|
|
|
|
|
Rapidly Progressive Dementia with Gait Ataxia
|
|
|
imurel azathioprinimurel 25 mg prix read imurel ja flunssa
From the Department of General Medicine, Pondicherry Institute of Medical Sciences, Ganapthychettikulam, Kalapet, Pondicherry, India. |
|
|
|
|
|
Corresponding Author:
|
Dr. Vijay Shanmugam G
Email: gvijais85@gmail.com
|
|
|
|
|
|
|
|
|
Received:
23-APR-2014 |
Accepted:
21-MAY-2014 |
Published Online:
20-JUN-2014 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
Choroid plexus papillomas are rare neoplasms that arise from choroid plexus epithelium. Most of these lesions appear in children, mainly located in the lateral ventricles. We report a case of a 40 year old male with rapidly progressive dementia and gait ataxia who was found to have choroid plexus papilloma. This condition predominantly affects children and is mostly located in the lateral ventricles. Choroid plexus papilloma accounts for 0.5% of all brain tumors in adulthood with very few case reports in the world which have depicted this unusual presentation.
|
|
|
|
|
|
Keywords :
|
Choroid Plexus, Papilloma, Dementia, Gait Ataxia, Brain Neoplasms.
|
|
|
|
|
|
|
|
|
|
|
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff58c905000000dd02000001000900 6go6ckt5b5idvals|330 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
Choroid plexus tumors are rare intra-ventricular papillary neoplasms derived from choroid plexus epithelium, which account for only between 0.4-0.6% of all intracranial and 2-3% of pediatric neoplasms [1]. Clinically, choroid plexus tumors tend to cause hydrocephalus and increased intracranial pressure [1]. Choroid plexus papillomas are twice as frequent as carcinomas [2]. It constitutes about 0.5 percent of the adult brain tumors [2].
Case Report
This 40 year old male a known case of psoriasis and type 2 diabetes mellitus, on methotrexate and metformin was brought with complaints of reduced word output and decline in immediate and recent memory with preserved remote memory over past 25 days. He also had swaying to either side while walking. His relatives gave history of reduced speech but no slurring or irrelevant speech. There was no history of fever or seizures or bowel and bladder involvement. Patient had no substance abuse but had a road traffic accident 6 months prior to the current admission. Neuroimaging done then was normal.
On examination, he was conscious, disoriented to time and place, and had reduced spontaneous speech. His Glasgow coma scale was 15/15 (E4M6V5). His attention was reduced and his mini-mental status examination revealed MMSE score of 23. His cranial nerve examination was normal. There was marked hypertonia with grade 4/5 power of upper limbs, and normal tone and power in lower limbs. He had an exaggerated left biceps and supinator reflexes with left sided Babinski positive. Cerebellar signs were present in both upper and lower limbs with gait ataxia.
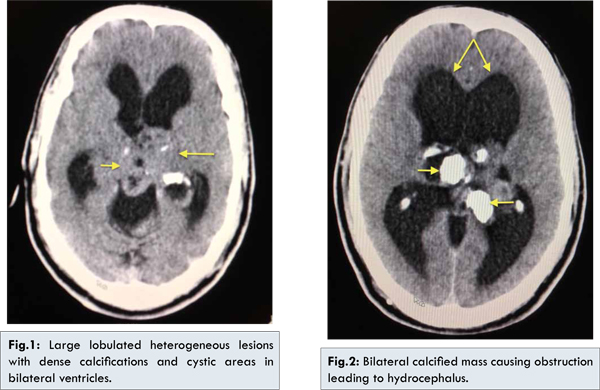
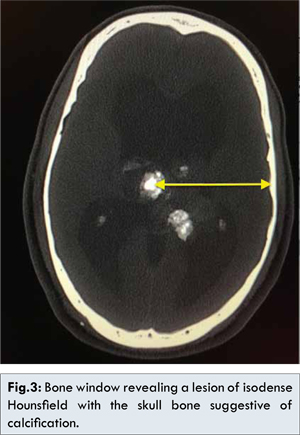
His blood panel revealed a normal study with normal electrolyte and liver enzyme levels. His retroviral status was negative. A computed tomography scan of brain revealed large lobulated heterogeneous lesions with dense calcifications and cystic areas in bilateral ventricles extending into the region of posterior third ventricle and pineal gland causing hydrocephalus suggestive of choroid plexus papilloma [Fig.1,2]. The bone window revealed an iso-dense Hounsfield unit of the hyper-dense region in the lesion when compared with the skull bone suggestive of calcification of the lesion [Fig.3]. Neurosurgery consult was taken and was advised surgery. However the patient was not willing for surgery and was referred to a neurorehabilitation centre.
Our case presented with one of the rare forms of neoplasms of the nervous systems. The presentation was deceiving and had various other differential diagnosis including normal pressure hydrocephalous and subdural hematoma and progressive supranuclear palsy. Moreover the clinical presentation in the form of rapidly progressive dementia and ataxia was also fairly uncommon.
Discussion
Neoplasms of the choroid plexus account for 0.4-0.6% of all intracranial tumors, 2-4% of pediatric brain tumors, and 10-20% of brain tumors in children younger than 1 year of age [2,3]. Choroid plexus papilloma usually present with signs of raised intracranial pressure like headache, nausea, vomiting, drowsiness, ocular and gaze palsies, papilledema and blindness [4-6]. In rare circumstances patients present with seizure and psychosis [7-9]. On the contrary our case presented with sub-acute onset and rapidly progressive of dementia and gait ataxia which is an unique and rare presentation. This history, findings and the age of the patient held us in a diagnostic quandary. However the radiologic findings were conclusive and the diagnosis was established.
