|
|
|
|
|
Intrauterine Contraceptive Device in Peritoneal Cavity Invading Sigmoid Colon
|
|
|
BC Shah, Sarang Degloorkar
From the Department of Surgery, Bhakti Vedanta Hospital, Srishti Complex, Mira Road East, Thane, Maharashtra-401017, India. |
|
|
|
|
|
Corresponding Author:
|
Dr. BC Shah
Email: vaishnavasevadasa@gmail.com
|
|
|
|
|
|
|
|
|
Received:
07-APR-2014 |
Accepted:
13-MAY-2014 |
Published Online:
05-JUN-2014 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
The intrauterine contraceptive device (IUCD) is a commonly used method of contraception for women. However, there is a rare but serious risk of migration into the myometrium and then into the peritoneal cavity. IUCD migration into bowel, bladder, omentum, abdominal wall has been reported. We report here, a rare case of an IUCD migrating through the uterus into the peritoneal cavity and subsequently invading into the sigmoid colon.
|
|
|
|
|
|
Keywords :
|
Intrauterine Devices, Intrauterine Device Migration, Uterus, Sigmoid colon, Peritoneal Cavity.
|
|
|
|
|
|
|
|
|
|
|
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff44c905000000de02000001000700 6go6ckt5b5idvals|325 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
Intrauterine contraceptive device (IUCD) is the most common method of contraception worldwide. It has been found to be very effective and more affordable despite some associated complications. Uterine perforation is the most serious complication of IUCD and has been reported at a frequency of 1-2 per 1000 [1]. Perforation can occur either as primary which occurs at the time of IUD insertion or more commonly, delayed. In 15% of patients when such perforation occurs, the adjacent organs are also involved. Involvement of intestine may result in obstruction, perforation, ischemia, mesenteric injury, strictures or fistulae [2]. Very few reports exist on IUCD being displaced into colon [2-4]. Hence, we are presenting here one such case encountered in our clinical practice.
Case Report
A middle aged woman of 35 years presented with inability to find the IUCD thread in vagina since few days. She had put copper -T (IUCD) in uterus around six months back by a local general practitioner. Per vaginal examination did not show the thread of IUCD in vagina. An ultrasound abdomen was carried out; it showed presence of IUCD in abdomen. The patient was explained that she needs to undergo surgery to remove the IUCD since it can cause complications. Possible complications (the chance of likely procedure on bowel or urinary bladder in case of invasion of IUCD in bowel or bladder like repair of bowel) of keeping IUCD in abdomen were explained to patient. Incidentally she had gall stones also. She was planned for laparoscopic cholecystectomy & IUCD removal.
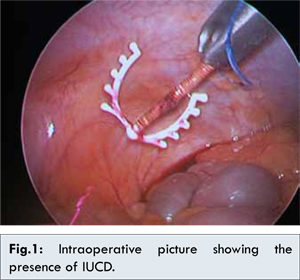
Bowel was prepared by proper laxative day prior to surgery in anticipation of any bowel procedure. During laparoscopic surgery, general anaesthesia was given. Patient was put in head low position so as to get good view of pelvis & dissection is easier. Urine catheterization was carried out. Three port entries were made. First port was put in umbilicus; two other ports were put in each iliac fossa. On initial laparoscopic examination findings were, uterus, ovaries & tubes were normal in appearance. There was no evidence of any abscess, collection in pelvis. One limb of IUCD was seen to invade wall of sigmoid colon, lying in peritoneal cavity. IUCD was invading antero-medial wall, of sigmoid colon. Few flimsy adhesions were present around IUCD. Adhesions were lysed carefully by sharp scissor dissection. Then linear incision was made on serosal wall of sigmoid colon at place where IUCD was embedded in it. IUCD was removed carefully from sigmoid wall after careful sharp scissor dissection. On careful examination only serosa & muscular layers of sigmoid was cut during dissection. Mucosa was not opened. The IUCD was then taken out from umbilical port. Few seromuscular sutures were taken over sigmoid to close partial rent which occurred during dissection.
