6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff2cf8050000002103000001000600
6go6ckt5b5idvals|368
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Introduction
Subgaleal hematoma (SGH) is an unusual type of birth trauma, and commonly it is associated with assisted delivery by instrumentation (vacuum and/or forceps) [1]. The most commonly associated clinical problems with mortality are due to severe hypovolemia and coagulopathy, but not intracranial hemorrhage (ICH). Careful assessment and monitoring of the infant following birth is necessary to ensure prompt intervention, referral, and improved outcomes [2]. Additional care, planning, and communication are especially important in the transport environment. A brain computed tomography or Magnetic Resonance Imaging should be considered in evaluating a clinically symptomatic SGH to delineate the extent of extra and intracranial hemorrhage, there is associated mortality in severe cases if not cared seriously, but short-term outcome in survivors is good [2].
Case Report
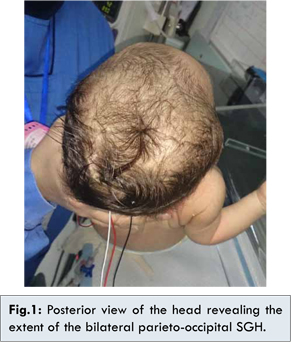
During the routine physical examination of newborn babies in the nursery, the case was: A full term female newborn, with abnormal and asymmetric head shape despite being totally normal at birth as I was the attending neonatologist who has attended her non traumatic birth by an elective, programmed and smooth cesarean section. During her evaluation, we noticed that she had three swellings over the right and left parietal areas and over the right temporo-occipital bones, which were firm, elevated and crossed the suture lines with increase of the head circumference from 35 to 36 cm [Fig.1].
There was no ecchymosis or other sites of hemorrhages, neither history nor signs of external trauma or report of uterine contraction. Further positive findings to be noted were her yellowish, pale color due to early jaundice despite the absence of blood group incompatibility, and the presence of a holosystolic ejection murmur over the left lower sternal border of 2/6 intensity without further added heart sounds.
So, the origin of the scalp masses most probably was due to non-traumatic encephalohematomas or subgaleal bleedings, and could it be the cause of anemia with decrease of her hematocrit to 27%, and subsequent indirect hyperbilirubinemia, also causing the hyperdynamic heart murmur? And what are the underlying causes of such spontaneous bleeding?
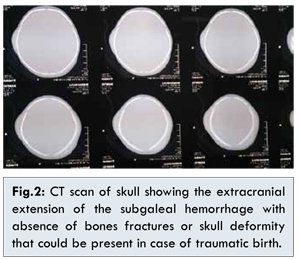
The baby was admitted to NICU at the age of 2 day of life for evaluation and management: our primary aim was to determine the extent of the cranial bleeding, detect possible intracranial bleeding and to find out if there is any bleeding disorder; given her stable neurological and hemodynamic status, with no vomiting, RDS, or abnormal movement we requested a cranial CT scan first that showed the presence of the subgaleal hematomas with no fractures or internal bleeding [Fig.2]. Serial complete blood count revealed progressive decrease of her hematocrit to 33% and down to 27% which is far below the normal range, PT, PTT, fibrinogen, clotting time, bleeding time, factor XIII, LFT’s were all normal except for elevated bilirubin level. The echocardiography showed a moderate sized, apical ventricular septal defect of 5 mm with normal cardiac function and structures. Fundoscopy to find out any retinal hemorrhage, was normal as the abdominal ultrasonogram, so, she received blood transfusion of 40 cc of red cell concentrate, to stabilize her hematocrit and prophylactic phototherapy and discharged home at the age of 5 day of life with stable hemodynamic condition as per admission, stable hematocrit level and normal neurological exam, with a stable head circumference measurements. Follow up assessment at 1 month of age revealed normalization of her head shape and contour.
Discussion
Extracranial hemorrhage (ECH) is one of the common complications of instrumental deliveries. However, it can occur in all modes of delivery, even in utero prior to the onset of labor [1,3]. Based on scalp anatomy and clinical presentation, hemorrhages deep in the scalp and outside the calvarium are categorized into cephalhematoma, subgaleal hemorrhage and caput succedaneum. The incidence of subgaleal hemorrhage has been estimated to be 1 in 2,000 normal vaginal deliveries; it increases to 1 in 200 cases of vacuum assisted deliveries, the likelihood of this injury is increased with multiple applications of the vacuum cup and reported “pop offs.”
