|
|
|
|
|
Surgical Reconstruction of Non Malignant Superior Vena Cava Syndrome by PTFE Graft
|
|
|
generico cialis farmacia tadalafil generico doc click here
From the Department of General Surgery1; Department of Medicine, Nephrology Division2; Department of Vascular Surgery3; St Georges Hospital University Medical Center, Beirut, Lebanon. |
|
|
|
|
|
Corresponding Author:
|
Dr. Christian GERGES
Email: christiangergess@hotmail.com
|
|
|
|
|
|
|
|
|
Received:
07-FEB-2014 |
Accepted:
22-MAR-2014 |
Published Online:
15-APR-2014 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
Non-malignant superior vena cava syndrome due to indwelling catheters is rising in prevalence, reaching 1-3% of patients with central venous catheters. Surgical treatment is curative and long-standing. More than 5 million central venous catheters are now being implanted in the United States and are associated with upper extremity or central vein deep vein thrombosis in 7-30% of patients. Herein, we present a case of 18 year old male patient with history of end stage renal disease with recurrent use of indwelling catheters for haemodialysis admitted for surgical management of non-malignant superior vena cava occlusion by PTFE graft.
|
|
|
|
|
|
Keywords :
|
Superior Vena Cava Syndrome, Indwelling catheters, Kidney Failure, Thrombosis, Renal Dialysis.
|
|
|
|
|
|
|
|
|
|
|
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff74c105000000ba02000001000900 6go6ckt5b5idvals|307 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
The rapid increase in use of indwelling central venous catheters over the past two decades has resulted in greater number of patients with superior vena cava syndrome of benign etiology. More than 5 million central venous catheters are now being implanted in the United States and are associated with upper extremity or central vein deep vein thrombosis in 7-30% percent of patients [1,2]. Symptoms of venous congestion of the head and neck secondary to occlusion of the superior vena cava or innominate veins develop in about 15,000 patient each year in United States [3].
Superior vena cava syndrome is caused by malignant tumors of the lung and mediastinum in 60% of cases. The most frequent non-malignant cause of superior vena cava syndrome is intravenous catheters or pacemaker wires, where superior vena cava syndrome occurs in 1-3% of patients with central venous catheters. Surgical treatment for benign superior vena cava syndrome is usually curative and long lasting.
Herein, we report a case of 18 year old male patient known to have end stage renal disease on hemodialysis with history of recurrent use of indwelling catheter admitted for surgical management of nonmalignant superior vena cava syndrome induced by venous catheter for hemodialysis using a PTFE graft.
Case Report
An 18 year old male patient was admitted for surgical management of non-malignant superior vena cava syndrome induced by indwelling catheter for hemodialysis by PTFE graft after failure of endovascular intervention. History dates back to the age of 8 years, that is 10 years prior to the presentation, where the patient was diagnosed, by kidney biopsy, to have focal segmental glomerulosclerosis (FSGS) progressing to end stage kidney disease requiring dialysis. Consequently, arteriovenous fistula was created and central venous catheter for hemodialysis was inserted awaiting AV fistula maturation.
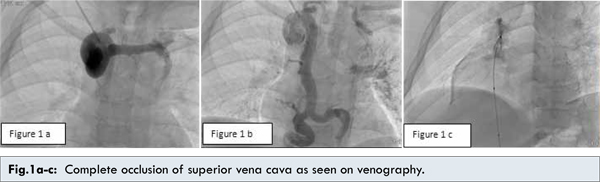
Over a period of seven years the patient suffered from recurrent AV fistula thrombosis requiring multiple thrombectomies and multiple insertions of central venous catheter for hemodialysis. Meanwhile the patient was investigated for hypercoagulable state which turned out to be negative. Over a period of 7 years, multiple catheters were required and the procedures were complicated by failure to proceed by catheter to the level of atriocaval junction. On the other hand, the patient started to complain of superior vena cava syndrome symptoms manifested by feeling of fullness in head and neck, orthopnea, head and neck swelling. Hence, the diagnosis was confirmed by CT scan of chest showing complete occlusion of the distal superior vena cava. This was followed by three years of progressive worsening in symptoms with failure of conservative measures in alleviating the patients symptoms. Consequently the patient was scheduled for endovascular intervention with an attempt to place a stent in the superior vena cava at level of obstruction, but the procedure failed due to inability to cross the occluded superior vena cava [Fig.1a-c].
