Introduction
Acute endophthalmitis typically develops 2-5 days postoperatively and rarely caused by fungal infection [1,2]. It is associated with ocular pain in 74-85% cases and reduced vision in more than 90% cases [3]. There were only few reports about fungal wound infection related to endophthalmitis [4]. Outbreaks of fungal endophthalmitis may be derived from contaminated instruments, airborne contaminants, and ventilator systems [5,6]. This study reports 2 patients with fungal infection in clear corneal incision wound, leading to acute endophthalmitis post phacoemulsification in charity cataract surgery setting. This study emphasizes on clinical appearance and possible predisposing factors. The need for pars plana vitrectomy as a gold standard in cases of endophthalmitis is very challenging in case of endophthalmitis with keratitis/corneal ulcer. It is very important to detect and know the diagnosis earlier, thus appropriate treatment and management could be performed earlier in order to eradicate the infection, maintain the eye ball integrity and prevent severe visual loss.
Case Reports
Case 1
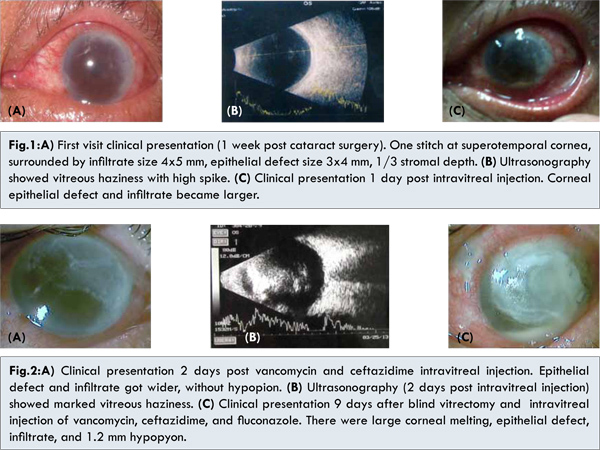
A 55 years old man presented with chief complaints of blurred vision, redness, pain on his left eye (LE) since 4 days after cataract surgery. One week before, he underwent uneventful phacoemulsification in charity cataract surgery. He denied washing his eyes with tap water or betel leaf water. He only used his medications which were levofloxacin eyedrop and antibiotic plus steroid eyedrops. At first presentation, his visual acuity was 6/30 before correction and 6/21 with pinhole. There was a stitch at supero-temporal cornea with burried knot, surrounded by infiltrate of size 4x5 mm, epithelial defect size 3x4 mm, 1/3 stromal depth [Fig.1a]. Anterior chamber indicated cells (+4), flare with fibrin and 1 mm hypopyon. Pupil was round, central, with positive light reflex. Intraocular lens was placed centrally. Vitreous was hazy and fundus was hard to be evaluated. The right eye (RE) was pseudophakic and visual acuity was 6/7.5 before correction and 6/6 with pinhole. The other parts were within normal limit.
Corneal scrapping with Gram staining demonstrated gram negative rod bacteria, while KOH examination found no hyphae. Ultrasonography of the LE revealed vitreous haziness [Fig.1b]. Patient was diagnosed with endophthalmitis post phacoemulsification of LE, corneal ulcer due to bacteria (differential diagnosis with fungal) of LE. He underwent vancomycin and ceftazidime intravitreal injection. Vitreous tap revealed relatively clear vitreous. He was hospitalized and received levofloxacin 1x500 mg intravenously, vancomycin eyedrops hourly, ceftazidime eyedrops hourly, levofloxacin eyedrops hourly.
On the next day, his visual acuity was hand movement with high intraocular pressure per palpation. Corneal epithelial defect and infiltrates became larger. Hypopyon was diminished into 0.5 mm [Fig.1c]. Two days after vancomycin and ceftazidime intravitreal injection, visual acuity was still restricted to hand movement. The epithelial defect and infiltrate got wider but no hypopyon was found [Fig.2a]. The corneal scrapping found hyphae but no bacteria. Ultrasonography of LE showed marked vitreous haziness [Fig.2b].
