in movement of eyeball or any bruit. Visual acuity was normal bilaterally. Enlargement of bilateral submental and submandibular glands were noted without any evidence of tenderness, lobulation or fixity to surrounding structures. The glands appeared firm in consistency. Indirect ophthalmoscopy and tonometry was normal. Examination of the other systems was unremarkable.
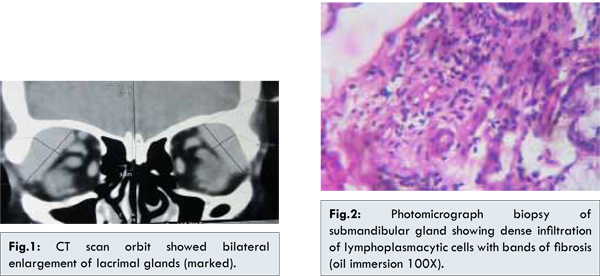
Routine investigations showed Hb: 12.6 g/dL, TLC: 7200/cumm, (N70L27M02E01), platelets were adequate, ESR: 30 mm, urea: 16 mg/dL, creatinine: 1.2 mg/dL, total proteins: 7.2 g/dL, albumin: 4.1 g/dL, globulin: 3.1 g/dL, SGOT: 13 U/L, SGPT: 19 U/L, alkaline phosphatase: 101 U/L, LDH: 427 U/L, Na: 141 meq/L, K: 3.3 mEq/L, HIV serology and thyroid function test were negative. Chest X-ray and ultrasonography of whole abdomen were normal without any evidence of retro peritoneal lymphadenopathy. Blood for ANA, anti SSA & SSB, cANCA were negative, serum ACE levels of 43.6 (8-65 U/L). CT scan orbit showed bilateral enlargement of lacrimal glands without any focal lesion [Fig.1]. CT scan thorax was normal. Bone marrow study showed normal findings. Schirmer’s test was positive. Lip biopsy report had no significant findings. Submandibular gland biopsy showed dense infiltration of lympho-plasmacytic cells with bands of fibrosis [Fig.2]. Following the biopsy report of submandibular gland, serum IgG4 was sent and it was found to be 3.5 gm/L. The patient was put on steroid at a dose of prednisone 0.6 mg/kg for 4 weeks followed by tapering to 5 mg/day over 3 to 6 months and advised for regular follow up. She showed signs of response in the form decrease in the size of the neck swelling and decrease in the bulge within weeks after starting the medication.
The main target organs in IgG4 related diseases are pancreas, bile ducts, salivary glands, lacrimal glands, mediastinal lymph nodes, retroperitoneum, aorta, lungs, and kidneys. It was first described to be associated with pancreatitis and hypergammaglobulinemia. The disease was later considered to be systemic in the year 2003 after extra pancreatic manifestations were found to be associated with autoimmune pancreatitis [1]. The lesion in pancreas and other organs in are characterized by lymphocytic infiltrate on a background of fibrosis morphologically similar to that seen in a case of idiopathic orbital inflammation [2,3]. IgG4 mainly affects men older than 50 years of age with a sex ratio of 3.7 to 5.7:1 [4]. The age of our patient also corresponds with this age but incidence in female is uncommon. No accurate prevalence data is available for IgG4 related disease. The disease has been reported mainly from Japan; where the prevalence of autoimmune pancreatitis is 8 per lac and the estimated incidence is 0.2 per lac [5]. Clinically the main presenting sign is a focal pseudotumoral swelling of an organ.Onset is usually subacute with no constitutional symptoms. Though disease onset was also subacute in our patient, presence of fever and arthralgia are not common for this disease. The clinical presentation of our patient simulated various other known conditions like sarcoidosis, Sjogren syndrome, thyroid ophthalmopathy, orbital pseudotumour, diffuse infiltrative lymphocytosis syndrome and lymphoma. It was very important for us to rule out all these conditions to come at a final diagnosis of IgG4 related disease, which is rather a much rarer one. Now a number of previously recognized conditions indicating the involvement of a particular organ like Miculicz’s syndrome, Kuttner’s syndrome, retroperitoneal fibrosis etc. has been kept under the single spectrum of IgG4 related disease. Experts in the international symposium in 2011 agreed that the name IgG4 related disease should be used throughout