|
|
|
|
|
A Fatal combination of HIV and Falciparum Malaria
|
|
|
Sivakumar Periyasamy, Nayyar Iqbal, Sanjoy George, Kevin John
From the Department of General Medicine, Pondicherry Institute of Medical Sciences, Puducherry-605014, India. |
|
|
|
|
|
Corresponding Author:
|
Dr. Nayyar Iqbal
Email: drinayyar@gmail.com
|
|
|
|
|
|
|
|
|
Received:
24-OCT-2014 |
Accepted:
05-DEC-2014 |
Published Online:
25-DEC-2014 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
Severe falciparum malaria is a medical emergency with high mortality rate. HIV co-infection not only adds to the severity of illness and mortality but also contributes to the decreased effectiveness of the treatment. We report 40 year old male of severe falciparum malaria with HIV co-infection, who presented with altered sensorium, severe intravascular hemolysis and acute renal failure with parasite index of more than 10%. Although, he was treated with artesunate, clindamycin and hemodialysis, he succumbed to his illness.
|
|
|
|
|
|
Keywords :
|
Falciparum malaria, HIV Infections, Acute Kidney Injury, Plasmodium falciparum, Parasites, Humans.
|
|
|
|
|
|
|
|
|
|
|
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff5c00060000006603000001000100 6go6ckt5b5idvals|405 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
Malaria, HIV along with the diarrhea, tuberculosis, measles, hepatitis B and pneumonia, accounts for 85% of global infectious disease burden. According to WHO 70% malaria cases that are found in South East Asia, reside in India. The estimated death due to malaria in India is around 205,000 per year [1]. There are nine vectors transmitting malaria in India out of which Anopheles culicifacies is widely distributed and principal vector of rural and peri-urban malarial infection. Among all the reported cases of malaria, Plasmodium falciparum has shown an increasing trend as an agent [2].
India has the third largest population of HIV/AIDS in the world. The annual report 2013-14 of National Aids Control Organization (NACO) estimates around 20.89 lakhs of people living with HIV/AIDS in India [3]. People living with HIV and AIDS (PLHA) has higher risk of developing severe falciparum malaria. Malaria parasite index is high in PLHA as compared to normal population. This could lead to increased malarial transmission affecting both HIV infected and non-infected individuals [4]. We report a case of severe falciparum malaria and HIV co-infection with severe hemolysis and multiorgan dysfunction (MODS).
Case Report
A 40 year old gentleman presented to emergency department of Pondicherry Institute of Medical Sciences with history of intermittent fever with chills and rigor for past 4 days, jaundice for past 2 days and passing of dark coloured urine for past 1 day. On examination patient was confused and disoriented, febrile with temperature 1030F and pulse of 120 per minute. His blood pressure was 110/64 mmHg and he was severely icteric with mild splenomegaly. There was no neck stiffness. Other systemic examination was found to be normal. There was no history of pain abdomen and vomiting. Patient was admitted in ICU in view of his clinical condition. He was catheterized which revealed black coloured urine [Fig.1].

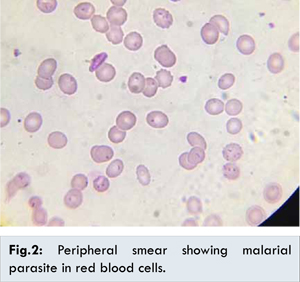
His complete blood count revealed severe anemia. His initial biochemistry analysis of blood sample could not be done as blood was getting hemolysed. His malarial antigen and peripheral smear was positive for Plasmodium falciparum with parasite index of 10.1 % [Fig.2]. Blood and urine cultures were negative. Leptospira antibody and scrub antibody was also negative. He was immediately started on injection artesunate (2.4 mg/kg/dose at 0, 12, 24 hours followed by once daily) and also injection clindamycin 600 mg twice daily. He was transfused with 1 unit of packed cell volume. After 2 dose of injection artesunate, serum biochemistry revealed deranged renal function and liver function [Table 1]. His urine for hemoglobin was positive. G6PD, Coomb’s test and ANA was found to be within normal limit.
