|
|
|
|
|
Pregnancy in a case of Klippel Trenaunay Syndrome: A Case Report and Review of Literature
|
|
|
Sunita Gupta, Charu Sharma, Geetika Tomar, Abhishek Bhardwaj1
From the Department of Obstetrics and Gynecology and Dermatology1, Subharti Medical College Meerut, Uttar Pradesh, India. |
|
|
|
|
|
Corresponding Author:
|
Dr. Charu Sharma
Email: sharma.charu651@gmail.com
|
|
|
|
|
|
|
|
|
Received:
10-OCT-2014 |
Accepted:
28-NOV-2014 |
Published Online:
20-DEC-2014 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
We are describing here a rare case of pregnancy in a patient of Klippel-Trenaunay syndrome (KTS). She was an unbooked case and her pregnancy was uneventful. The patient presented to emergency department in labor and her caesarean section was performed in view of contracted pelvis. Her intraoperative and post-operative period was uneventful. The clinical course and the risks of pregnancy in such a background are discussed. Given the rarity of the disease, there is little information available to counsel these patients regarding obstetric outcome. |
|
|
|
|
|
Keywords :
|
Klippel-Trenaunay-Weber Syndrome, Port-Wine stain, Hemangioma, Hyperostosis, Pregnancy, Humans.
|
|
|
|
|
|
|
|
|
|
|
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff5400060000002203000001000200 6go6ckt5b5idvals|403 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
Klippel Trenaunay syndrome is a rare congenital disorder characterized by a triad of congenital malformations including extensive cutaneous haemangioma (port wine stain), soft tissue or bone hypertrophy affecting a leg and/or arm on one side and venous varicosities [1]. When associated with arteriovenous fistulas, it is known as Klippel Trenaunay Weber syndrome (KTWS) [2]. KTS is often associated with massive hemorrhage, thrombosis and pulmonary embolism due to the rupture of superficial and deep arteriovenous malformations (AVMs) during surgery [1]. It affects females and males equally and presents at birth or during early infancy or childhood. International reports estimate an incidence of 2-5 cases per 100,000 live births. There is no national record of such cases in India. Although Klippel-Trenaunay syndrome probably has a genetic background, it is very rare for more than one person in a family to be affected. Literature quotes only one example of sibling involvement [2]. In our patient there was no family history of KTS.
Pregnancy has been rarely reported in patients with KTS and to the best of our knowledge, literature includes only 20 reports of pregnancy complicated by KTS [1] and none reported from India. Usually pregnancy is discouraged because this rare disease puts a pregnant woman at increased obstetric risks of deep venous thrombosis (DVT), thromboembolism and hemorrhage, intra-uterine growth restriction etc. We present here a case of pregnancy with KTS which was diagnosed just prior to delivery when she came with labor pains in emergency department.
Case Report
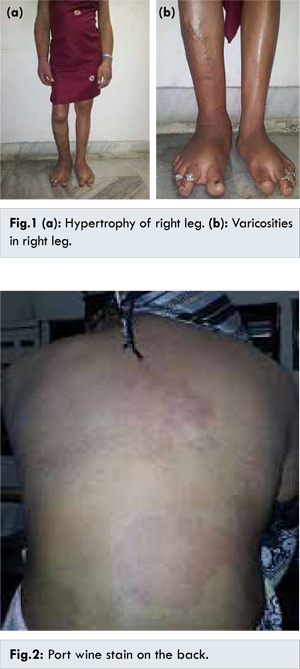
A 22 years old, unbooked primigravida presented in emergency at term gestation with labor pains. She had an abnormal built of body since birth for which she never consulted any clinician. She had right sided hemi-hypertrophy of the body below neck [Fig.1a] leading to scoliosis of thoracolumbar spine. There was also hypertrophy of left palm and sole. Varicose veins were present in both the legs, more in right leg [Fig.1b]. Large port wine stains were present on the back and right hypochondriac region [Fig.2]. Preoperative investigations including the coagulation profile were all within normal limits. She was taken up for an emergency caesarean section in view of contracted pelvis. Low transverse abdominal incision under general anesthesia was given and she delivered a healthy male baby of 3 kg. Intra-operative and post-operative period was uneventful. No abnormal finding indicative of neonatal KTS was seen. Elastic stockings and low-molecular weight heparin (40 mg/day) injection was administered subcutaneously for seven postoperative days as prophylaxis to prevent DVT. The patient was discharged with her baby in good health on 8th postoperative day. She accepted lactational amenorrhea method for contraception. She did not have any unfavorable event in life till date. She was counseled and referred for specific treatment of her vascular abnormalities.