Patient underwent blind vitrectomy and injection of fluconazole, vancomycin, ceftazidime. Unfortunately the vitrectomy was unsuccessful and gram positive hyphae and coccus were detected in Gram’s staining. Therapies were continued with addition of fluconazole eyedrops hourly, natamycin eyedrops hourly, and itraconazole. Therapeutic keratoplasty was planned after inflammation subsided. Patient was referred to internal medicine department to look for any associated risk factors. He was diagnosed with type II diabetes mellitus, dyslipidemia and prescribed subcutaneous novorapid 3x8 IU.
Nine days following blind vitrectomy and intravitreal injection of vancomycin, ceftazidime, and fluconazole, visual acuity was still hand movement. There were large corneal melting, epithelial defect and infiltrates. Anterior chamber was deep with 1.2 mm hypopyon [Fig.2c]. However, reverse relative afferent pupillary defect (RAPD) showed negative result. Corneal culture demonstrated Aspergillus flavus. He underwent therapeutic keratoplasty, used non-optical corneal donor. During the operation, anterior chamber was irrigated by voriconazole. Intraocular lens was removed and intracameral voriconazole was injected at the end of surgery. Therapy post-surgery were itraconazole 1x200 mg, ciprofloxacin 2x750 mg, antifungal eyedrop (natamycin, fluconazole, voriconazole), timol 0.5% eyedrop 2x.
One day post therapeutic keratoplasty, visual acuity was light perception with good projection. Corneal graft was hazy with 16 stitches with burried knot [Fig.3a]. Anterior chamber was deep while other parts were hard to be evaluated. Ultrasonography showed minimal vitreous haziness on anterior part [Fig.3b]. One week post keratoplasty, visual acuity became hand movement with good projection. Intraocular pressure was 5 mmHg. Anterior chamber was shallow at nasal and temporal, but deep on the other part [Fig.3c]. The other parts were hard to be evaluated. Therapies were continued with itraconazole 1x200 mg, ciprofloxacin 2x750 mg, antifungal eyedrops.
One month post-therapeutic keratoplasty, visual acuity was hand movement. Anterior chamber was deep, iris/pupil was irregular, lens was aphakic [Fig.3d]. Posterior segment was hard to be evaluated. Therapies were continued with addition of pilocarpine 2% eyedrop 3x, and the loose sutures were released. Unfortunately patient did not come again for control because he passed away. His family said that he was hospitalized due to diabetes mellitus’ complication.
Case 2
A 59 years old woman presented with similar complaints since 1 week after cataract surgery. She also underwent uneventful phacoemulsification on charity cataract surgery. She was operated at the same operating table with the first patient. She denied washing her eyes with tap water or betel leaf water. She merely used her medications, which were levofloxacin eyedrops and antibiotic plus steroid eyedrops. She had history of steroid consumption orally for 6 months.
One week post-operative her visual acuity was 6/30. There were 3 stitches on the temporal cornea with infiltrate surrounded it [Fig.4a]. There were cells (+4) and flare in the anterior chamber without hypopyon. Intraocular lens was in central position and covered by fibrin. Funduscopy examination showed vaguely round optic nerve head with distinct edge but other details were hard to be evaluated. Ultrasonography revealed vitreous haziness on the anterior part [Fig.4b]. She was diagnosed with suspicion of endophthalmitis of LE. She received levofloxacin eyedrops hourly, antibiotic plus steroid eyedrops 6x, ciprofloxacin 2x750 mg oral, chloramphenicol eye ointment 3x, with a plan for ultrasonography again in two days.
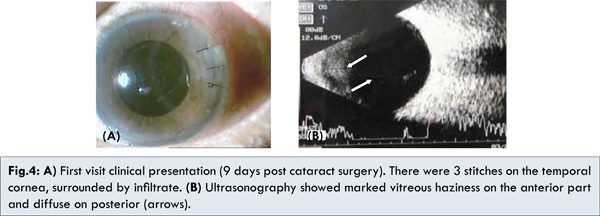
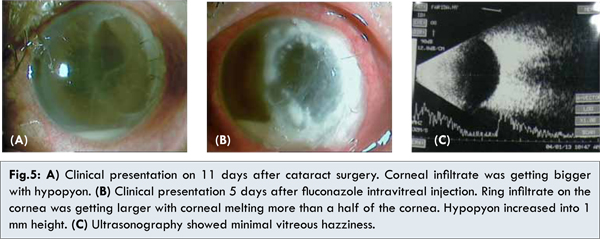
Two days later, her visual acuity decreased into half meter finger counting. The infiltrate was getting larger with size 6 mm diameter and hypopyon was 0.5 mm [Fig.5a]. Gram’s staining and KOH examination from corneal scrapping merely found hyphae. Patient was diagnosed with fungal post phacoemulsification endophthalmitis. Patient underwent vitreous tap and 100 mcg fluconazole intravitreal injection. Five days after intravitreal injection, ring infiltrate on the cornea was getting larger with corneal melting more than a half of the cornea. Hypopyon increased to 1 mm. [Fig.5b]. Ultrasonography showed minimal vitreous hazziness [Fig.5c]. Acanthamoeba laboratory examination was conducted, however it showed negative result. Vitreous culture showed Serratia marcescens on the isolate. However, culture result from corneal swab grew Aspergillus flavus which were sensitive to amphotericin B, itraconazole, ketoconazole, voriconazole, but resistant to fluconazole.
