6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ffd434050000009f02000001000100
6go6ckt5b5idvals|286
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Introduction
Pulmonary sarcomatoid carcinomas (PSC) are a rare occurrence accounting for less than 1% of all non-small cell lung carcinomas (NSCLC). Patients commonly present with pulmonary symptoms such as chest pain, hemoptysis, cough and dyspnea. Distant metastasis is extremely common and these tumors tend to have a worse prognosis due to their aggressive and chemoresistant nature. We herein report a case of PSC to discuss clinical presentation, diagnosis, treatment modalities and prognosis of this rare condition.
Case Report
A 36 year old Caucasian male presented to the Emergency Department with a six-month history of right shoulder pain. Six months ago he was diagnosed with a pinched nerve and treated with anti-inflammatory medications. However, the pain progressively worsened and was now associated with right upper extremity weakness. The patient was unable to grip objects, lift his arm and noticed a sensation of numbness predominantly affecting the deltoid region. He also reported new onset bilateral lower extremity weakness, which interfered with his ability to ambulate. He reported a 30-pound weight loss and interrupted night sweats over the past few months. His wife also noticed increasing confusion and inappropriate response to questions. He denied having any chest pain, dyspnea, hemoptysis or headaches. Past medical history was unremarkable. He was a previous smoker with a 20 pack year smoking history. He denied any alcohol, or recreational drug use. He worked as a computer technician and had no previous exposure to asbestos or silica. On examination, his vital signs were within normal limits. He was breathing comfortably without accessory muscle use. Chest auscultation revealed decreased breath sounds in the right apex. Muscle strength was reduced in the right upper extremity and he had very weak right grip strength. The rest of the physical examination was unremarkable.
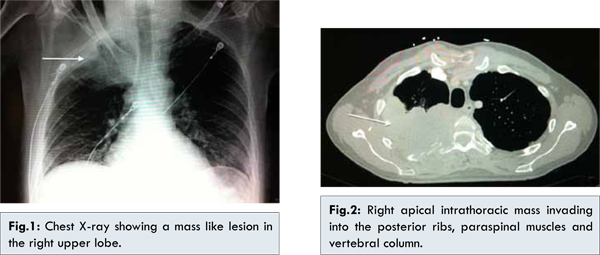
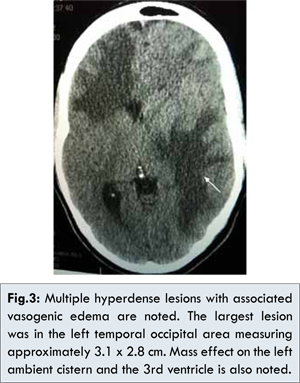
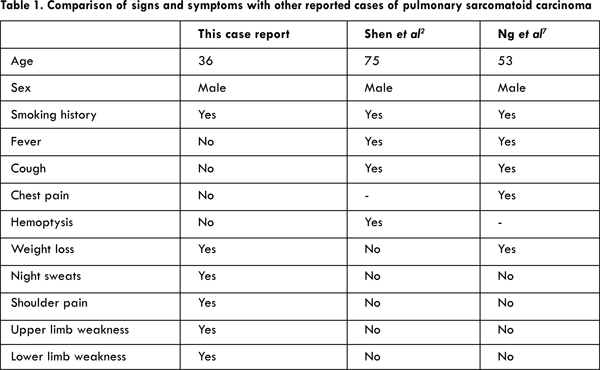
Full blood count and comprehensive metabolic panel were within normal range. Chest X-ray showed a dense focus of consolidation in the right upper lobe associated with volume loss and subpleural thickening in the apical region of the chest [Fig.1]. CT scan of the chest, abdomen, and pelvis showed a large heterogeneous attenuating mass within the apex of the right thoracic cavity that measured 10.8 x 7.4 x 6.3 cm with associated central necrosis [Fig.2]. There was destruction of the right 3rd and 4th ribs posteriorly as well as the right transverse process and vertebral bodies of the T3 and T4. The patient subsequently underwent a CT guided biopsy of the lung mass and the biopsy specimen was sent for histopathological analysis. It revealed a poorly differentiated carcinoma with giant cells and spindle cells. The tumor cells were positive for AE1:AE3 and CK7 while they are negative for p40, TTF-1, Napsin A, p63, WT1, calretinin, CK5/6, and CK20, supporting the diagnosis of PSC. Further imaging was performed for staging purposes. CT scan of the brain revealed multiple primary hyperdense lesions with surrounding vasogenic edema at the gray-white matter junctions [Fig.3]. MRI of the spine revealed tumor invasion of the inferior right brachial plexus and multilevel thoracic spinal cord compression (C6-T6) with enhancing epidural tumor.
The patient was commenced on levetiracetam 500 mg twice daily for seizure prophylaxis and dexamethasone 4 mg every 6 hours for reduction of vasogenic edema. His shoulder pain was well controlled using MS Contin 15 mg every 12 hours with morphine 5 mg every 4 hours for breakthrough pain. Radiation oncology was consulted and the patient was commenced on whole brain and lung radiation. Neurosurgery was consulted for management of the spinal cord compression however they did feel that the patient would benefit from any surgical intervention. A multidisciplinary team meeting was conducted and the patient was not deemed to be a suitable candidate for systemic chemotherapy due to his weak functional status and poor prognosis. Over the course of treatment his medical condition declined rapidly. The weakness and gait abnormalities he presented with progressed to total paraplegia with loss of sensation to approximately T3 level. As the disease progressed he had more difficulty with respirations and used his accessory and abdominal muscles. His mental status however remained intact with minor cognitive deficits. Unfortunately he died three weeks after initial diagnosis.
