|
|
|
|
|
Acanthamoeba Keratitis in a Non-contact Lens Wearer: A Challenge in Diagnosis and Management
|
|
|
Dian Eka Putri, Lukman Edwar, Made Susiyanti
Department of Ophthalmology, Medical Faculty Universitas Indonesia, Indonesia. |
|
|
|
|
|
Corresponding Author:
|
Dr. Dian Eka Putri
Email: ekaputri_dian@yahoo.com
|
|
|
|
|
|
|
|
|
Received:
24-JUL-2014 |
Accepted:
13-SEP-2014 |
Published Online:
30-OCT-2014 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
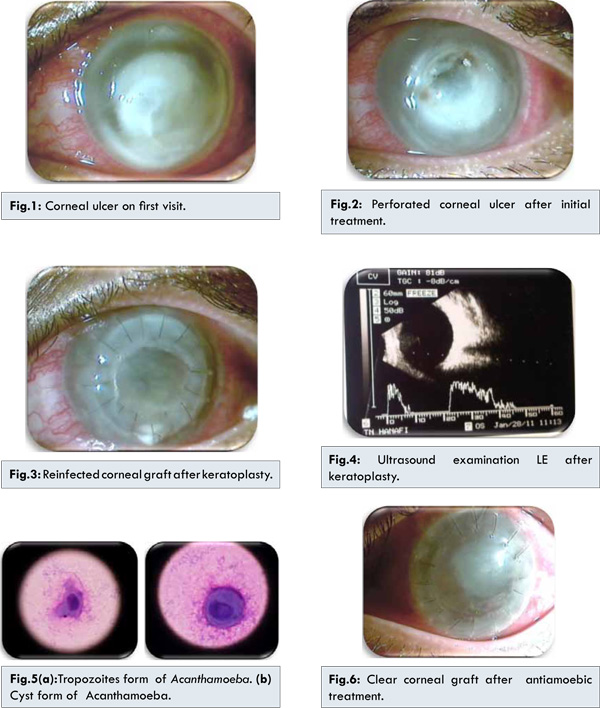
Purpose: To report a rare and challenging case of Acanthamoeba keratitis (AK) in non-contact lens wearer that required multiple therapeutic keratoplasty and succesfully treated with topical anti-parasitic drops. Methods: A twenty-two years old Indonesian man with no history of wearing contact lens came to the hospital with chief complain of whitish spot and foreign body sensation in his left eye. He washed his eyes with tap water and few days afterwards began to develop redness and severe blurred vision. The visual acuity (VA) was hand movement (HM) with wrong projection, there was corneal ulceration and infiltrate of 8 mm diameter. Therapeutic penetrating keratoplasty (PK) was performed due to nonresponsive corneal infiltrate and development of hypopyon. No sign of endophthalmitis was noted on the posterior part of the eye. Parasitic laboratory culture on non-nutrient agar with E. coli overlay from reinfected corneal graft specimen revealed Acanthamoeba in trophozoites and cysts forms. Patient improved with anti-parasitic propamidine 0.1% eyedrops. Conclusion: Acanthamoeba keratitis should be suspected in cases which fail to respond to antibiotic and/or antifungal medical therapies. |
|
|
|
|
|
Keywords :
|
Acanthamoeba Keratitis, Acanthamoeba, Keratoplasty, Contact Lenses, Cornea, Endophthalmitis, Humans.
|
|
|
|
|
|
|
|
|
|
|
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff0800060000003f03000001000700 6go6ckt5b5idvals|384 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
Acanthamoeba keratitis is a rare and one of the challenging cases of corneal infection. History of contact lens use is the most common etiology. Acanthamoeba keratitis in non-contact lens wearer is often associated with trauma and exposure to contaminated water or soil, tank-fed water in home, warmer heater, or poor socioeconomic conditions. Clinical presentation of AK is unilateral redness and severe pain in the eye. Non specific epitheliopathy in cornea may progress to ulceration with corneal infiltration. Other typical but uncommon finding is radial keratoneuritis or perineuritis and in late phase showed stromal ring infiltrates [1-3]. In United States, an estimated 85% of cases were contact lens wearer, with incidence in developed countries being 1 of 33 cases per million contact lens wearers [4]. Difficulties in diagnosis of AK may due to clinical appearance mimicing other corneal diseases such as herpes simplex keratitis, reccurrent corneal erosion, and diffuse epitheliopathies [3]. Corneal scraping smears or stromal biopsies are required to be examined for specimen culture on non-nutrient agar with overlay Escherichia coli or Enterobacter [1]. The management of AK is difficult due to the ability to encyst in the corneal tissue (cyst form) despite the use of aggressive topical therapy [1]. In severe or refractory cases, surgical keratoplasty is required. Medical treatment of AK includes anti-parasitic topical eye-drops like propamidine 0.1%, neomycin 1%, and cationic antispeptic such as chlorhexidine 0.02% and polyhexamethylene biguanide (PHMB 0.02%) [4]. This case d emonstrates a challenge in making the diagnosis and management of AK in non-contact lens wearer.
