|
|
|
|
|
Hyperphosphatemic Tumoral Calcinosis
|
|
|
Umesh S Mudaliyar
From the Department of Radiology, Bhakti Vedanta Hospital, Thane, Mumbai - 401017, India. |
|
|
|
|
|
Corresponding Author:
|
Dr. Umesh S Mudaliyar
Email: umeshmudliyar@gmail.com
|
|
|
|
|
|
|
|
|
Received:
19-MAY-2014 |
Accepted:
30-AUG-2014 |
Published Online:
30-SEP-2014 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
Tumoral calcinosis is a rare ectopic extra-vascular calcification occurring around the joints. Deranged metabolic abnormality is the initial trigger for such calcification. We had a 28 year old female who had chronic swelling in both the hips for the past 24 months. On examination, bilateral, painless non-tender, firm lumps were observed in both the gluteal regions. X-ray of the local regions revealed bilateral large, lobulated, soft tissue masses that showed flocculent calcification which overlay the proximal third of femur. The patient was diagnosed to be a case of bilateral tumoral calcinosis and was managed successfully by excision and debulking surgery. We describe here this case of idiopathic calcinosis due to hyperphosphatemia considering its rare occurrence.
|
|
|
|
|
|
Keywords :
|
Hyperphosphatemia, Calcification, Calcinosis, Hip, Joints, Humans.
|
|
|
|
|
|
|
|
|
|
|
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff38f8050000001103000001000d00 6go6ckt5b5idvals|371 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
Tumoral calcinosis refers to the rare metabolic dysfunction of phosphate regulation resulting in massive periarticular calcinosis. Three types of calcinosis have been described in the literature. The first one (primary normophosphatemic tumoral calcinosis) being sporadic variety, in which there is no family history of a similar illness and the serum phosphate levels being in the normal range. The second type (secondary tumoral calcinosis) is associated with metabolic disturbances such as those with calcium or phosphate, the common causes being chronic renal failure, hypervitaminosis D, and primary hyperparathyroidism. The third variety (primary hyperphosphatemic tumoral calcinosis) is familial due to gene defect on the long arm of chromosome 2 leading to abnormal serum phosphate levels and increased 1, 25-dihydroxycholecalciferol levels [1]. In the last variety the defect may be present in any of the fibroblast growth factor, KL or GALTN3 gene [2]. There is no predilection to any of the genders. We described here a case of sporadic tumoral calcinosis attributed to hyperphosphatemia which is idiopathic in origin.
Case Report
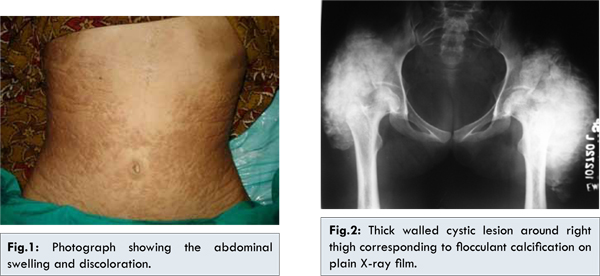
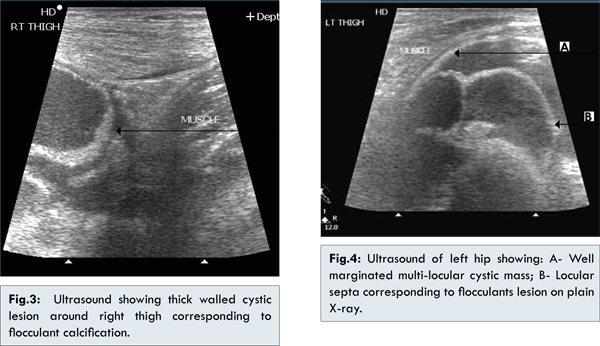
A 28 year old female presented with the complaints of progressive swelling in both the sides of the hip for the past 24 months. They were associated with reddish pigmentation without any pain. There was no history of trauma. On examination, bilateral, painless non-tender, firm lumps were observed in both the gluteal regions. There was an associated cutaneous pigmentation over the swellings [Fig.1] and the swellings were immobile. A mild restriction in abduction and external rotation of both the hip joints were noted. X-ray of the local regions revealed bilateral large, lobulated, soft tissue masses that show flocculent calcification which overlay the proximal third of femur [Fig.2]. Ultrasound examination showed bilateral multilocular cystic mass in hip and gluteal regions (20x16x27 cm right side and 28x17x26 cm left side) in the intermuscular planes & extending in to subcutaneous tissue [Fig.3,4]. There was no obvious demonstrable vascularity on colour doppler study. All the laboratory investigations were within normal limits except serum phosphate level [10.8 mg/dL; normal range – 2.6 to 4.5 mg/dL]. The parathyroid hormone was within normal limits and there was no history of consuming antacids or vitamin D preparations. The patient was diagnosed to be a case of bilateral tumoral calcinosis and was managed by excision and debulking surgery. Histopathological examination of the tissue revealed calcification with surrounding inflammatory giant cells and foreign body. Also medical management (aluminium hydroxide 2 TDS for 2 months followed by 1 TDS for 4 months) and dietary restriction of foods containing calcium were directed to correct serum phosphate level. The patient was given postoperative physiotherapy support and an improvement in the abduction & external rotation movements was observed. At the point of writing this manuscript, six months follow up was done and no local recurrence was seen.