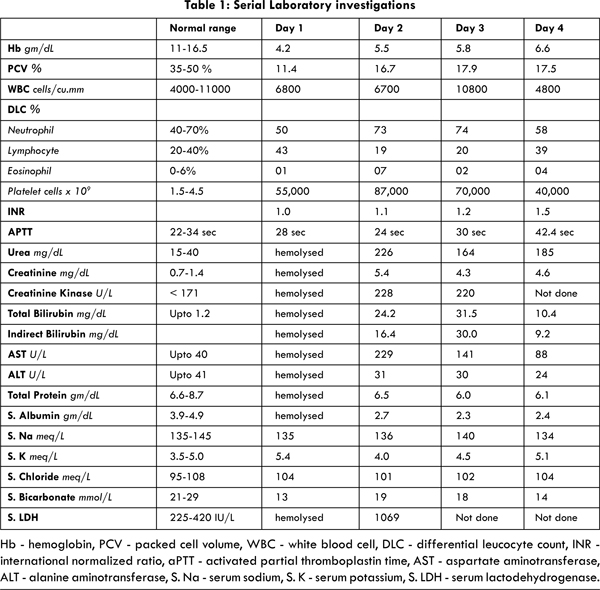
In view of haemoglobinuria secondary to hemolysis and severe metabolic acidosis on arterial blood gas analysis, he was started on hemodialysis. As a pre-hemodialysis work up, HbsAg, anti HCV antibody and HIV I &II were done. The result revealed that he was retroviral positive with negative titres for HbsAg, anti HCV antibody. Subsequently, his CD 4 count was found to be very low (CD4+: 41). On retrospectively taking history, we got history of promiscuity from his wife. He was started on tablet cotrimaxazole as prophylaxis for opportunistic infection. On 2nd day of admission patient became tachypneic and his oxygen saturation dropped below 90% so he was intubated and put on ventilator. His chest X-ray showed bilateral infiltrates, suggestive of acute respiratory distress syndrome. His blood pressure also dropped, hence inotropes were initiated. He was empirically started on injection piperacillin-tazobactum. Although, his parasite index was decreasing with injection artesunate his condition did not improve. On 4th day of admission his condition further deteriorated and inspite of all supportive treatment he succumbed to his illness. Patients relative did not gave consent for autopsy.
Discussion
Plasmodium falciparum is a protozoan disease transmitted by the bite of Anopheles mosquito. Among the five causes of malaria, falciparum has more severe form of presentation [5]. Severe falciparum malaria is defined by the following criteria [6] - cerebral malaria, severe anemia, respiratory distress, renal failure, hypoglycemia, circulatory collapse, coagulation failure, impaired consciousness of any degree, jaundice, intractable vomiting and parasitemia > 2%. According to World Health Organization (WHO) severe disease is defined by presence of one or more of the following - impaired renal function, recurrent fits, unarousable coma (Glasgow coma scale < 11), anaemia (haemoglobin < 5 gm/dL), acute confusion or drowsiness, pulmonary edema, hypoglycaemia, metabolic acidosis. The case fatality by this stage of the disease is 10 - 20% [7]. Mohapatra BN et al. proposed a new scoring system for predicting outcome in severe falciparum malaria [8]. According to this scoring system our patient had a score of 6, which predicted a poor outcome.
The pathogenesis of severity of falciparum is due to its predilection to invade younger red blood cells and can also infect red blood cell of all ages. This contributes to the increased severity of the disease by causing high parasite load. Once parasite enters the human body it invades the liver and replicate there before entering the blood circulation and then invading the erythrocytes. CD4+ and CD 8+ T cells kills the intrahepatic parasites [9]. In retroviral positive patient, there could be aberrant host response triggered by malaria, which can lead to the severe illness [10]. HIV infection decreases opsonizing antibodies to variant surface antigens of Plasmodium falciparum and antibodies to merozoite antigen, which may contribute to high parasite load [11]. Study from Uganda has showed that malaria speed up the progression of HIV disease and there is a rapid decline of CD4 cells inspite of the treatment [12].
Severe hemolysis is one of the features of complicated falciparum malaria. It may be due to either by rupture of infected red blood cell or phagocytosis of uninfected cell due to antibody sensitization or splenic sequestration. There can also be decreased erythropoiesis, as seen in acute infection [13]. In endemic area the cause for anemia could be secondary to iron, folate and Vit. B12 deficiency or due to effects of the antimalarial drugs through immune and non immune mechanism [14]. These work up was not done in our patient. Vishnu Sharma et al. has reported three cases of autoimmune hemolytic anemia in case of falciparum malaria [15]. All the three cases had drop in their hemoglobin level even after the treatment of malaria and they all responded to steroid. In our patient Coomb’s test and ANA both were negative.
Although, our patient had not taken quinine as a treatment for his fever, he presented with black coloured urine. Black water fever is seen in residents of malaria endemic region who take quinine irregularly. Another cause for black water fever is G6PD deficiency. In our patient, G6PD was found to be normal. Black water fever is characterized by severe intravascular hemolysis. This can be associated with abdominal pain, jaundice, hepatosplenomegaly and renal failure [16].