the world abandoning other names of past [6]. The cornerstone for the diagnosis of IgG4 related disease is histopathological examination.Not specific but elevated level of IgG4 in tissue and serum are helpful in diagnosing IgG4 related disease [7]. Histology should show dense lymphoplasmacytic infiltrate organized in matted and irregularly whorled pattern (storiform), obliterative phlebitis and a mild to moderate eosinophilic infiltration. Typical histopathological features and elevated serum IgG4 level were present in our patient. The lymphoplasmacytic infiltrate and IgG4 are not monoclonal, which rules out a lymphoproliferative syndrome. Probably, IgG4 production is a marker for a distinct inflammatory process due to a Th2 and T-regulatory immune response. The presence of eosinophils in the tissue sample supports a Th-2 response mediated by IL-5.IL-4, IL-10 and IL-13 which stimulates plasma cells to produce IgG4 may be causing the IgG4 excess [8]. The diagnosis is based on clinical, laboratory and pathological criteria. Clinical criteria includes swelling in one or more organs [8]. Laboratory evidence is serum IgG4 level greater than 1.35 gm/L [8]. Pathological criteria includes plasma cell and lymphocytic infiltration in the tissue, IgG4 positive plasma cells more than ten per high power field with an IgG4/IgG ratio greater than 40% and storiform fibrosis [9,10]. This patient had proptosis with enlargement of both submandibular and sublingual glands, sicca symptoms and constitutional symptoms. Sarcoidosis or Sjogren syndrome were the tempting initial diagnosis but careful evaluation ultimately led to the diagnosis of IgG4 related disease with dacryoadenitia and sialadenitis which has been further supported by dramatic response with steroids.
References
- Kamisawa T, Funata N, Hayashi Y, Eishi Y, Koike M, Tsuruta K, et al. A new clinicopathological entity of IgG4-related autoimmune disease. J Gastroenterol. 2003;38(10):982-984.
- Hsuan JD, Selva D, McNab AA, Sullivan TJ, Saeed P, O’Donnell BA. Idiopathic sclerosing orbital inflammation. Arch Ophthalmol. 2006;124(9):1244-1250.
- Jacobs D, Galetta S. Diagnosis and management of orbital pseudotumor. Curr Opin Ophthalmol. 2002;13(6):347-351.
- Kamisawa T, Kim MH, Liao WC, Liu Q, Balakrishnan V, Okazaki K, et al. Clinical characteristics of 327 Asian patients with autoimmune pancreatitis based on Asian diagnostic criteria. Pancreas. 2011; 40(2):200-205.
- Guma M, Firestein GS. IgG4-related diseases. Best Pract Res Clin Rheumatol 2012;26:425–438.
- Stone JH. IgG4-related disease: nomenclature, clinical features, and treatment. Semin Diagn Pathol 2012;29:177–190.
- Sah RP, Chari ST. Serologic issues in IgG4-related systemic disease and autoimmune pancreatitis. Curr Opin Rheumatol 2011;23:108-113.
- Palazzo E, Palazzo C, Palazzo M. IgG4-related disease. Joint Bone Spine. 2013 Jul 9. doi: pii: S1297-319X (13)00153-X. 10.1016/j.jbspin.2013.06.001. PubMed PMID: 23849464.
- Umehara H, Okazaki K, Masaki Y, Kawano M, Yamamoto M, Saeki T, et al. Comprehensive diagnostic criteria for IgG4-related disease (IgG4-RD), 2011. Mod Rheumatol. 2012;22(1):21-30.
- Deshpande V, Zen Y, Chan JK, Yi EE, Sato Y, Yoshino T, et al. Consensus statement on the pathology of IgG4-related disease. Mod Pathol. 2012;25(9):1181-1192.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
Ete T, Mondal S, Sinha D, Bhar K, Kamei S, Bhunia A, Siddhanta S, Pal J, Ghosh AIgG4 Related Disease-The Great Masquerade.JCR 2014;4:143-146 |
|
Ete T, Mondal S, Sinha D, Bhar K, Kamei S, Bhunia A, Siddhanta S, Pal J, Ghosh AIgG4 Related Disease-The Great Masquerade.JCR [serial online] 2014[cited 2025 May 11];4:143-146. Available from: http://www.casereports.in/articles/4/1/IgG4-Related-Disease-The-Great-Masquerade.html |

|
|
|
|
|