Discussion
Pulmonary sarcomatoid carcinomas (PSC) tumors are rare neoplasms of the lung accounting for 0.1-0.3% of all invasive lung malignancies. PSC of the lung are a form of NSCLC with poorly differentiated sarcoma like elements that are diagnostically challenging because they are uncommon and present with extensive histological heterogeneity [
9,
10]. There has been much controversy regarding their classification owing to their morphological diversity in the past. In 2004, WHO classified sarcomatoid carcinomas into five subgroups: pleomorphic carcinoma, spindle cell carcinoma, giant cell carcinoma, carcino-sarcoma and pulmonary blastoma [
4,
5,
9,
10]. PSCs predominantly occur in older males in their sixth or seventh decade and are associated with high degree of smoking. The exception to this is the pulmonary blastoma subtype of PSC, which demonstrates an equal preponderance for both men and women and tends to present earlier in
the fourth decade with a mean age of diagnosis of 35 [
4].
Sarcomatoid carcinomas tend to run a more aggressive course than other NSCLC, presenting as either a central or a peripheral lesion with a predilection for upper lobes [
1,
3]. Pleomorphic carcinomas and blastomas have a propensity to be situated in the peripheral lung with frequent chest wall involvement whereas a central location with endobronchial involvement is more often seen in carcino-sarcomas but radiological differentiation of these tumors is difficult [
3,
4,
10]. These are frequently bulky tumors ranging up to 16 cm in size, invading through the lung parenchyma, bronchial tree, mediastinal structures and chest wall resulting in clinical signs and symptoms that may be local or systemic in nature due to their high metastatic potential [
2-
4,
10]. PSC metastasize to the same anatomical sites as conventional NSCLC, especially to brain, bone, adrenals and liver but gastrointestinal, cardiac and renal metastatic disease has been noted as well [
2,
7].
Patients often present with respiratory symptoms including thoracic pain, cough and hemoptysis. The case reported here illustrates a unique case of PSC presenting in a young patient in the third decade remarkably with no respiratory symptoms. This is particularly rare, contrary to the usual expectation, as most PSC cases would present with respiratory symptoms to some degree. This is evident from comparison made between this case report and other case reports of PSC [Table 1].
The patient discussed here startlingly remained completely asymptomatic from a respiratory point of view despite bulky disease with an aggressively growing right upper lobe mass extending up to 10 cm. The patient instead solely presented with right upper limb and shoulder weakness and bilateral lower limb weakness as a consequence of metastatic disease to the brain and local invasion of brachial plexus. Within a short period of six months there was evidence of widespread metastatic disease and extensive lower cervical and thoracic spinal cord invasion resulting in debilitating disease and paraplegia. This again highlights the truly aggressive and malignant potential of PSCs. PSCs behave more aggressively than conventional NSCLC and generally portend a worse prognosis [
5,
6,
8]. In advanced stages, PSC rarely responds to chemotherapy and surgical resection is only chosen in very early stage disease but overall prognosis still remains dismal with high recurrence rates post-surgery [
8,
9].
Conclusion
In our opinion the case presented here truly represents an extraordinary and one of the most atypical forms of presentation of PSC and underscores the diagnostic challenges associated with PSCs. A concerted therapeutic approach aiming to alleviate tumor-related burden and preserving a meaningful quality of life remains paramount in treatment of aggressive carcinomas such as PSC.
References
- Huang S, Shen S, Li X. Pulmonary sarcomatoid carcinoma: a clinicopathologic study and prognostic analysis of 51 cases. World Journal of Surgical Oncology. 2013;11:252.
- Shen X, Lin Z, Lin Q, Ruan Z, Huang H, Ju C, Wang J. Pulmonary sarcomatoid carcinoma: a case report. Contemporary oncology (Wspolczesna Onkol). 2013;17(2):210-213.
- Pelosi G, Sonzogni A, De Pas T, Galetta D, Veronesi G, Spaggiari L, et al. pulmonary sarcomatoid carcinomas: a practical overview. International Journal of Surgical Pathology. 2010;18(2):103–120.
- Travis W. Sarcomatoid Neoplasms of the Lung and Pleura. Archives of Pathology & Laboratory Medicine. 2010;134(11):1645-1658.
- Franks T, Galvin J. Sarcomatoid Carcinoma of the Lung: Histologic Criteria and Common Lesions in the Differential Diagnosis. Archives of Pathology & Laboratory Medicine. 2010;134(1):49-54.
- Nakajima M, Kasai T, Hashimoto H, Iwata Y, Manabe H. Sarcomatoid carcinoma of the lung: a clinicopathologic study of 37 cases. Cancer. 1999;86:608-616.
- Ng SW, Lim CH, Wang CW, Chua YL. Primary pulmonary Sarcomatoid carcinoma with intracardiac extension: The Japanese Journal of Thoracic and Cardiovascular Surgery. 2006 54:416–419.
- Chaft JE, Sima CS, Ginsberg MS, Huang J, Kris MG, Travis WD, et al. Clinical Outcomes with Perioperative Chemotherapy in Sarcomatoid Carcinomas of the Lung. Journal of Thoracic Oncology. 2012;7(9):1400-1405.
- Park JS, Lee Y, Han J, Kim HK, Choi YS, Kim J, et al. Clinicopathologic outcomes of curative resection for sarcomatoid carcinoma of the Lung. Oncology. 2011;81:206–213.
- Litzky L. Pulmonary Sarcomatous Tumors. Archives of Pathology & Laboratory Medicine.2008;132(7):1104-1117.