6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1fff405050000008f02000001000600
6go6ckt5b5idvals|280
6go6ckt5b5idcol1|ID
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Introduction
Inversion of uterus is an unusual entity and may be classified as puerperal or obstetric and non-puerperal or gynecologic inversion [
1-
4]. Puerperal uterine inversion occurs with an incidence of 1 in 3,500 to 1 in 1,00,000 deliveries [
5]. But non-puerperal uterine inversion is very rare and many gynecologists are unlikely to encounter such a case during their life time [
6], this fact gives a clue as to its infrequent nature [
7].
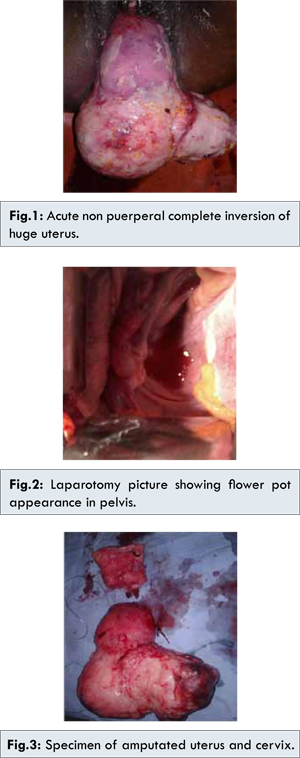
We report a case of acute non-puerperal complete inversion of the uterus with huge fundal myomas and carcinoma cervix (incidental diagnosis). This case is being reported for the safe surgical management with combined abdomino-perineal approach for acute non-puerperal complete inversion of uterus with huge myomas with severe infection and necrosis threatening to fall off by auto-amputation.
Case Report
A 50 year old woman para2, living2 got admitted as an emergency case with history of sudden onset of pain abdomen, mass per vaginum on lifting heavy weight and profuse vaginal bleeding. She gave history of foul smelling vaginal discharge since last one year. She attained menopause 3 years back and was alcoholic since 1 year. On examination she was anaemic, cachexic with normal vitals. Abdomen was soft and nontender. Vulval examination revealed large irregular, firm, hemorrhagic mass covered with necrotic areas measuring approximately 15x20 cms seen outside the introitus. There were two masses measuring 5x6 cm and 6x7 cm at the tip of the vulval mass [Fig.1]. Copious purulent foul smelling vaginal discharge was present and cervix was not visualized. On per vaginal examination, vagina was filled with mass, rent was felt in the posterior fornix and induration was present. On per rectal examination, uterus was not felt in position. Her hemoglobin was 5.8 gm%, other investigations were within normal limit. Ultrasound and CT scan could not be done. Patient could not walk due to threatening auto-amputation. She was given supportive treatment.
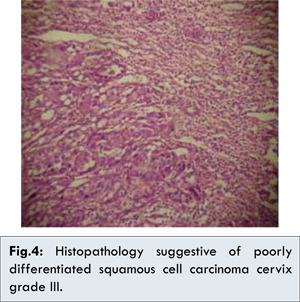
The mass was necrotic, hemorrhagic and because of the rent in the posterior fornix, auto amputation of the mass was anticipated. Patient was posted for the emergency surgery. Under combined epidural spinal anesthesia patient was placed in frog position. Abdomen was opened in layers. On laparotomy typical ‘flower pot appearance’ was noticed [Fig.2]. Ovaries, fallopian tubes and round ligaments were found in the cup shaped depression of uterine inversion. Infudibulo-pelvic ligaments and round ligaments were clamped, cut and ligated. Utero-vesical fold of peritoneum was cut and bladder mobilized downwards. To prevent pus entering the peritoneal cavity a perineal approach for incising the infected, necrotic mass at the level of the isthmus after ligating the descending cervical branch of uterine artery was done. Amputated stump was sutured with intermittent stitches for hemostasis and it was pushed inside the vagina and vagina was packed. Through abdominal approach cervical stump was pulled up, uterine vessels were visualized, clamped, cut and ligated, followed by uterosacral and Mackerodt ligaments and vaginal angles. Cervical stump was delivered out [Fig.3]. Biopsy was taken from the necrotic tissue in the posterior fornix. Peritoneal cavity, abdomino-pelvic organs and pelvic lymph nodes were palpated which were normal. The purpose of amputating the uterus by perineal approach was to avoid contamination of the peritoneal cavity. Usual surgical procedures for inversion would expose the peritoneal cavity to infection. The amputated mass weighed about 3 kgs. Specimen was sent for histo-pathological examination. This patient recovered within 24 hours without any evidence of pelvic peritonitis and she had uneventful post-operative period. Histopathology report came as poorly differentiated squamous cell carcinoma cervix grade III [Fig.4]. Three weeks later she was referred for radiotherapy.
Discussion
Most cases of uterine inversion are puerperal. Non-puerperal uterine inversions are extremely rare. From 1887 to 2006, 150 cases of non-puerperal inversions have been reported [
8]. Their etiology in order of frequency was submucus leiomyoma (71.6%), endometrial carcinoma (6.8%) and unspecified etiology (8%).
