|
|
|
|
|
Rapid Transition from Subclinical Hypothyroidism to Hyperthyroidism
|
|
|
amlodipin sandoz 5 mg amlodipin teva link
From the 1Department of Biochemistry & Laboratory Services and 2Department of Endocrinology, The Mission Hospital, Durgapur, West Bengal, India. |
|
|
|
|
|
Corresponding Author:
|
Dr. Moushumi Lodh
Email: drmoushumilodh@gmail.com
|
|
|
|
|
|
|
|
|
Received:
24-JUN-2014 |
Accepted:
09-SEP-2014 |
Published Online:
10-OCT-2014 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
Subclinical thyroid dysfunction is defined as an abnormal serum thyroid stimulating hormone level and free thyroxine and triiodothyronine levels within their reference ranges. We report here a case of otherwise asymptomatic subclinical hypothyroidism, who progressed to overt hyperthyroidism within a span of one year, with tremors, heat intolerance and fidgetiness. If a patient on levothyroxine for autoimmune hypothyroidism on replacement therapy presents with hyperthyroidism, the possibility of endogenous hyperthyroidism should also be considered. |
|
|
|
|
|
Keywords :
|
Graves Disease, Hashimoto Disease, Autoimmune thyroiditis, Hypothyroidism, Thyroxine, Tremor.
|
|
|
|
|
|
|
|
|
|
|
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff44f8050000003403000001000100 6go6ckt5b5idvals|374 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
Reversible hypothyroidism is known to occur in the following situations: antithyroid drug and iodine administration, subacute thyroiditis, auto-immune chronic thyroiditis (transition from hypothyroid to hyperthyroid state after delivery and when treatment with cortisol is initiated in Schmidt’s syndrome), on stopping long term treatment with thyroid hormone, post-operatively in Graves’ disease, after radio-iodine treatment, initial primary hypothyroidism changing to Graves’ disease, spontaneous recovery from hypothalamic disease and in newborn infants. We describe below a case that was initially hypothyroid but became hyperthyroid under observation for one year only.
Case Report
A thirty four year old male, employed with a central government job, reported to a doctor in the community for occasional chest pain and gastritis. There was no family history of diabetes mellitus, hypertension although his mother was a known hypothyroid, on treatment, since fifty four years of age. The patient had not had any surgery or treatment for any major illness. He was married since five years with a three year old daughter. He was tested for thyroid function test in addition to a battery of tests which picked up subclinical hypothyroidism. In view of subclinical hypothyroidism he was followed closely as antithyroid peroxidase antibody was significantly high.
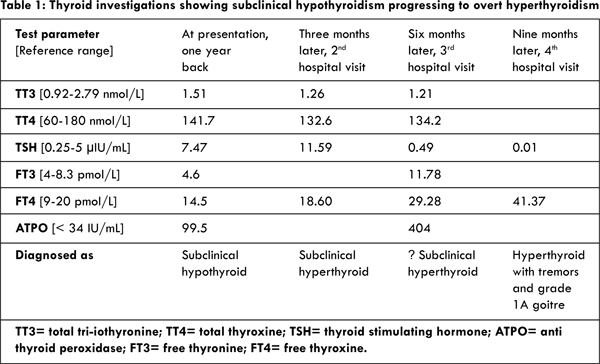
Routine examination revealed his weight to be 54 kg, height 179 cm, blood pressure 110/70 mm Hg and pulse 80/minute. His fasting plasma glucose, serum creatinine, cholesterol, triglyceride and total bilirubin were within reference range. However, low density lipoprotein cholesterol was 132 mg/dL (reference range <100). Ultrasonography of the thyroid gland showed no obvious abnormality. The thyroid function tests were performed at first visit and repeated at every visit. He was advised levothyroxine 50 mg once a day in empty stomach for three months. Third visit in the hospital interestingly showed a change in his thyroid function parameters, swing from subclinical hypo to hyperthyroidism [Table 1]. Levothyroxine was stopped. On his fourth visit, he displayed fine tremors, heat intolerance and fidgetiness. There was grade 1A goitre but no marked change in body weight. Ultrasonography of the thyroid gland showed no obvious abnormality. Doppler study showed no abnormal vascularity of the thyroid, spectral flow and velocity were within normal limits. In view of his frank biochemical parameters, he was started on carbimazole tablet 10 mg once a day for one month.
Subclinical hypothyroidism is found in approximately 2 percent of the population [1]. The two main disorders that comprise autoimmune thyroid disease are Hashimoto thyroiditis and Grave’s disease. Hashimoto thyroiditis is the most common cause of hypothyroidism, whereas Grave’s disease is a major cause of hyperthyroidism. Occasionally, a patient may present with features of one of these disorders at one time and features of the other at another time. The usual sequence is hyperthyroidism followed by hypothyroidism. Graves’ disease may result eventually in hypothyroidism in approximately 5-20% of patients. [2].