A subgaleal hemorrhage can be noted at birth, or can appear gradually over the first hours. The diagnosis is clinical in many cases, with an enlarging head due to swelling which crosses suture lines, ending at the orbits anteriorly and at the nape of the neck posteriorly, and accompanied by clinical and laboratory evidence of diminishing circulating blood volume. Symptoms can include respiratory distress, anemia, hypovolemic shock, pallor, hypotension, acidosis and jaundice [1,3].
The pathogenesis of neonatal subgaleal hemorrhage involves trauma to the scalp. The subgaleal space is a potential space, meaning two adjacent tissues, not tightly adjoined, can be separated to create a previously non-existent cavity [2]. The two tissues bordering the subgaleal space are the periosteum of the skull and the flat broad tendinous material covering the cranium called the galea aponeurotica. The subgaleal space can fill with blood following rupture of veins that connect scalp veins to the dural sinus. Veins traversing this potential space, termed emissary veins, can rupture after twisting, sheering, or torsion of the scalp [3]. The subgaleal space of a neonate can accommodate 50-80% of the blood volume, and consequently massive bleeding can occur into this space, resulting in hypovolemic shock. To estimate the volume of blood loss in this space, compare the head circumference at birth with the head circumference at presentation. Estimation can be made by considering that each 1-cm increase in head circumference corresponds to 40 mL of blood loss in this space [4-6].
In the current case, SGH occurred in an infant with a non-traumatic cesarean delivery with no known associated-risk factors. Although SGH is often considered in traumatic or instrumented deliveries, our patient illustrates the important lesson that SGH should also be part of the differential diagnosis in infants with anemia and jaundice without hemolytic causes, despite a non-traumatic delivery. In addition, this case demonstrates that SGH in a non-instrumented delivery should prompt an evaluation for bleeding disorders. Although there are rare case reports of SGH in patients with hemophilia, our patient was unique in that his coagulopathy was completely normal with normal coagulation profile tests values including level of FXIII.
Management of neonatal subgaleal hemorrhage involves NICU monitoring and serial quantification of the hemoglobin or hematocrit. Monitoring includes a minimum of 8 hours’ observation for all babies following difficult vacuum extractions or forceps deliveries, regardless of Apgar score or need for resuscitation [4,5]. This observation should include at least hourly recording of vital signs. Examination of the head, including the circumference of the head and assessment of the location and characteristics of any swelling, should be repeated hourly if concerns are present. Using these features to aid early recognition is an important key to intact survival. Hemoglobin measurement should be performed as soon as possible and should be monitored every 4–8 hours, as should coagulation studies. Although it is not necessary to make the clinical diagnosis, optimal imaging for subgaleal hemorrhage is by CT or MRI [2-4].
Acute volume resuscitation should be undertaken initially with normal saline as 10 mL/kg bolus infusions followed by emergent whole blood or packed red blood cell transfusion. O-negative blood available for emergency use should be accessed and fresh frozen plasma used initially for a developing coagulopathy [6]. Serial hematocrits and blood pressure should be monitored closely. It is critically important to maintain stable hemodynamics and assure adequate organ perfusion. Pressors should be added (dopamine 5 to 20 mcg/kg per minute) if volume alone is not sufficient or there is coexisting cardiac decompensation [5,6].
Most neonates with a subgaleal hemorrhage have a good outcome, and perhaps this is improving over time. For instance, the mortality rate in a recent Taiwan study was 12% in contrast to earlier reports where mortality rates of 17 to 25% were cited. Neurodevelopmental problems were present in 17% in the same Taiwan report [6].
Conclusion
Subgaleal hematoma is a serious neonatal emergency especially after device assisted deliveries. Non traumatic caesarean could also be associated with SGH, where investigations for bleeding disorder should be performed. Early recognition of the condition and appropriate time referral to NICU after birth will improve the clinical and neurological outcomes and decrease mortality rate.
References
- Abroms IF, Rosen BA. Neurologic trauma in newborn infants. Semin Neurol 1993;13:100-105.
- Davis DJ. Neonatal subgaleal hemorrhage: diagnosis and management, CMAJ. 2001;164(10):1452-1453.
- Rosenberg AA. Traumatic birth injury. Neoreviews 2003;4:e270-e276.
- Kilani RA, Wetmore J. Neonatal subgaleal hematoma: presentation and outcome-radiological findings and factors associated with mortality. Am J Perinatol 2006;23(1):41-48.
- Schierholz E, Walker SR. Responding to traumatic birth: subgaleal hemorrhage, assessment, and management during transport. Adv Neonatal Care 2010;10(6):311-315.
- Christensen RD. Neonatal subgaleal hemorrhage in a multihospital healthcare system: prevalence, associations, and outcomes, e-Journal of Neonatology Research Volume 1, Issue 1, Spring 2011.