|
|
|
|
|
Living Donor Liver Transplantation To Primary Sarcoma of the Liver
|
|
|
viagra cena bez receptu viagra
From the Departments of Gastroenterological Surgery1, Pathology2, Radiology3; Turkiye Yuksek Ihtisas Teaching and Research Hospital, Ankara, Turkey. |
|
|
|
|
|
Corresponding Author:
|
Dr. Volkan Öter
Email: otervolkan@gmail.com
|
|
|
|
|
|
|
|
|
Received:
20-JUL-2014 |
Accepted:
16-SEP-2014 |
Published Online:
20-OCT-2014 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
Primary sarcomas are rare tumors of the liver. Assessment of the diagnosis is difficult, particularly on percutaneous liver biopsy. Although liver transplantation (LT) can be indicated in selected cases of hepatic epithelioid hemangioendothelioma (HEHE) because of an excellent long term outcome, it is not advised for hepatic angiosarcoma (HAS) because of a high risk of early local or general recurrence rate after LT. We report the case of a young woman who underwent LT for a vascular hepatic tumor, of which some characteristics and the clinical presentation were suggestive of hepatic epithelioid hemangioendothelioma. However, the histological analysis of the explanted liver revealed hepatic angiosarcoma. We report an atypical clinical observation, which is especially interesting in that it illustrates the difficulty in distinguishing
the two forms of primary sarcoma of the liver. |
|
|
|
|
|
Keywords :
|
Liver Neoplasms, Bile Duct Neoplasms, Liver Transplantation, Hemangiosarcoma, Humans.
|
|
|
|
|
|
|
|
|
|
|
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1fff4ff05000000b802000001000e00 6go6ckt5b5idvals|379 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
Primary sarcomas of the liver are rare tumors and an exceptional indication for liver transplantation (LT) [1]. Assessment of the diagnosis is difficult, particularly on percutaneous liver biopsy. The two main histological forms are angiosarcoma (HAS) and hepatic epithelioid hemangioendothelioma (HEHE) [2]. Epithelioid hemangioendothelioma is a rare vascular tumour that was first described by Weiss and Enzinger in 1982 [3]. It has been described in many different organs such as the spleen, bone, brain, meninges, breast, heart, head and neck, soft tissue, stomach and lymph nodes [3,4]. HEHE has a 3:2 preponderance for females [5] and occurs most often in adults, with a peak incidence between 30 and 40 years of age [6]. HAS is a rare vascular tumor (<1/106 persons) and predominant in men (sex ratio, 4:1). The mean age is around 60 years [7]. Although LT can be indicated in selected cases of HEHE because of an excellent long term outcome [1,8], it is not advised for AS because of a high risk of early local or general recurrence rate after LT [7].
We report the case of a young woman who underwent LT for a infiltrative hepatic tumor, of which some characteristics and the clinical presentation were suggestive of HEHE. However, the histological analysis of the explanted liver revealed AS.
Case Report
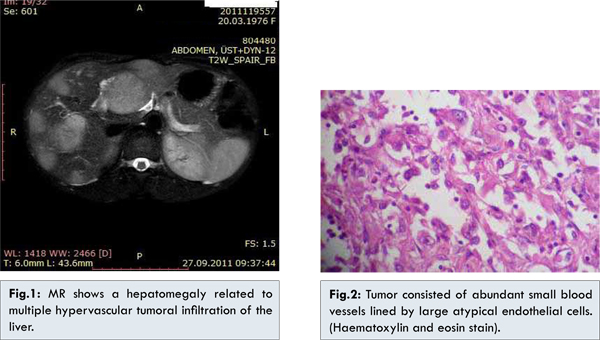
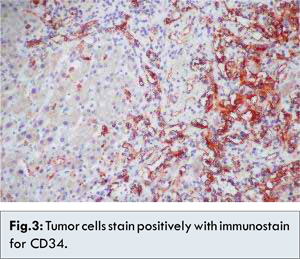
A 36 year old woman initially was referred to our hospital with multiple hepatic lesions. In physical examination; painless hepatomegaly was detected. Her blood pressure was 117/53 mmHg, heart rate 75 per min, respiratory rate 16 per min, and body temperature was 36.7oC. On physical examination, liver was hard and palpable by two finger breadth below the rib and abdomen was distended with ascites. Laboratory tests showed hemoglobin 11.6 g/dL, platelet count 93,000/mm3, white blood cell count 5,500/mm3, total protein 6.2 g/dL, albumin 3.8 g/dL, alanine aminotransferase 48 IU/L, aspartate aminotransferase 67 IU/L, total bilirubin 2.8 mg/dL, direct bilirubin 1.2 mg/dL, gamma-glutamyl transpeptidase 65 IU/L, alkaline phosphatase 79 IU/L, prothrombin time 35.5 seconds (1.23 INR), and activated partial thrombin time 33 seconds. Serologic markers for hepatitis A virus, hepatitis B virus and hepatitis C virus were negative. MRI detected a hepatomegaly related to multiple hypervascular tumoral infiltration of the liver [Fig.1]. The patient underwent liver biopsy. Microscopic examination showed cords, strands, and solid aggregates of round, oval, and polygonal cells, with abundant pale eosinophilic cytoplasm, vesicular nuclei, and inconspicuous nucleoli, embedded in a fibromyxoid or sclerotic stroma [Fig.2]. Many neoplastic cells exhibited prominent cytoplasmic vacuolization as an expression of primitive vascular differentiation. Tumor cells were immunoreactive for CD34 and CD31 demonstrating endothelial differentiation [Fig.3]. Biopsy was reported as vascular neoplasia; possibly HEHE.