Acute renal failure is one of the presentations of severe falciparum malaria. The underlying cause could be dehydration, intravascular hemolysis, hyperparasitemia, cholestatic jaundice and hypotension [17]. Prakash J et al. reported acute renal failure in 26 patients of falciparum malaria [17]. Out of which 8 had intravascular hemolysis and 15 required hemodialysis. In his study mortality was seen in 30.8% of cases.
The recommended treatment for severe falciparum malaria is injection artesunate with tablet doxycycline or clindamycin [7]. L Zamidei et al. has reported a case of severe falciparum malaria, which was successfully treated with the combination of artesunate and quinine [6]. In our case due to severe intravascular hemolysis quinine was not initiated, although injection artesunate was immediately administered along with clindamycin. Parasite index with the above treatment improved but later he developed MODS and succumbed to his illness.
Conclusion
Severe falciparum malaria at presentation with very high parasite index should always prompt the clinician to rule out HIV co-infection. Inspite of advances in detection and treatment of malaria, coinfection with HIV has high mortality.
References
- Dhingra N, Jha P, Sharma VP, Cohen AA, Jotkar RM, Rodriguez PS, et al. Million Death Study Collaborators: Adult and child mortality in India: a national representative mortality survey. Lancet. 2010;376:1768-1774.
- Dash AP, Valecha N, Anvikar AR, Kumar A. Malaria in India: Challenges and opportunities. J Biosci. 2008;33:583-592.
- Department of AIDS control of India. Annual Report 2013-14. New Delhi, India. Ministry of health and family welfare, 2014.
- Shankarkumar U, Shankarkumar A, Ghosh K. HIV and malaria co-infection in Mumbai, western India. J Vector Borne Dis. 2011;48;155-158.
- Muddaiah M, Prakash PS. A study of clinical profile of malaria in a tertiary referral centre in South Canara. J Vect Borne Dis. 2006;43:29-33.
- Zamidei L, Durval A, Bettocchi DM, Luzzio G, Bartoloni A, Consales G. Efficacy and safety of quinine-artesunate in an HIV-positive patient with severe falciparum malaria. Minerva Anestesiologica. 2010;76(1):66-69.
- World Health Organization. Guidelines for the treatment of malaria -2nd edition. 2010.
- Mohapatra BN, Jangid SK, Mohanty R. GCRBS Score: A new scoring system for predicting out come in severe falciparum malaria. Journal of the Association of Physicians of India. 2014;62:14-17.
- White NJ, Breman JG. Malaria. In: Longo D L (ed). Harrison’s Principles of Internal Medicine. 18th ed. McGraw Hill Medical. New Delhi. 2012. pp. 1688-1705.
- Grimwade K, French N, Mbatha DD, Zungu DD, Dedicoat M, Gilks CF. HIV infection as a cofactor for severe falciparum malaria in adults living in a region of unstable malaria transmission in South Africa. AIDS. 2004;18:547-554.
- Hasang W, Dembo EG, Wijesinghe R, Molyneux ME, Kublin JG, Rogerson S. HIV-1 Infection and Antibodies to Plasmodium falciparum in Adults. J Infect Dis. 2014:210(9):1407-1414.
- Tkachuk AN, Moormann AM, Poore JA, Rochtford RA,Chensue SW, Mwapasa V, et al. Malaria enhances expression of CC chemokine receptor 5 on placental macrophages. J Infect Dis. 2001;183:967-972.
- Phillips RE, Pasvol G. Anaemia of Plasmodium falciparum malaria. Baillieres Clin Haematol. 1992;5(2):315-330.
- Ghosh K, Ghosh K. Pathogenesis of anemia in malaria: a concise review. Parasit Res. 2007;101:1463-1469.
- Sharma V, Samant R, Hegde A, Bhaja K. Autoimmune Hemolysis in Malaria: A Report of Three Cases. J Assoc Physician of India. 2012;60:129-130.
- Gobbi F, Audagnotto S, Trentini L, Kurunziza I, Manuel Corachan M, Perri GD. Blackwater Fever in Children, Burundi. Emerging Infectious Diseases. 2005;11(7):1118-1120.
- Prakash J, Gupta A, Kumar O, Rout SB, Malhotra V, Srivastava PK. Acute renal failure in falciparum malaria-increasing prevalence in some areas of India a need for awareness. Nephrol Dial Transplant. 1996;11(12):2414-2416.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
Periyasamy S, Iqbal N, George S, John KA Fatal combination of HIV and Falciparum Malaria.JCR 2014;4:500-504 |
|
Periyasamy S, Iqbal N, George S, John KA Fatal combination of HIV and Falciparum Malaria.JCR [serial online] 2014[cited 2025 Apr 26];4:500-504. Available from: http://www.casereports.in/articles/4/2/A-Fatal-combination-of-HIV-and-Falciparum-Malaria.html |

|
|
|
|
|