However, cases of hypothyroidism followed by hyperthyroidism, such as in our patient, have also been described. Takasu et al. described eight cases of autoimmune thyroid disease with an alternating pattern of thyroid function [3]. In five cases, hypothyroidism was followed by transient hyperthyroidism. In two other cases, hypothyroidism was followed by persistent hyperthyroidism, and in one case hypothyroidism was associated with thyroid-stimulating antibodies, a characteristic finding in Graves’s disease. Alzahrani describes Grave’s disease after many years of hypothyroidism followed by a similar period of euthyroidism in a female [4].
Suggested cause of the change over from hypothyroid to hyperthyroid state is the damage of thyroid cells by autoimmune process with a consequent increase in pituitary TSH secretion. This fails to keep the patient euthyroid as TSH blocking antibodies render TSH ineffective. The transition from TSH blocking antibodies to thyroid stimulation antibodies may be the cause of hyperthyroidism in some cases. Alternatively, PGE and PGF released by lymphocytes in the thyroid might cause thyroid hyperplasia and hyperthyroidism [5]. Progression of subclinical hypothyroidism to overt hypothyroidism occurs at a rate of about 5 percent per year in patients with raised TSH levels and detectable antithyroid antibodies [6]. In elderly patients with high titers of antithyroid antibodies, the risk of progression to overt disease may be closer to twenty percent per year [7].
Our patient clearly demonstrated the fact that subclinical hypothyroid patients should be followed regularly for few years, and the development of clinical and/or biochemical hyperthyroidism should alert the physician to the possibility of another thyroid disease, especially those having a high anti-TPO antibody titre. During our patient’s progression from subclinical hypo to hyperthyroidism we waited for another 3 months just to be sure what is happening with his thyroid.
Rarely, autoimmune hyperthyroidism can occur after hypothyroidism in patients with Hashimoto thyroiditis. When a patient on levothyroxine for Hashimoto hypothyroidism presents with hyperthyroidism, over-replacement with levothyroxine is the likely cause, but the possibility of endogenous hyperthyroidism
should also be considered.
Conclusion
Rarely, autoimmune hyperthyroidism can occur after hypothyroidism in patients with Hashimoto thyroiditis. When a patient on levothyroxine for Hashimoto hypothyroidism presents with hyperthyroidism, over-replacement with levothyroxine is the likely cause, but the possibility of endogenous hyperthyroidism should also be considered.
References
- Wilson GR, Curry RW. Subclinical thyroid disease. Am Fam Physician. 2005;72(8):1517-1524.
- Tamai H, Kasagi K, Takaichi Y, Takamatsu J, Komaki G, Matsubayashi S, et al. Development of spontaneous hypothyroidism in patients with Graves’ disease treated with antithyroidal drugs: clinical, immunological, and histological findings in 26 patients. Clin Endocrinol Metab. 1989;69(1):49-53.
- Takasu N, Yamada T, Sato A, Nakagawa M, Komiya I, Nagasawa Y, et al. Graves’ disease following hypothyroidism due to Hashimoto’s disease: Studies of eight cases. Clin Endocrinol (Oxf). 1990;33:687-698.
- Alzahrani AS, Aldasouqi S, Salam SA, Sultan A. Autoimmune thyroid disease with ?uctuating thyroid function. PLoS Med. 2005;2(5):e89.
- Bhandarkar SD, Retnam VJ. Hyperthyroidism following hypothyroidism. JPGM. 1980;26(1):90-94.
- Tunbridge WM, Brewis M, French JM, Appleton D, Bird T, Clark F, et al. Natural history of autoimmune thyroiditis. Br Med J [Clin Res]. 1981; 282:258-262.
- Rosenthal MJ, Hunt WC, Garry PJ, Goodwin JS. Thyroid failure in the elderly. Microsomal antibodies as discriminant for therapy. JAMA. 1987;258:209-213.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
Lodh M, Mukhopadhyay RRapid Transition from Subclinical Hypothyroidism to Hyperthyroidism.JCR 2014;4:383-386 |
|
Lodh M, Mukhopadhyay RRapid Transition from Subclinical Hypothyroidism to Hyperthyroidism.JCR [serial online] 2014[cited 2026 Feb 5];4:383-386. Available from: http://www.casereports.in/articles/4/2/Rapid-Transition-from-Subclinical-Hypothyroidism-to-Hyperthyroidism.html |

|
|
|
|
|