Introduction
Jacob Arthur in Dublin in 1827 first coined the term “rodent ulcer” to describe what we now know as basal cell carcinoma [1]. It is the most common carcinoma of the skin [2,3]. Technically, the lesion is not a true carcinoma. A more correct pathologic description would be basal cell epithelioma [2]. Ultraviolet radiation is the most important and common cause of BCC. Syndromes like xeroderma pigmentosum and nevoid BCC syndrome are characterized by multiple basal cell carcinomas occurring in early age [3,4]. BCC arises from the basal cell layer of the skin. Advanced lesions may ulcerate and extensive local invasion of bone or facial sinuses may occur after many years of neglect or in unusually aggressive tumors explaining the past designation rodent ulcers [5]. Pigmented basal cell carcinoma is about 6% of all BCCs and has similar features to nodular BBC but with increased melanization. Here we present a case of pigmented basal cell carcinoma which is a very rare occurrence.
Case Report
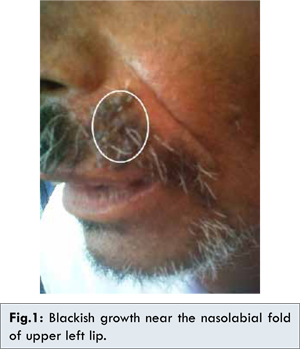
A 60 year old male patient reported with complaint of itching near left nasolabial fold region since 1 month. Patient was apparently alright 4 years back when he observed a small growth near the nasolabial fold. There was no history of exposure to radiation other than routine sun exposure. Initially the growth was small and later increased steadily. On clinical examination, the growth presented below the left nasolabial fold. It was irregular in shape and surface. Growth was approximately 3x1.5 cm in size and black in color [Fig.1]. Growth was soft to firm in consistency and non-tender on palpation. The skin around the growth was normal. On the basis of history and clinical examination, provisional diagnosis of basal cell carcinoma and melanoma was given. Incisional biopsy was performed and tissue was sent for microscopic evaluation.
Microscopic examination showed irregular covering of hyper-orthokeratinised stratified squamous epithelium [Fig.2a]. Underlying connective tissue consisted of epithelial islands of basaloid cells, typically having large hyperchromatic nuclei with little cytoplasm and few mitotic figures [Fig.2a,2b]. The peripheral cells of these islands showed palisading appearance. Melanin pigmentation was seen in basal and suprabasal layers of the overlying epithelium and within the islands [Fig.2a,2b]. The melanin pigment was confirmed by positive Fontana-Masson stain [Fig.2c]. Immunohistochemical analysis was done with S-100 and the result was negative [Fig.2d]. Thus on the basis of microscopy and immunohistochemical examination final diagnosis of pigmented variant of basal cell carcinoma was established.
Discussion
BCC may arise in skin damaged by sunlight, ionizing radiation, burn scars or vaccination scars. The risk of skin cancer is related to the amount of sun exposure and pigmentation in the skin [6]. In our case the patient was a farmer and used to spend most of his time in the open field.
BCC is believed by many to arise from pluripotential cells within the basal layer of the epidermis of follicular structures [1,4]. BCC occurs most frequently in the fourth decade of life or later but it has also been reported as occurring in younger persons. Male to female ratio is approximately 3:2 [4]. BCC is most frequently seen in the middle third of the face. Our patient was in his 7th decade with a lesion on the middle third of the face.
The subtypes of basal cell carcinoma are nodular basal cell carcinoma, pigmented basal cell carcinoma, cystic basal cell carcinoma, superficial basal cell carcinoma, micro-nodular basal cell carcinoma, morpheaform and infiltrating basal cell carcinoma. Nodular basal cell carcinoma is the most common variety of basal cell carcinoma. It begins as a small, slightly elevated papule with central depression. Pigmented basal cell carcinoma in addition to features seen in lesions of nodular BCC, contains increased brown or black pigment. Our case too showed all the features of a BCC along with increased pigmentation. Cystic BCC lesions are translucent blue-gray cystic nodules that may mimic benign cystic lesions. Superficial BCC presents as scaly patches or papules that are pink to red-brown in color often with central clearing. Superficial BCC is often found on the trunk and extremities, although 40% still occurs on the head and neck [7]. Micro-nodular BCC appears as yellow-white when stretched, whereas morpheaform and infiltrating basal cell carcinoma present as sclerotic plaques or papules. Ulceration, bleeding and crusting are uncommon. Both micro-nodular and morpheaform subtypes are aggressive in nature.
H and E stained sections of the biopsy specimen reveals an increase in melanocytes and melanin deposition in the basal layer, apart from the islands of basaloid cell proliferation, with peripheral palisading. Melanocytes proliferate within the tumor and the melanin that they produce causes the tumor to be pigmented.
The clinical features and histopathology indicated BCC, the presence of pigmentation made it necessary to rule out the possibility of melanoma. The HMB-45 and S-100 are currently the two most useful immunomarkers to identify melanocytes and melanomas. Anti-HMB-45 is regarded more specific but less sensitive than S-100 protein. It is very helpful in distinguishing the melanomas from other non-melanocytic malignancies. S-100 is expressed by cells derived from the neural crest. Lesions like melanomas, schwannomas and glioblastomas shows positivity for S-100. An immunohistochemistry with S-100 was thus done. In this case immunohistochemistry with S-100 showed negative result, thus ruling out melanoma.
Surgical excision is the treatment of choice for most primary BCCs. Mohs micrographic surgery (MMS) is recommended for larger BCCs of the face and those with more aggressive growth patterns. Intralesional injection of interferon alpha (IFN alpha) has also been shown to provide a safe and effective treatment alternative [2,8].
Conclusion
This report describes a rare variant of BCC,
diagnosed by histopathology and immunohistochemistry. The knowledge of histopathological features of pigmented basal cell carcinoma and its differentials can lead to correct diagnosis and allow for correct management of patient.
References
- Janjua OS, Qureshi SM. Basal cell carcinoma of the head and neck region: An analysis of 171 cases. J of Skin Cancer 2012;2012:943472.
- Zabbia G, Gulotta E, Clemente D, Napoli P, Tripoli M, Corradino B, et al. Basal Cell Carcinoma Arisen on Rhinophyma: Report of Four Cases. Journal of Case Reports 2013;3(2):299-303.
- Mehta V, Balachandran C. Pigmented basal cell carcinoma of skin successfully treated with 5% imicuimod cream. Indian Journal of Dermatol 2008;53:140-143.
- Bsoul SA, Terezhai GT, Moore WS. Basal cell carcinoma. Quintessence Int 2004;3:251-252.
- Neville BW, Damm DD, Allen CM, Bouquot JE. Oral and maxillofacial pathology. 2nd ed. Philadelphia (PA): WB Saunders; 2002.
- Ejaz A, Aurangzeb, Awan ZI, Bux H. Basal cell carcinoma involving the skin of breast- A rare site. JPAD 2006;16:49-51.
- Nakayama M, Tabuchi K, Nakamura Y, Hara A. Basal cell carcinoma of the head and neck. J of Skin Cancer 2011;1-9.
- Thissen MR, Neumann MH, Schouten LJ. Systemic review of treatment modalities for primary basal cell carcinomas. Arch dermatol 1999;135:1777-1883.