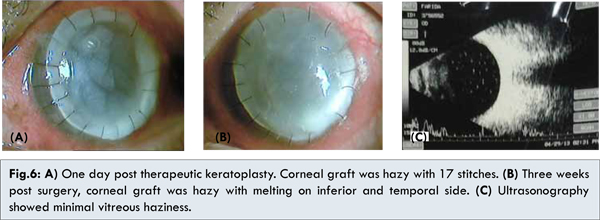
She underwent therapeutic keratoplasty of the LE. The infected cornea was discarded and examined for cultures (sabouraud and thioglikolat). During the surgery, anterior chamber was irrigated by voriconazole and intraocular lens was removed. Intracameral voriconazole was performed at the end of the surgery. Therapies post-surgery were itraconazole 1x200 mg, antifungal eyedrops, levofloxacin eyedrops 6x. One day post therapeutic keratoplasty, visual acuity was hand movement with good projection. Corneal graft was hazy with 17 stitches with burried knot [Fig.6a].
Three weeks post keratoplasty, she complained of pain on her left eye. She continued her medication, but sometimes skipped voriconazole eyedrops. She could not afford it due to the financial problem. Her visual acuity was decreased into light perception with wrong projection. Corneal graft was hazy with melting on inferior and temporal side. Anterior chamber was vaguely deep, and reverse RAPD was negative. The other parts were hard to be evaluated [Fig.6b]. Ultrasonography of LE was performed and showed minimal vitreous haziness without retinal detachment [Fig.6c]. Therapies were continued with oral itraconazole 1x200 mg, natamycin eyedrops, artificial tears, doxycycline 2x100 mg, medroxyprogesterone eyedrops 4x, EDTA eyedrops 4x, vitamin C 3x500 mg. She was planned for vitrectomy and repeat keratoplasty.
She underwent repeat keratoplasty, vitrectomy, voriconazole intravitreal injection of LE. Previous donor was retrieved, followed by open sky vitrectomy which showed vitreous haziness. Voriconazole was used to irrigate the vitreous cavity and clean up the fibrin, clot. The new cornea donor was stitched, continued with injection of intravitreal, intracameral voriconazole. Post-operative treatments were levofloxacin eyedrops, steroid eyedrops, voriconazole eyedrops. One day post-surgery, her visual acuity was hand movement. Corneal graft was clear with 16 stitches, burried knot. Anterior chamber was deep with minimal coagulum. Iris/pupil was irregular and the lens was aphakic [Fig.7a]. Posterior segments were hard to be evaluated. Therapies were still continued.
One week post-surgery, her visual acuity still hand movement with good projection. Corneal graft was clear with 16 stitches. The other anterior segments were relatively the same [Fig.7b]. She still continued her medications. One month post-surgery, her vision was getting better with objective 2 meters finger counting. Corneal graft was clear, with 16 stitches [Fig. 7c]. Two month post-surgery, her visual acuity increased into 3 meters finger counting. Corneal graft was clearing, with several loose stitches [Fig.7d]. Other anterior segments were show significant decrease of infection. Fundus reflex was positive. Therapies were replaced by antibiotic plus steroid eyedrops 4x, artificial tear eyedrops 6x.