We did not encounter any complication during cesarean section, but in the post-operative period we should be aware of the possible complications related to this syndrome. Given the rarity of the disease, there is little information available to discuss and counsel the patients regarding effects of Klippel-Trenaunay syndrome on maternal physiology and fetal outcome. Four cases reported by Rebarber Andrei et al. had successful delivery of healthy infants at or beyond 36 weeks of gestation with one having pulmonary embolism in post-operative period [4]. G. Fait et al. reported a case, who on two occasions delivered small for gestational age neonates [5]. Our patient delivered a baby by LSCS that was appropriate for gestational age.
Early identification of such patients presenting directly to obstetrics department is important and depends on prior knowledge of such syndrome. The diagnosis is based on clinical evidence. At least two of the three criterias discussed above must be fulfilled [4]. Our patient had all the three features. We were unaware of such a case and hence diagnosis of KTS was not made in emergency department and preliminary necessary precautions could not be taken.
Hemangiomas associated with KTS may involve any part of body including abdominal viscera like liver, spleen, uterus etc. leading to sometimes acute abdomen with hemoperitoneum with even slight trauma, that may occur while conducting delivery. Vulval hemangioma should be excluded while planning such patients for vaginal deliveries as cases of DIC with abnormal haemorrhage because of such vessels have been reported [1]. To prevent these complications, MRI should be done to determine the existence of abnormal vessels in the pelvis, birth canal or spinal cord before delivery so as to decide the mode of delivery [1]. If neuraxial vascular anomalies cannot be ruled out radio graphically, regional anesthesia should be avoided. The literature also recommends avoidance of epidural or spinal analgesia because of the risk of spinal hematoma [1]. Because our patient had severe scoliosis, general anesthesia was given and complications related to regional anaesthesia were avoided.
Additionally, regardless of the anesthetic technique chosen, the coagulation profile of these patients should be verified for signs of coagulopathy. One report regarding cutaneous hemangiomas sequestering platelets, leading to Kasabach-Merritt syndrome, a type of consumptive coagulopathy is also present, [6] so prior to any operative procedure one must get the platelet count done.
Patients with the Klippel-Trenaunay syndrome have an increased risk of thromboembolism [1] and in one survey of 252 patients, 20 (8%) patients had pulmonary embolism or deep vein thrombosis [4]. Hence, long term anticoagulation in such patients is advocated during pregnancy to prevent thromboembolism [1]. As there is currently no cure for Klippel-Trenaunay syndrome, treatment aims to relieve symptoms and prevent disabilities. In mild forms of the disease, elastic stockings are advised to prevent oedema [2]. Hypertrophy of a limb may lead to subsequent vertebral scoliosis, gait abnormalities, and compromise of function, hence surgical correction has been described in few studies [2]. We advised our patient for elastic compression stockings and gave her prophylactic low molecular weight heparin. On follow up after six weeks, the patient had no problem.
References
- Tanaka R, Fujita Y, Hiasa KI, Yumoto Y, Hidaka N, Fukushima K, et al. Successful management of pregnancy complicated by Klippel- Trenaunay Syndrome using MR angiography based evaluation. Case reports in Obstetrics and Gynaecology. 2011, Article ID 723467, 4 pages.
- Heydanus R, Wladimiroff JW, Bradenburg H, Gaillard JLJ. Prenatal diagnosis of Klippel Trenaunay Weber Syndrome: a case report. Ultrasound Obstet Gynecol. 1992;2:360-363.
- Rebarber A, Roman AS, Roshan D, Francine B. Obstetric Management of Klippel Trenaunay Syndrome. Obstet Gynecol. 2004;104:1205-1208.
- Watermeyer SR, Davies N, Goodwin R. The Klippel–Trenaunay syndrome in pregnancy. BJOG: an International Journal of Obstetrics and Gynecology. 2002;109:1301-1302.
- Fait G, Daniel Y, Kupfermine MJ, Gull I, Peyser MR, Lessing JB. Klippel Trenaunay Weber Syndrome associated with fetal growth restriction. Human Reproduction. 1996;11:2544-2545.
- David W. Barbara, Jack L. Wilson Anesthesia for Surgery Related to Klippel–Trenaunay Syndrome: A Review of 136 Anesthetics. Journal of anesthesia and analgesia. 2011;113(1):98-102.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
Gupta S, Sharma C, Tomar G, Bhardwaj APregnancy in a case of Klippel Trenaunay Syndrome: A Case Report and Review of Literature.JCR 2014;4:491-494 |
|
Gupta S, Sharma C, Tomar G, Bhardwaj APregnancy in a case of Klippel Trenaunay Syndrome: A Case Report and Review of Literature.JCR [serial online] 2014[cited 2026 Feb 23];4:491-494. Available from: http://www.casereports.in/articles/4/2/Pregnancy-in-a-case-of-Klippel-Trenaunay-Syndrome.html |

|
|
|
|
|