Clinical presentation pointed towards a diagnosis of diffuse HEHE with portal hypertension. Thus, LT was considered. Living donor liver transplantation was performed from her father in January 2012. The transplant was uneventful. The explanted liver, measured 20x19x8 cm and weighed 651 gm. The tumor was multifocal and involved both lobes of the liver diffusely. Cut surface revealed multiple hemorrhagic solid nodules.
Histologically there was growth of the malignant endothelial cells along the hepatic sinusoids and venules. The tumor cells were usually spindle shaped with enlarged, hyperchromatic nuclei. The dilated sinusoids formed irregular cavernous blood–filled spaces. Large atypical hyperchromatic endothelial cells were lining the hepatic sinosoids. The histopathological examination for the resected specimen yielded the final diagnosis of diffuse angiosarcoma with necrosis and invasion of small veins. Following liver transplantation, the patient was treated with standard immunosuppressive therapy. Two years after transplantation, she is well, with normal liver function.
Discussion
HEHE is a rare neoplasm of vascular origin. It generally presents with poor clinical signs. Patients have generally nonspecific symptoms such as epigastric pain or right upper quadrant, weight loss and weakness. Jaundice, fever and fatigue are less common symptoms at initial presentation. Suggested therapeutic approaches in HEHE are partial hepatectomy, orthotopic liver transplantation and chemotherapy [6,9,10,11].
Angiosarcoma is the most common primary sarcoma in the liver accounting for up to 0.2% to 2% of primary liver tumors [13]. It commonly affects patients at 60 to 70 years of age but also rarely affects younger patients too [13,14]. A strong male predominance has been reported, with a male-female ratio of 4:1 [14]. Primary sarcomas of the liver are rare tumors . Although LT can be indicated in some cases of HEHE because of a favorable long term outcome [1,8], it is not advised for AS owing to a high risk of early local or general recurrence rate after LT [7]. The distinction between AS and HEHE remains a delicate issue, especially on a percutaneous liver biopsy. Also, the amount of tumor tissue was too small to make a definite diagnosis. The primary diagnosis was based on the presence of positive endothelial markers in malignant cells of a hepatic tumor. The diagnosis of HEHE are nodes formed by a hyaline stroma, epithelioid cells with intracytoplasmic red blood cell inclusions and sometimes calcifications (which are not present in HAS) [15]. The histological characteristic of HAS is the presence of atypical tumoral cells at the edge of the sinusoids, often with vascular dilatations or rarely nodular solid tumors. Metastases are found frequently at the time of the diagnosis, mainly located in the spleen, lung and bones. MRI or CT scans may show a multinodular tumor or a mass syndrome, or more rarely a diffuse infiltration of the liver [16]. Diagnosis of hepatic angiosarcoma can be made by biopsy that needs adequate and representative tissue, which sometimes can only be obtained during laparotomy [17]. In this case; preoperative liver biopsy pointed towards a diagnosis of diffuse HEHE but the histopathological examination of the resected specimen revealed the final diagnosis as diffuse angiosarcoma with necrosis and invasion of the centrilobular veins.
Overall prognosis of hepatic angiosarcoma is very poor regardless of the treatment with surgery, chemotherapy, or radiation. The mean survival noted in the literature is 10 months to 2 years [18]. The role of liver transplantation is contentious. In some reports, it has been abandoned because of high recurrence rate with poor survival [7,19,20].
Indeed, early diagnosis is very rare, tumor biology of HAS is very poorly understood, and effective chemotherapy and radiotherapy is lacking because HAS is radioresistant and an established chemotherapy regimen is not available [7,17]. The combination of chemotherapy and antiangiogenic-based immunosuppression, using rapamycin, needs to be investigated [7, 21, 22].
In this report, a case of hepatic angiosarcoma treated by orthotopic liver transplantation in Turkey is presented. Our report is not to suggest LT for HAS, based on this unusual case study, but rather to optimize the management of such patients. We report an atypical clinical observation, which is especially interesting in that it illustrates the difficulty in distinguishing the two forms of primary sarcoma of the liver.
References
- Adam R, McMaster P, O’Grady JG, Castaing D, Klempnauer JL, Jamieson N, et al. Evolution of liver transplantation in Europe: report of the European Liver Transplant Registry. Liver Transpl. 2003;9:1231-1243.