After failure of conservative measures and after failure of endovascular intervention, surgical treatment was the only option left. A surgical reconstruction was performed from the superior vena cava to the level of right atrium using a 16 mm PTFE graft through a median sternotomy. [Fig.1d,e]
Discussion
Patients with superior vena cava syndrome can have severe incapacitating symptoms that cannot be relieved by conservative measures. Failure of conservative measures and endovascular intervention in managing and relieving the symptoms are indications for surgical reconstruction. Surgical treatment of superior vena cava syndrome can be performed using great saphenous vein graft, femoral vein graft, spiral saphenous vein graft and PTFE. Patients should be individualized when surgery is indicated.
Our choice was PTFE due to unavailability of large diameter autologous vein to be used as a conduit , and the poor size match of the great saphenous. Added to this was underlying thrombotic abnormality in our patient, manifested by recurrent AV fistula thrombosis, making the choice of femoral vein as a conduit not optimal. This is due to the underlying risk of edema, pain, compartment syndrome, and chronic venous insufficiency after removal of deep leg veins in patients with thrombotic abnormalities [4,5]. Besides, the excellent long term patency of short and large diameter PTFE grafts when used for large vein reconstruction made PTFE our best choice [6,7]. On the other hand, the already present AV fistula in the right arm will ensure long lasting patency of the graft [8].
The patient tolerated the reconstruction well, where complete relief from orthopnea was noted soon after surgery and 50% decrease in neck edema was seen next day.
Conclusion
Surgery for nonmalignant superior vena cava syndrome is usually curative and long lasting. Surgical reconstruction is indicated after failure of conservative measures and failure of endovascular intervention. Patients should be individualized while choosing the material of reconstruction.
References
- Rosamond W, Flegal K, Friday G, et al. Heart disease and stroke statistics-2007 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2007;115:e69.
- Korkeila P, Nyman K, Ylitalo A, Koistinen J, Karjalainen P, Lund J, et al. Venous obstruction after pacemaker implantation. Pacing Clin Electrophysiol. 2007;30:199.
- Wilson LD, Detterbeck FC, Yahalom J. Superior vena cava syndrome with malignant causes. N Engl J Med. 2007;356:1862.
- Wells JK, Hagino RT, Bargmann KM, et al. Venous morbidity after superficial femoral-popliteal vein harvest. J Vasc Surg. 1999; 29:282-289.
- Modrall JG, Hocking JA, Timaran CH, Rosero EB, Arko FR 3rd, Valentine RJ, et al. Late incidence of chronic venous insufficiency after deep vein harvest. J Vasc Surg. 2007; 46:520.
- Gloviczki P, Pairolero PC. Prosthetic replacement of large veins. In: Bergan J, Kistner RL, ed. Atlas of Venous Surgery, Philadelphia, PA: WB Saunders; 1992:191.
- Jost CJ, Gloviczki P, Cherry KJ, McKusick MA, Harmsen WS, Jenkins GD, et al. Surgical reconstruction of iliofemoral veins and the inferior vena cava for nonmalignant occlusive disease. J Vasc Surg. 2001;33:320.
- Magnan PE, Thomas P, Giudicelli R, Fuentes P, Branchereau A. Surgical reconstruction of the superior vena cava. Cardiovasc Surg. 1994; 2:598.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
SAIKALY E, ZEIDAN S, GERGES C, El FEGHALY MSurgical Reconstruction of Non Malignant Superior Vena Cava Syndrome by PTFE Graft.JCR 2014;4:120-122 |
|
SAIKALY E, ZEIDAN S, GERGES C, El FEGHALY MSurgical Reconstruction of Non Malignant Superior Vena Cava Syndrome by PTFE Graft.JCR [serial online] 2014[cited 2025 Sep 30];4:120-122. Available from: http://www.casereports.in/articles/4/1/Surgical-Reconstruction-of-Non-Malignant-Superior-Vena-Cava-Syndrome-by-PTFE-Graft.html |

|
|
|
|
|