Tumors that arise in the lateral ventricle are much more common in patients 10 years of age or less, whereas those that arise in the fourth ventricle are fairly evenly distributed among patients 0-50 years of age [3]. In a study conducted by Taconni et al the main symptom of choroid plexus papilloma in adults was papilledema, which accounted for 63% and unsteady gait in children, which accounted for 71% [10]. On the contrary a study conducted by Ta Hsieh C et al. concluded that choroid plexus papilloma in the lateral ventricle presents with long history of headache, paresis, and cranial nerve palsies, and progressive visual loss is typical in adults [6]. Choroid plexus papillomas in the fourth ventricle or cerebellopontine angle, signs and symptoms of hydrocephalus accompanied by ataxia, lower cranial nerve palsies, and visual disturbances are the most common presentations in all age groups [6,11]. In our case there was neither cranial nerve involvement nor visual disturbances, however there was limited involvement of the pyramidal tract and dementia which is not very frequently accounted before.
The pathophysiology has been attributed to an obstruction to CSF flow by the tumor or the higher production (four to five times) of CSF by the stimulated tumor cells [6,11,12]. It is well documented that choroid plexus tumors may produce CSF in amounts far exceeding the average of 450 mL per day that is normally observed [12,13]. In neuroimaging studies, a choroid plexus papilloma usually presents as a well-margined, smooth or lobulated, calcified, iso-dense or hyper-dense mass on pre-contrast computed tomography (CT) and shows dense and usually homogeneous enhancement on post-contrast CT [6,12]. Choroid plexus tumors are soft well-circumscribed cauliflower-like masses with prominent lobulations peripherally. Hemorrhage and cyst formation may be seen. Necrosis and parenchymal invasion are characteristic features for choroid plexus carcinoma [14,15]. Those tumors that have a pedicular attachment may move within the ventricle, giving rise to acute gravity-dependent intermittent ventricular obstruction, and have been associated with the bobble-head doll syndrome in some cases [15,16].
This case highlights a very rare benign intracranial neoplasm in an adult with a unique presentation of rapidly progressive dementia. This reiterates the role of neuroimaging in cases of cognitive dysfunction even in elderly where it need not always be neurodegenerative disorder.
References:
- Christian H. Rickert, Werner Paulus. Tumors of the choroid plexus. Microsc Res Tech. 2001;52(1):104-111.
- Strojan P, Popovic M, Surlan K, Jereb B. Choroid plexus tumors: a review of 28-year experience. Neoplasma. 2004;51(4):306-312.
- Aguzzi A, Brandner S, Paulus W. Choroid plexus tumours. In: Kleihues P, Cavenee W, eds. Pathology and genetics of tumours of the nervous system. Lyon, France: IARC, 2000; 84-86.
- Krishnan S, Brown PD, Scheithauer BW, Ebersold MJ, Hammack JE, Buckner JC. Choroid plexus papillomas: a single institutional experience. J Neurooncol. 2004;68:49-55.
- Agarwal A, Chopra S, Sehgal AD. Choroid plexus papilloma associated with developmental delay. Indian J Pediatr. 2004;71:763-766.
- Cheng-Ta Hsieh, Guann-Juh Chen, Wen-Chiuan Tsai, En-Yuan Lin, Chung- Ching Hsia. Choroid Plexus Papilloma in an Adult. J Med Sci 2008;28(2):95-98.
- Carson B, Weingart J, Guarnieri M, Fisher P. Third ventricular choroid plexus papilloma with psychosis: case report. J Neurosurg 1997;87:103-105.
- McGirr S, Ebersold M, Scheithauer B, Quast L, Shaw E. Choroid plexus papillomas: long-term follow-up results in a surgically treated series.?J Neurosurg 1988;69:843-849.
- Pollock I, Schor N, Martinez A, Towbin R. Bobble-head doll syndrome and drop attacks in a child with a cystic choroid plexus papilloma of the third ventricle. J Neurosurg 1995;83:729-732.
- Tacconi L, Delfini R, Cantore G. Choroid plexus papillomas: consideration of a surgical series of 33 cases. Acta Neurochir (Wien). 1996;138:802-810.
- Ironside JW, Moss TH, Louis DN, Lowe JS, Weller RO. Diagnostic pathology of nervous system tumours. London:Churchill Livingstone, 2002:168-173.
- McEvoy AW, Harding BN, Phipps KP, Ellison DW, Elsmore AJ, Thompson D, Harkness W, Hayward RD. Management of choroid plexus tumours in children: 20 years experience at a single neurosurgical centre. Pediatr Neurosurg. 2000;32:192-199.
- Koeller and Sandberg. Cerebral Intraventricular Neoplasms: Radiologic Pathologic Correlation.2002;22(6):1490-1497.
- Shin JH, Lee HK, Jeong AK, Park SH, Choi CG, Suh DC. Choroid plexus papilloma in the posterior cranial fossa: MR, CT, and angiographic findings. Clin Imaging. 2001;25:154-162.
- Pencalet P, Sainte-rose C, Lellouch-tubiana A, Kalifa C, Brunelle F, Sgouros S, et al. Papillomas and carcinomas of the choroid plexus in children. J Neurosurg 1998;88:521-528.
- Ellenbogen R, Winston K, Kupsky W. Tumors of the choroid plexus in children. Neurosurgery 1989;25:327–335.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
Shanmugam G V, Basheer A, SudhakarRapidly Progressive Dementia with Gait Ataxia.JCR 2014;4:209-212 |
|
Shanmugam G V, Basheer A, SudhakarRapidly Progressive Dementia with Gait Ataxia.JCR [serial online] 2014[cited 2026 Jan 3];4:209-212. Available from: http://www.casereports.in/articles/4/1/Rapidly-Progressive-Dementia-with-Gait-Ataxia.html |

|
|
|
|
|