|
|
|
|
|
Unusual Presentation of Papillary Renal Cell Carcinoma
|
|
|
asthma rescue inhaler otc inhalers for copd read here
From the 1Department of Urology, KLES Kidney Foundation, 2Department of Pathology, KLE University’s JN Medical College, KLES Dr Prabhakar Kore Hospital & MRC, Belgaum, India 590010. |
|
|
|
|
|
Corresponding Author:
|
Dr. Ajay Kumar G
Email: drajay707@gmail.com
|
|
|
|
|
|
|
|
|
Received:
22-APR-2014 |
Accepted:
17-JUL-2014 |
Published Online:
20-AUG-2014 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
Papillary renal cell carcinoma (pRCC) is the second most frequent renal cell carcinoma (RCC) subtype, accounting for approximately 13–15% of all known RCC lesions. We report a case of papillary renal cell carcinoma presented clinically and radiologically like that of a transitional cell carcinoma of renal pelvis in a 62 year old male. |
|
|
|
|
|
Keywords :
|
Kidney, Renal cell carcinoma, Flank Pain, Hematuria, Kidney Neoplasms, Abdomen.
|
|
|
|
|
|
|
|
|
|
|
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff54f0050000001903000001000900 6go6ckt5b5idvals|355 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
Renal cell carcinoma (RCC) accounts for nearly 3% of all solid tumors [1]. It is estimated that approximately 46,000 new cases of RCC were diagnosed in 2008. Most RCCs are incidentally diagnosed at imaging. The number of cases diagnosed by using the classic triad of hematuria, flank pain, and a mass in the abdomen continues to decline. The incidence of RCC is gradually increasing, partly due to increased use of imaging and partly due to the increasing incidence of obesity in the general population, a risk factor associated with increased incidence of RCC [2]. Papillary renal cell carcinoma (pRCC) is the second most frequent renal cell carcinoma (RCC) subtype, accounting for approximately 13-15% of all known RCC lesions [1]. We report a case of papillary renal cell carcinoma presented clinically and radiologically like that of a transitional cell carcinoma of renal pelvis.
Case Report
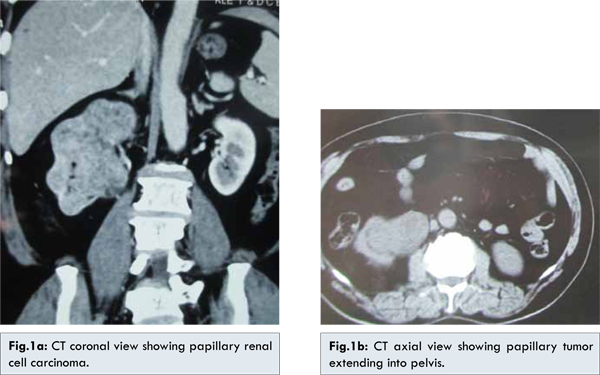
A 62 year old male presented with history of recurrent episodes of hematuria over the past two years. Hematuria was occasionally associated with right sided loin pain with and passage of clots. No radiation of pain was present. No other significant history noted. Urine examination revealed 10-15 RBCs/hpf with proteinuria. Urine cytology was negative for abnormal cells. Ultrasonography revealed a hypoechoic mass (6.1×6.1 cm) arising from the upper pole of the right kidney and extending into pelvis. Computed tomography (CT) [Fig.1a-c] showed a mixed density mass lesion with an enlarged kidney and extending into the pelvis and upper ureter and the opposite kidney was normal. A clinical diagnosis of transitional cell carcinoma of renal pelvis was made. Cystoscopy was done to rule out lower tract lesions. The patient underwent right sided radical nephroureterectomy retroperitoneally and the specimen sent for histopathology. Macroscopic examination of the specimen revealed an enlarged kidney (13x7x5 cm) with nodular surface. Cut sections showed the whole parenchyma was replaced by the neoplasm and the tumor extended into the renal pelvis and upper ureter. Histopathological examination [Fig.2a-d] revealed a malignant neoplasm composed of low columnar cells arranged in papillary fronds. The papillary projections consist of a central fibrovascular core lined by a single layer or a pseudostratefied layer of tumor cells. The fibrovascular cores contained variable number of foamy histiocytes along with sclerosis. Foamy histiocytes caused expansion of the fibrovascular cores. The presence of abundant foamy histiocytes is a helpful diagnostic feature since it is seen almost consistently with papillary renal carcinomas.