Discussion
Acute endophthalmitis typically develops 2-5 days postoperatively and associated with ocular pain, reduced vision and redness [1,3]. Both patients complained of ocular pain, redness, and reduced vision since 4 days and 1 week after cataract surgery respectively. Signs of endophthalmitis include eyelid or periorbital edema, ciliary injection, anterior chamber reaction, corneal edema, and retinal hemorrhages, vitreous inflammation [7,8]. Both patients had corneal stitches, surrounded by infiltrate, anterior chamber reaction, vitreous haziness. Ultrasonography in endophthalmitis is routinely performed, showing strands/membranes, dense vitreous opacities, and posterior wall thickness [9,10]. Our patients subsequently showed vitreous haziness with high spike and milder haziness on the anterior part.
Aspirate of aqueous and/or vitreous for Gram stain and culture are commonly employed for diagnosis [11]. The highest rate of pathogen identification is obtained from vitreous using vitrectomy cutter [3]. First patient was given vitreous tap with syringe. The culture result did not reveal any growth of microorganism because the use of syringe may gave insufficient sample [3]. Negative result may be related to the primary location of the infection which starts in the front of the eye [12]. Vitreous culture from second patient showed Serratia marcescens. These results could be unreliable caused by specimen contamination [13].
Fungal organisms uncommonly cause postoperative endophthalmitis. Investigation on air particle at operating theatre showed normal limit of microorganism’s count. Both patients were operated on charity cataract surgery which used reusable instruments. Microbiological investigation from linen, instruments, wall, patient’s bed and floor were revealed no microbiological contamination.
Only few studies published data about wound infection related to endophthalmitis. Study from India investigated 31 cases of cataract wound infection and 174 cases of postoperative endophthalmitis. Fungi were isolated in 7 of these cases [4]. Intraoperative complications, temporal clear corneal incisions (CCI), and poor constructed wounds have significant relationship with higher incidence of endophthalmitis [7,14,15]. Both patients underwent uneventful phacoemulsification and had CCI on the temporal side sutured with nylon. They did not present with broken suture, but fungus still can penetrate through an incomplete epithelial barrier along the suture track and cause a stromal infiltrate [15,16]. It may also enter anterior chamber directly from contaminated instruments. However, we still could not establish the main mechanism.
Clinical presentation and onset may be helpful in predicting keratitis’ etiology. Fungal infection is insidious, insidious onset (5 to 10 days) and has dry ring infiltrate feature [16]. Corneal scrapping should directly inoculated into the culture media [16]. Gram staining is a helpful tool for initiating a rational antibiotic therapy while awaiting the results of definitive cultures [9]. Culture result from corneal swab of both patients showed Aspergillus flavus.
The use of topical/oral corticosteroid, immune/systemic conditions (diabetes, leukemia) can enhance fungal infection [3,17]. Corticosteroids used in the absence of an antifungal agent permits more aggressive fungal behavior [12]. Both patients got combination of antibiotic and steroid eyedrops post-surgery. It may be one of the risk factor for developing infectious corneal ulcer [17]. Moreover, first patient has diabetes mellitus while second patient had history of oral corticosteroid consumption. The gold standard treatment of acute post-operative endophthalmitis is immediate pars plana vitrectomy. However, it is often not possible so a silver standard may be applied with the antibiotic/antifungal intravitreal injection, preceded by vitreous biopsy [3].
First patient was underwent vancomycin, ceftazidime, fluconazole intravitreal injection and blind vitrectomy. However the blind vitrectomy was unsuccessful due to the opacity of the cornea. Second patient was instilled 100 µg fluconazole intravitreal injection. Fluconazole has broad antifungal activity but most active against Candida and Aspergillus. Intraocular injection of fluconazole (100 µg) is well tolerated and has been associated with resolution of exogenous fungal endophthalmitis [7].
Management of these cases was also hardly focusing on management of corneal ulcer which consists of medical therapy and surgical intervention. Clinical presentation of the first patient on two weeks of initial treatment showed no improvement. Despite combination of antifungal and antibiotic therapies, the corneal infiltrate was still progressing with corneal melting.
Therapeutic keratoplasty should be performed in cases of impending perforations, frank perforations >2 mm and/or if there is no response to maximum medical therapy [9]. Both patients were already receiving treatment with antifungal and antibiotic therapies for 2 weeks, however the infiltrate was getting larger with severe corneal melting and progression of hypopyon, hence they underwent therapeutic keratoplasty.