We have presented here a case of young female presented with the complaints of chronic non-traumatic swelling in both the hips radiologically diagnosed as having tumoral calcinosis. Tumoral calcinosis is a rare pathological entity characterized by circumscribed, tumor-like, calcified masses in the connective tissues surrounding a joint [3]. These lesions mainly comprise calcium and phosphate crystals. The first description of the case is from Inclan et al. in 1943 [4], who described a familial condition characterized by normal serum calcium levels and elevated or normal serum phosphate levels. It typically occurs in the peri-articular regions such as around the hip, greater trochanter, behind the elbow, shoulder, chest wall, inferior angle of the scapula, sacrum, scalp and the bones of the hands and feet [5]. We have reported here a case of tumoral calcinosis of the hip. Apart from being idiopathic, several other causes have been attributed such as renal insufficiency, hyperparathyroidism, hypervitaminosis D and milk-alkali syndrome [6]. These disorders have an underlying abnormality of calcium and phosphorus homeostasis. Tumoral calcinosis is frequently misdiagnosed disorder. Steinbach et al. [7] reviewed the radiological and pathological reports of 12 patients with tumoral calcinosis, the largest collection till date, and found that a common radiological feature of these patients was a homogenous, dense calcified mass with “Chicken-wire” type lucencies representing the thin fibrous septae. Other differential diagnoses include calcific tendonitis, calcinosis universalis, calcinosis circumscripta, synovial osteochondromatosis, synovial sarcoma, myositis ossificans, tophaceous gout and calcific myonecrosis [8]. Estimation of serum mineral levels of calcium, phosphorus, tests of renal function, complete blood count, autoantibodies, hormonal assay, X-ray, bone scintigraphy, CT scan, MRI, FNAC, chemical analysis, microspectroscopic study of deposit and skin biopsy may help to achieve the specific diagnosis. In the present case, the serum levels of calcium and phosphate were normal and so was categorized as idiopathic. The pathway of calcinosis is initiated due to altered phosphate levels that start with the local hemorrhage progressing to fat necrosis, collagen formation and a massive calcification [9]. Surgery is the mainstay of management of tumoral calcinosis although recurrences have been noted if done incompletely. For patients with hyperphosphatemia, aluminium hydroxide is used as a first-line agent and others such as bisphosphonates, acetazolamide were found to be useful for those who don’t adequately respond to aluminium hydroxide [10,11]. Our patient was managed effectively by surgical correction and no recurrence was noted since 2 years following the intervention.
Considering the rarity of the occurrence of this type of pathologic calcification, tumoral sclerosis shall be considered as one of the differential diagnosis of patients with flocculent calcification at the bones and joints.
References
- Thomas N, Jacob JJ, Mathew K. Idiopathic sporadic tumoral calcinosis of the hip: successful oral bisphosphonate therapy. Endocrine Practice 2007;13:1-5.
- Lammoglia JJ, Mericq V. Familial tumoral calcinosis caused by a novel FGF23 mutation: Response to induction of tubular renal acidosis with acetazolamide and the non-calcium phosphate binder sevelamer. Horm Res 2009;71:178-184.
- Teutschlaender O. Ueber progressive Lipogranulomatoseder Muskulatur. Klin Wschr 1935;14:451-453.
- Inclan A, Leon P, Camejo MG. Tumoral calcinosis. JAMA 1943;121:490-495.
- Prasad VLN, Naresh KN, Krishna G, Ananthakrishnan N, Veliath AJ. Tumoral calcinosis. World J Surg 1989;13:803-808.
- Durant DM, Riley LH, Burger PC, McCathy EF. Tumoral calcinosis of the spine: a study of 21 cases. Spine. 2001;26:1673-1679.
- Steinbach LS, Johnston JO, Tepper EF, Honda GD, Martel W. Tumoral calcinosis: radiologic-pathologic correlation. Skeletal Radiology 1995;24:573-578.
- Hutt N, Baghla DP, Gulati V, Pastides PS, Beverly MC, Bashir WA. Acralpost-traumatic tumoral calcinosis in pregnancy: a case report. J Med Case Rep. 2011;5:89.
- Weiss SW, Goldblum JR. Soft Tissue Tumors. 4th edition. St Louis, MO: CV Mosby; 2001.
- Oslen KM, Chew FS. Tumoral calcinosis: pearls, poleomics and alternative possibilities. RadioGraphics 2006;26:871-885.
- Kirk TS, Simon MA. Tumoral calcinosis: report of a case with successful medical management. J Bone Joint Surg Am 1981;63:1167-1169.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
Mudaliyar USHyperphosphatemic Tumoral Calcinosis.JCR 2014;4:371-374 |
|
Mudaliyar USHyperphosphatemic Tumoral Calcinosis.JCR [serial online] 2014[cited 2026 Jan 9];4:371-374. Available from: http://www.casereports.in/articles/4/2/Hyperphosphatemic-Tumoral-Calcinosis.html |

|
|
|
|
|