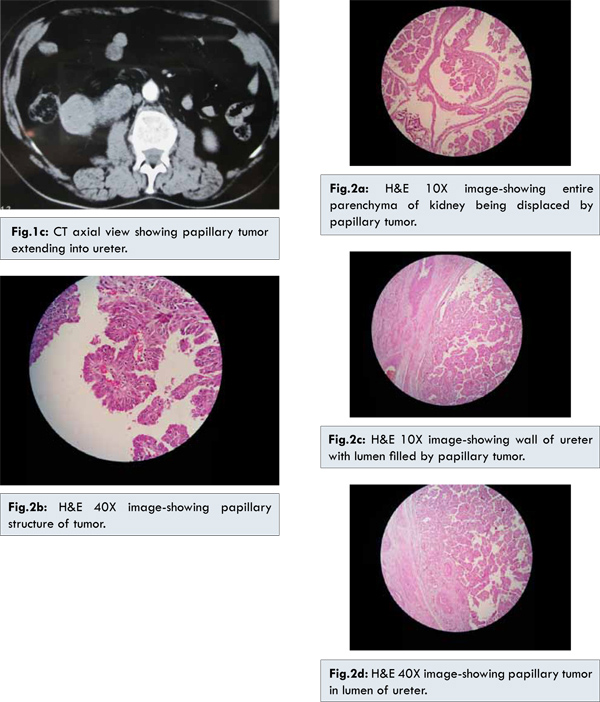
Papillary renal cell carcinoma (pRCC) is the second most frequent renal cell carcinoma (RCC) subtype, accounting for approximately 13-15% of all known RCC lesions [1]. Patients present in the third to eighth decades of life. The male-to-female ratio ranges from 2:1 to 3.9:1. Although most pRCCs are unilateral, pRCC is the most common multifocal or bilateral renal tumor [1]. Cytogenetic and molecular studies have revealed distinct findings in pRCC that allow differentiation from other renal epithelial tumors [3,4]. pRCCs are characterized by a papillary, tubular, or tubopapillary growth pattern. They are composed of cells arranged on a delicate fibro-vascular core. The cytoplasm may be basophilic, eosinophilic, or sometimes partially clear.
Our case was unique because the presentation clinically and radiologically was like that of a transitional cell carcinoma of renal pelvis. Only after sending the specimen for macroscopic and microscopic analysis with histopathology the diagnosis of papillary renal cell carcinoma was made. pRCC at diagnosis tends to be of smaller mean diameter and be of lower stage, when compared with cRCC (clear cell renal cell carcinoma). Delahunt et al. described two morphologic types of pRCC with different clinical behavior [5]. Type 1 tumors have papillae covered by a single layer of cuboidal or low columnar cells with scanty cytoplasm and low-grade nuclei. Type 2 tumors are of a higher nuclear grade and contain more than one layer of cells with abundant eosinophilic cytoplasm. Type 2 tumors generally carry a worse prognosis than type 1 tumors. Sarcomatoid dedifferentiation is seen in approximately 5% of pRCCs; it has been associated with both type 1 and type 2 tumors and is associated with a worse prognosis [6]. pRCC is known to be less vascular than cRCC. It was subsequently reported in several CT studies that pRCC typically enhances to a lesser degree than cRCC. The difference in the degree of enhancement between pRCC and cRCC is due to differences in the intratumoral vascularity, measured in terms of microvessel density (MVD) [7].
Conclusion
This case of pRCC presented clinically and radiologically like that of a transitional cell carcinoma of renal pelvis. This however made no major difference in surgical treatment. Such unusual presentations may mislead the clinician.
References
- Reuter VE. The pathology of renal epithelial neoplasms. Semin Oncol 2006;33:534-543.
- HuJ, Mao Y, White K. Canadian Cancer Registries Epidemiology Research Group. Overweight and obesity in adults and risk of renal cell carcinoma in Canada. Soz Praventivmed 2003;48:178-185.
- Presti JC Jr, Rao PH, Chen Q,V E Reuter,F P Li,W R Fair, et al. Histopathological, cytogenetic, and molecular characterization of renal cortical tumors. Cancer Res 1991;51:1544-1552.
- Yoshida MA, Ohyashiki K, Ochi H,Z Gibas, J E Pontes, G R Prout, et al. Cytogenetic studies of tumor tissue from patients with nonfamilial renal cell carcinoma. Cancer Res 1986;46:2139-2147.
- Delahunt B, Eble JN, McCredie MR, Bethwaite PB, Stewart JH, Bilous AM. Morphologic typing of papillary renal cell carcinoma: comparison of growth kinetics and patient survival in 66 cases. Hum Pathol 2001;32:590-595.
- Eble JN, Sauter G, Epstein JI, Sesterhenn IA. WHO classification of tumours: pathology and genetics of tumours of the urinary system and male genital organs. Paris, France: International Agency for Research on Cancer, 2004.
- Raghunandan V, Ng CS, Tamboli P, Tannir NM, Jonasch E, Matin SF, Wood CG, Sandler CM. Papillary Renal Cell Carcinoma: Radiologic-Pathologic Correlation and Spectrum of Disease. RadioGraphics 2009; 29:741-757.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
Kumar G A, RB Nerli, Malur P.Unusual Presentation of Papillary Renal Cell Carcinoma.JCR 2014;4:313-316 |
|
Kumar G A, RB Nerli, Malur P.Unusual Presentation of Papillary Renal Cell Carcinoma.JCR [serial online] 2014[cited 2026 Feb 21];4:313-316. Available from: http://www.casereports.in/articles/4/2/Unusual-Presentation-of-Papillary-Renal-Cell-Carcinoma.html |

|
|
|
|
|