Case Report
A twenty-two year old male presented to the hospital with chief complaint of whitish spot in his left eye (LE) since last two months. In earlier symptoms, he felt foreign body sensation in his LE while he was riding motorcycle. Thereafter, he felt blurred vision and redness of the LE. He had history of rubbing and washing his eye with tap-water at his home. He went to the clinic and was prescribed oral and eyedrop antibiotics, natamycin eyedrops and oral mefenamic acid.
Ophthalmology examination revealed visual acuity of hand movement in LE with doubtful projection, edema and spasm of the eyelid, conjunctiva and ciliary injection, defect of cornea with infiltrate 8 mm diameter, while other parts were hard to be evaluated [Fig.1]. Direct microbiology examinations and cultures from corneal scrapings failed to reveal bacterial or fungal infection. Patient was diagnosed as keratitis of the LE secondary to mixed bacterial and fungal infection. His LE was treated with natamycin and levofloxacin eyedrops hourly, timolol 0.5% twice a day, chloramphenicol eye ointment three times, oral capsule levofloxacin 1x500 mg and mefenamic acid tablets 3x500 mg. Three days after treatment, hypopyon was noted at anterior chamber. Then patient was treated with intracameral amphotericin B injection and irrigation aspiration of hypopyon. Amphotericin B eyedrops were added hourly. Two days after last treament, corneal perforation occurred [Fig.2]. Penetrating keratoplasty (PK) was performed on the next day while continuing with all medical therapies. Visual acuity after PK improved to hand movement with good projection, corneal graft was relatively clear with coagulum and bubble in deep anterior chamber, iridectomy at 1 o’clock, clear lens and positive fundus reflex. One week after PK, there were epithelial defect with infitrate 6x7 mm noted at inferior graft and 1 mm hypopyon. Treatment of levofloxacin was changed to dibekacin fortified eyedrops hourly. One week after, the visual acuity decreased to light preception (LP) and there was a loose suture at six o’clock, corneal graft was largely edematous and inferior bulging with prolapse of coagulum [Fig.3]. Ultrasound examination revealed thickened choroid, however posterior segment was clear [Fig.4]. No signs of improvement were noted and the corneal graft was re-infected. Repeat PK was performed and the previous corneal graft was examined for parasitic culture. The culture result revealed trophozoites and cyst forms of Acanthamoeba [Fig.5a,b]. Previous treatment were stopped and changed to topical eyedrop propamidine 0.1% 2 hourly, lubricant protagent A® 3 hourly and polygran® antibiotic ointment at night. One month after repeated PK, the visual acuity improved to hand movement with good projection, no sign of infection was seen, and corneal graft was clear, however complicated cataract was noted due to chronic inflammation [Fig.6]. Cataract removal was planned to improve his vision.