The present report is a description of displacement of IUCD in peritoneal cavity invading the sigmoid colon. Uterine perforation and migration into the peritoneal cavity is rare but very serious complication of IUCD. Although perforation can occur during insertion of IUCD or secondary to uterine spasm, the entity has also been reported to occur during removal. The diagnosis is made when the absence of the string at the cervix is noted at routine gynecologic examination, and may be proved by radiological examination of the uterine cavity. Patient many a times may be asymptomatic, but a suspicion should arise when patients on IUCD present with abdominal pain, diarrhea and fever accompanied by the absence of IUCD string. In the present report, the patient was asymptomatic as she presented to the hospital at an early stage of perforation. The most common places for migration are the omentum, rectosigmoid colon, peritoneum, and bladder. Other places for IUD migration include the appendix, small intestine, adenexes, iliac veins, caecum, perirectal fat, retroperitoneal space, Douglas pouch, and ovaries at rare instances [5-6]. Following the entry of device into the peritoneal cavity, further symptoms depend on the organ that is affected. Ultrasound examination of the abdomen remains the diagnostic method of choice, but at times, when it does not reveal any intra-abdominal IUCD, X-ray abdomen should be carried out before considering that IUCD has expelled out. Factors affecting migration include uterine size, position, timing of insertion, congenital uterine anomalies and previous surgery. Insertion during the puerperium, presence of uterine involution, strong contractions and soft consistency of the uterus may increase risk of perforation [7]. Also, placing IUCD within 6 months postpartum and women with increased number of miscarriages has an increased risk [8]. Furthermore, faulty insertion technique and irregular physician follow-up increases the risk of uterine perforation. To prevent uterine perforation, the insertion should be performed by an experienced operator after a careful pelvic examination taking into consideration the uterine size, consistency and position. Patients with missing IUCD may present mostly within 6 months of insertion [9]. Removal of an IUCD that has migrated into or past the myometrium should be strongly considered even in asymptomatic patients because of the danger of migrating coil as well as risks from adhesion formation such as bowel obstruction and infertility [10,11].
Conclusion
Patients should be given IUCD under specialist supervision using appropriate technique, with regular follow-up and should be intervened as soon as possible in case of missing thread.
References
- Cicek N, Eryilmaz OG, Sarikaya E, Moraloglu O, Yavuz SM, Gulerman C. Clinical presentation, diagnosis, and management of intra-abdominally dislocated intrauterine devices. The New Journal of Medicine 2012;29:92-94.
- Arslan A, Kanat-Pektas M, Yesilyurt H, Bilge U. Colon penetration by a copper intrauterine device: a case report with literature review. Arch Gynecol Obstet 2009;279:395-397.
- Taras AR, Kaufman JA. Laparoscopic retrieval of intrauterine device perforating the sigmoid colon. JSLS 2010;14:453-455.
- Prabhu JK, Rani R, Nayak NK, Natarajan P. Migration of intrauterine contraceptive device into sigmoid colon. J Obstet Gynaecol 2010;30:526-527.
- Demir SC, Cetin MT, Ucunsak IF, Atay Y, Toksoz L, Kadayifci O. Removal of intra-abdominal intrauterine device by laparoscopy. Eur J Contracept Reprod Health Care. 2002;7:20-23.
- Ozdemir H, Mahmutyazicioglu K, Tanriverdi HA, Gundogdu S, Savranlar A, Ozer T. Migration of an intrauterine contraceptive device to the ovary. J Clin Ultrasound. 2004;32:91-94.
- Tosun M, Celik H, Yavuz E, Cetinkaya MB. Intravesical migration of an intrauterine device detected in a pregnant woman. Can Urol Assoc 2010;4:E141-E143.
- Peri N, Graham D, Levine D. Imaging of intrauterine devices. J Ultrasound Med 2007;26:1389-1401.
- Jimoh AAG, Balogun OR. Missing IUD Strings: Diagnosis and Management at Ilorin. Nig. Journal Med. 2004;13:118-123.
- Balci O, Capar M, Mahmoud AS, Colakoglu MC. Removal of intra-abdominal mislocated intrauterine devices by laparoscopy. J Obstet Gynaecol 2011;31:650-652.
- Organisation WH. WHO Mechanism of Action, Safety and Efficacy of Intrauterine Devices. Geneva: World Health Organisation; 1987; pp. 48-63.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
Shah BC, Degloorkar SIntrauterine Contraceptive Device in Peritoneal Cavity Invading Sigmoid Colon.JCR 2014;4:193-195 |
|
Shah BC, Degloorkar SIntrauterine Contraceptive Device in Peritoneal Cavity Invading Sigmoid Colon.JCR [serial online] 2014[cited 2025 Dec 24];4:193-195. Available from: http://www.casereports.in/articles/4/1/Intrauterine-Contraceptive-Device-in-Peritoneal-Cavity-Invading-Sigmoid-Colon.html |

|
|
|
|
|