- Weitz J, Klimstra DS, Cymes K, Jarnagin WR, D’Angelica M, La Quaglia MP, et al. Management of primary liver sarcomas. Cancer. 2007;109:1391-1396.
- Weiss SW, Enzinger FM. Epithelioid hemangioendothelioma: A vascular tumor often mistaken for a carcinoma. Cancer. 1982;50:970-981.
- Lee KC, Ng WF, Chan JK. Epithelioid haemangioendothelioma presenting as a gastric polyp. Histopathology. 1988;12:335-337.
- Mehrabi A, Kashfi A, Fonouni H, Schemmer P, Schmied BM, Hallscheidt P, et al. Primary malignant hepatic epithelioid hemangioendothelioma: A comprehensive review of the literature with emphasis on the surgical therapy. Cancer. 2006;107:2108-2121.
- Makhlouf HR, Ishak KG, Goodman ZD. Epithelioid hemangioendothelioma of the liver: A clinicopathologic study of 137 cases. Cancer. 1999;85:562-582.
- Maluf D, Cotterell A, Clark B, Stravitz T, Kauffman HM, Fisher RA. Hepatic angiosarcoma and liver transplantation: case report and literature review. Transplant Proc. 2005;37:2195-2199.
- Lerut JP1, Orlando G, Sempoux C, Ciccarelli O, Van Beers BE, Danse E, et al. Hepatic haemangioendothelioma in adults: excellent outcome following liver transplantation. Transpl Int. 2004;17:202-207.
- Ishak KG, Sesterhenn IA, Goodman ZD, Rabin L, Stromeyer FW. Epithelioid hemangioendothelioma of the liver: a clinicopathologic and follow-up study of 32 cases. Hum Pathol. 1984;15:839-852.
- Bancel B, Patricot LM, Caillon P, Ducerf C, Pouyet M. Hepatic epithelioid hemangioendothelioma. A case with liver transplantation. Review of the literature. Ann Pathol. 1993; 13:23-28.
- Läuffer JM1, Zimmermann A, Krähenbühl L, Triller J, Baer HU. Epithelioid hemangioendothelioma of the liver. Cancer. 1996;78:2318-2327.
- Aizawa Y, Watanabe F, Fujise K, Watanabe R, Iemoto Y, Isikawa T, et al. A case of epithelioid hemangioendothelioma of the liver diagnosed by liver biopsy under laparoscopy and treated with interleukin 2 (IL2). Nippon Shokakibyo Gakkai Zasshi. 1991;88:2904-2909.
- Orlando G, Adam R, Mirza D, et al. Hepatic Hemangiosarcoma: An absolute contraindication to liver transplantation- The European liver transplant registry experience. Transplantation 2013;95:872-877.
- Locker GY, Doroshow JH, Zwelling LA, et al. The clinical features of hepatic angiosarcoma: a report of four cases and a review of the English literature. Medicine 1979;58:48.
- Soslow RA, Yin P, Steinberg CR, Yang GC. Cytopathologic features of hepatic epithelioid hemangioendothelioma. Diagn Cytopathol. 1997;17:50-53.
- Koyama T, Fletcher JG, Johnson CD, Kuo MS, Notohara K, Burgart LJ. Primary hepatic angiosarcoma: findings at CT and MR imaging. Radiology. 2002;222:667-673.
- Dimashkieh HH, Mo JQ, Wyatt-Ashmead J, Collins MH. Pediatric hepatic angiosarcoma: case report and review of the literature. Pediatr Dev Pathol. 2004;7:527-532.
- Emre S, Mckenna GJ. Liver tumors in children. Pediatr Transplant. 2004;8:632-638.
- Bien E, Stachowicz-Stencel T, Balcerska A, Godzinski J, Kazanowska B, Perek-Polnik M, et al. Angiosarcoma in children-still uncontrollable oncological problem. The report of the Polish Pediatric Rare Tumours Study. Eur J Cancer Care. 2009;18:411-420.
- Awans S, Davenport M, Portmann B, Howard ER. Angiosarcoma of liver in children. J Ped Surg. 1996;31:1729-1732.
- Budd GT. Management of angiosarcoma. Curr Oncol Rep. 2002;4:515.
- Kim HR, Rha SY, Cheon SH ,Roh JK, Park YN, Yoo NC. Clinical features and treatment outcomes of advanced primary hepatic angiosarcoma. Ann Oncol. 2009;20:780.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
Bostanci EB, Öter V, Ulas M, Turhan N, Ökten SLiving Donor Liver Transplantation To Primary Sarcoma of the Liver.JCR 2014;4:400-404 |
|
Bostanci EB, Öter V, Ulas M, Turhan N, Ökten SLiving Donor Liver Transplantation To Primary Sarcoma of the Liver.JCR [serial online] 2014[cited 2025 May 11];4:400-404. Available from: http://www.casereports.in/articles/4/2/Living-Donor-Liver-Transplantation-To-Primary-Sarcoma-of-the-Liver.html |

|
|
|
|
|