Corneal trauma becomes one of the main risk factor of corneal infection. Any event that disrupts the corneal epithelium is a potential risk factor for keratitis including AK [1]. The patient had history of corneal trauma followed by washing his eyes with tap water, this may have caused defect on the corneal epithelial surface. Tap water may be a source of Acanthamoeba infection. Other than the rarity of the case, misdiagnosis of AK on early presentation because of clinical characteristic symptom of painful eye was not seen in this patient. Xuguang et al. reported there were only 11 patients of AK who had severe ocular pain in total of 20 cases. Absence of ocular pain in patients of AK has also been reported in other studies [5]. The absence of ocular pain may be related to the absence of keratoneuritis which is characterized by linear radial, branching infiltration by the parasites along corneal nerves in the anterior stroma. It begins in paracentral and extends to limbus in radial pattern and stimulated sense of pain in AK [6]. Penetrating keratoplasty is usually performed to manage a corneal perforation or eliminate active infection in cornea when medical treatment is unable to halt the progression of the disease [7,8]. In this patient, the first penetrating keratoplasty was performed due to severe corneal infection which failed to respond to maximum antibiotics and antifungal treatments. However, the corneal graft was reinfected. This could be due to residual organism in the infected host cornea and reinfection of corneal graft, for which proper anti-parasitic medications were not prescribed. Recurrence of infection AK after PK had been reported 40-50% in several cases [5,9]. Repeated keratoplasty should be performed to prevent further infection to intraocular compartments. Penetrating keratoplasty is mostly required in moderate to severe cases of AK and in some cases requires repeated surgeries due to recurrence of infection or chronic complication [1,4]. Suspection of Acanthamoeba as the cause of infection was taken after 4 weeks of treatment without any sign of improvement. The culture result strongly helped to confirm the diagnosis. Savitri et al. reported, 38.5% patients of AK were delayed in diagnosis and initiation of treatment required more than 30 days [10]. Tight clinical observation and maintenance doses of medication may help to prevent the recurrence of Acanthamoeba infection.
Conclusion
Diagnosis and management of Acanthamoeba keratitis is rare and challenging. In non-contact lens wearer, it should be suspected if corneal infection significantly fails to respond with conventional antimicrobial therapy. Parasitic laboratory examination is needed to confirm the diagnosis.
Acknowledgment
The authors would like to give appreciation to Parasitology Department, Universitas Indonesia which had confirmed and made the laboratory diagnosis of this case.
References
- Sowka J, Gurwood A, Kabat A. Acanthamoeba keratitis. Handbook of ocular disease management [cited 2011 February 25]; Available from: http://cms.revoptom.com/handbook/oct02_sec3_2.html. Accessed on 13 September 2014.
- Tomita M, Shimura S, Tsubota K, Shimazaki J. Dacryoadenitis association with Acanthamoeba keratitis. Arch Ophthalmol. 2006;124:1239-1242.
- Dart J, Saw V, Kilvington S. Perspective Acanthamoeba keratitis: diagnosis and treatment update. Am J Ophthalmol. 2009;148:487-499.
- Centers fot Disease Control and Prevention. The live cycle Acanthamoeba. Last review [cited 2011 February 25]; Available from: http://www.cdc.gov/parasites/acanthamoeba/biology.html. Accessed on 13 September 2014.
- Sun X, Zhang Y, Li R, Wang Z, Luo S, Gao M, et al. Acanthamoeba keratitis clinical characteristics and management. Am J Ophthalmol. 2006;113:412-416.
- Sharma N, Vajpayee B. Corneal ulcers diagnosis and management. New Delhi: Jaypee brothers; 2008.
- Kitzmann A, Goins K, John E. Sutphin, Michael D. Keratoplasty for treatment of Acanthamoeba keratitis.Am J Ophthalmol. 2009;116:864-869.
- Chynn E, Lopez M, Pavan L, Talamo J. Acanthamoeba keratitis contact lens and non contact lens characteristics. Ophthalmology. 1995;102(9):1369-1373.
- Joslin C, Yu E, Shoff M, Booton G, Fuerst P, Mcmahon T. The association of contact lens solution use and Acanthamoeba keratitis. Am J Ophthalmol. 2007;144:169-180.
- Sharma S, Garg P, Rao G. Patient characteristics, diagnosis, and treatment of non-contact lens related Acanthamoeba keratitis. Br J Ophthalmol. 2000;84:1103-1108.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
Putri DK, Edwar L, Susiyanti MAcanthamoeba Keratitis in a Non-contact Lens Wearer: A Challenge in Diagnosis and Management.JCR 2014;4:419-423 |
|
Putri DK, Edwar L, Susiyanti MAcanthamoeba Keratitis in a Non-contact Lens Wearer: A Challenge in Diagnosis and Management.JCR [serial online] 2014[cited 2025 Apr 26];4:419-423. Available from: http://www.casereports.in/articles/4/2/Acanthamoeba-Keratitis-in-a-Non-contact-Lens-Wearer.html |

|
|
|
|
|