Takano et al summarized 88 reported cases of non-puerperal uterine inversion. 81(92%) of these were associated with uterine tumors, of which 20% were malignant. This emphasizes the need to perform biopsies prior to definitive treatment [
9,
10]. In this reported case, biopsy was done from the growth in the posterior fornix and from the uterine tumor, but we could not wait for the histopathology report before definitive treatment because emergency surgery had to be done due to threatening auto amputation.
Non-puerperal uterine inversion can also be classified into acute and chronic based on the onset and evolution. Usually non-puerperal inversions are chronic but 8.6% are presented as sudden onset. Symptoms of acute non puerperal uterine inversion are sudden onset of mass protruding through vagina, pain abdomen, vaginal bleeding and urinary disturbances. MRI and CT scan have been found to be useful diagnostic tools. MRI can show the characteristic image of uterine inversion. Lewin et al. reported that in T2-weighted MRI scans, a U shaped uterine cavity and a thickened and inverted uterine fundus on a sagittal image and a “bulls-eye” configuration on an axial image are signs indicative of uterine inversion [
11]. In this case, because symptoms were acute in onset and patient was in extreme agony due to necrosis, bleeding and threatening auto amputation requiring emergency intervention, we could not get either ultrasound or CT scan done to have accurate pre-operative diagnosis. However, with clinical findings and high index of suspicion patient was taken for surgery.
Most surgeons use abdominal approach for hysterectomy. We used combined abdominal and perineal approach for surgery. Initially at laparotomy to prevent an embolus due to pelvic congestion, both the infundibulo-pelvic ligaments were clamped and divided as the first step as suggested by Kopal [
12]. Since the mass was ischemic and necrotic, we avoided myomectomy from perineal route and reposition of the uterus as an usual procedure, to avoid intra-peritoneal infection. Instead we planned for amputation of the mass at the isthmus after ligating the vessels on either side. Later amputated cervix was removed through abdominal route.
S Uludag et al. demonstrated posterior hemi-dissection for non-puerperal uterine inversion caused by sub mucus fibroid, which could not be managed by standard procedures [
13]. Mathieu Auber
et al. managed a case of non-puerperal uterine inversion using combined laparoscopic and vaginal approach, where they ligated uterine arteries at their origin to completely devascularise the uterus facilitating identification of the limit between the ischemic reversed cervix and normal vascularised vagina [
14].
Conclusion
Non-puerperal uterine inversion is an unusual condition that most gynecologists will never encounter and thus has to be managed based upon little or no previous experience. In the presence of a tumor protruding from vagina or vulva we must consider uterine inversion. Non puerperal uterine inversion may be due to malignancy, therefore pre-operative diagnosis and histology are important for planning proper treatment and case follow up.
Acknowledgments
We would like to thank the patient and her relatives for giving us the permission to publish this case report.
References
- Barhmi R, Ferhati D, Nabil S. Complete non-obstetrical uterine inversion (in French). J. Gynaecol Obstet Biol Reprod. 1995;24:155-157.
- Gowri V. Uterine inversion and corpus malignancies: a historical review. Obstet. Gynecol Surv. 2000;55:703-707.
- GrischKe EM, Wallwiener D, Bastert G. Puerperal uterine inversion with covered uterine rupture (in German). Z Geburtshilfe Neonatal. 1999;203:123-125.
- Krenning RA, Dorr PJ, de Groot WH, de Goey WB. Non puerperal uterine inversion: Case report. Br J Obstet Gnecol. 1982;89:247-249.
- Abouleski E, Ali V, Joumaa B, Lopez L, Gupta D. Anaesthetic management of acute puerperal inversion. Br J Anaesth. 1995;75:486-487.
- M Winyoglee J, Simelela N, Marivate M. Non puerperal uterine inversions. A two case report and review of literature. Cent Afr J Med. 1997;43:268-271.
- Fofie CO, Baffoe P. Non-puerperal uterine inversion: A case report. Ghana Med J. 2010; 44(2):79-81.
- Bertrand S, Randriamarolahy A, Cucchi JM. Uterine inversion caused by a submucus leiomyoma. Clinical Imaging. 2011;35:478-479.
- Takano K, Ichikawa Y, Isunoda H, Nishida M. Uterine inversion caused by uterine sarcoma: a case report. Jpn J Clin Oncol. 2001;31:39-42.
- Nigam A, Jain S, Lal P. Twisted Ovarian Fibroma Mimicking as an Ectopic Pregnancy. Journal of Case Reports. 2013;3(1):64-67.
- Lewin JS, Bryan PJ. MR imaging of uterine inversion. J Comput Assist Tomogr. 1989; 13:357-359.
- Kopal S, Seckin NC, Turhan NO. Acute uterine inversion due to growing submucus myoma in an elderly woman: a case report. Eur J Obstet Gynecol Reprod Biol. 2001;99:118-120.
- Uludag S, Gezer A, Erkon S. Posterior hemidissection for non-puerperal uterine inversion. International Journal of Gynaecology and Obstetrics. 2006; 93:260-261.
- Mathieu Auber, BusmaDarwish, Anne Lefebure. Management of non-puerperal uterine inversion using combined laparoscopic and vaginal approach. American Journal of Obstetrics and Gynecology. 2011; 204(6):e7-e9.