Topical antifungal agents should be continued after penetrating keratoplasty for 6-8 weeks to prevent recurrence of infection. Systemic ketoconazole or fluconazole should be used in addition to topical antifungal agents in case with deep tissue fungal keratitis [9,16]. Culture result from corneal swab of both patients showed Aspergillus flavus, hence voriconazole eyedrops was given for prolonged period. Topical administration of voriconazole demonstrated good penetration through the cornea into the aqueous humour, without compromising intraocular safety [18].
First patient applied voriconazole eyedrop for 1 month post keratoplasty. However, second patient used voriconazole eyedrops for about 3 weeks and then discontinued it and corneal graft became infected and then she underwent repeated keratoplasty. This shows the importance of using antifungal agent post-keratoplasty in prolonged period until significant heal and improvement of infection is achieved.
Conclusion
This study reports rare cases of acute endophthalmitis post phacoemulsification preceded by fungal corneal ulcer, related to clear corneal wound infection. Diabetes mellitus, steroid oral consumption could be the risk factor for developing fungal infection. Although these cases are rare, early diagnosis is important thus early treatment and management (e.g vitrectomy and/or keratoplasty) could be performed earlier in order to eradicate the infection and prevent more severe visual loss.
References
- Brod R, Flynn H. Endophthalmitis. In: David Schlossberg (ed). Clinical Infectious Disease. Cambridge University Press: NewYork; 2008. pp.109-116.
- Mendicute J. Keratomycosis after cataract surgery. J Cataract Refract Surg. 2000;26:1660-1666.
- Barry P, Baumann W, Pleyer U, Seal D. ESCRS Guidelines on prevention, investigation and management of post operative endophthalmitis. The European society for cataract and refractive surgeon, 1-37 (2007).
- Garg P, Mahesh S, Bansal A, Gopinathan U, Rao G. Fungal Infection of Sutureless Self-sealing Incision for Cataract Surgery. Ophthalmology. 2003;110:2173-2177.
- Kresloff M, Castellarin A, Zarbin M. Endophthalmitis. Surv Ophthalmol.1998;43:193-224.
- Kelkar A, Kelkar J, Amuaku W, Shaikh A. How to prevent endophthalmitis in cataract surgeries. Indian J Ophthalmol. 2008;56:403-407.
- Meredith T. In: Duane’s clinical ophthalmology (monograph on CD-ROM) Vol. 4 Lippincot Williams & Wilkins Pub, Inc, Philadelphia, 2007.
- Putri DK, Edwar L, Susiyanti M. Acanthamoeba Keratitis in a Non-contact Lens Wearer: A Challenge in Diagnosis and Management. Journal of Case Reports. 2014;4(2):419-423.
- Sharma N, Vajpayee B. Corneal ulcers diagnosis and management. New Delhi: Jaypee brothers; 2008.
- Maneschg O, Sakany B, Nemeth J. Ultrasonographic findings in endophthalmitis following cataract surgery: a review of 81 cases. Ophthalmology. 2009;106:1012-1015.
- Safneck. Endophthalmitis: a review of recent trends. Saudi Journal of Ophthalmology. 2012;26:181-189.
- Wykoff C, Flynn H, MIler D, Scott I, Alfonso E. Exogenous fungal endophthalmitis: microbiology and clinical outcomes. Ophthalmology. 2008;115:1501-1507.
- Endophthalmitis Vitrectomy Study Group: Results of the endophthalmitis vitrectomy study: a randomized trial of immediate vitrectomy and of intravenous antibiotics for the treatment of postoperative bacterial endophthalmitis. Arch Ophthalmol. 1995;113:1479-1496.
- Nagaki Y, Hayasaka S, Kadoi C. Bacterial endophthalmitis after small-incision cataract surgery: effect of incision placement and intraocular lens type. J Cataract Refract Surg. 2003;29:20.
- Maxwell D, Diamond J, May D. Surgical wound defects associated with endophthalmitis. Ophthalmic Surg. 1994;25:157-161.
- Thomas P. Fungal infections of the cornea. Eye. 2003;17(8):852-862.
- Cohen J, Freeman S, Page E. Treatment strategies for endophthalmitis. Review of Optometry, 2011.
- Al-Badriyeh D, Neoh C, Stewart K, Kong D. Clinical utility of voriconazole eye drops in ophthalmic fungal keratitis. Clinical Ophthalmology. 2010;4:391-405.