|
|
|
|
|
An Unusual Cause of Acute Abdomen: Intestinal Ischemia due to Jejunal Heterotopic Pancreas
|
|
|
Murat Can Mollaoglu1, Sinan Soylu1, Birkan Bozkurt1, Hatice Reyhan Egilmez2, Mustafa Turan1
Department of 1General Surgery and 2Pathology, Cumhuriyet University, School of Medicine, Sivas, Turkey. |
|
|
|
|
|
Corresponding Author:
|
Dr. Birkan Bozkurt
Email: birkan.bozkurt@gmail.com
|
|
|
|
|
|
|
|
|
Received:
03-DEC-2014 |
Accepted:
16-FEB-2015 |
Published Online:
25-MAR-2015 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
Heterotopic pancreas is a defined as the case where pancreatic tissue is located outside its normal anatomical location. It is a congenital anomaly and often an incidental finding, and can be found at different sites in the gastrointestinal system. Jejunum is a rare localization for heterotopic pancreas. It is usually asymptomatic. Due to their origin and spread, these lesions form intramural masses with relatively late mucosal invasions and their diagnosis is difficult task through endoscopic technique and radiological imaging. In this case report, we are presenting the case of a 64 year-old male patient, due to its rare localisation and complication, who was taken under an urgent operation due to acute abdomen diagnosis, and who was diagnosed, during the operation, with jejunal heterotopic pancreas which causes segmental mesenteric ischemia. |
|
|
|
|
|
Keywords :
|
Pancreas, Jejunum, Mesenteric ischemia, Acute Abdomen, Congenital, Humans.
|
|
|
|
|
|
|
|
|
|
|
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ffa417060000008c03000001000400
6go6ckt5b5idvals|442
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Introduction
Heterotopic pancreas is a congenital anomaly where pancreas tissue is found in a different location than its anatomically normal location [1]. The literature indicates that it is found in 0.20-0.25% of all abdomen operations [2,3]. The condition is named in the literature with different terms such as aberrant pancreas, ectopic pancreas and accessory pancreas [4]. Inspite of appearing more frequently in stomach and duodenum, it also appears in jejunum, ileum, gall bladder, bile ducts, colon, spleen, omentum, urinary bladder, thorax and abdominal wall. It is an unusual condition in jejunum and usually asymptomatic [5]. In symptomatic cases, the heterotopic pancreas is mostly located in stomach and duodenum.
In this paper, we present and discuss, in line with the literature, the case of a 64 year-old male patient, due to its rare localisation and complication, who was admitted in emergency due to abdominal pain, and taken under operation with pre-diagnosis of mesenteric embolism as a result of radiologic examinations, and who was diagnosed, during the operation, with jejunal heterotopic pancreas which causes segmental mesenteric ischemia.
best quality Replica Breitling Canada with Swiss movements are worth having.
The Swiss knockoff website provides male and female wearers cheap and uk high end 2024 Cheap Replica Watches UK online.
Case Report
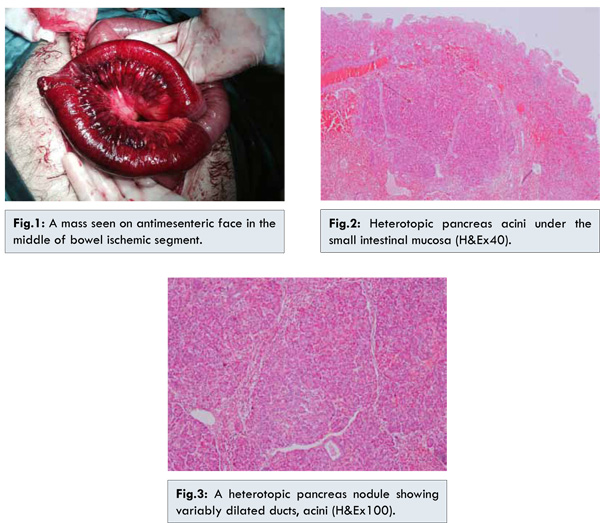
64 year-old male patient presented with history of nausea, pain abdomen and post-prandial vomiting for last three months. Initially he used to have 1-2 episodes of post-prandial vomiting, which progressively increased to 3-5 episodes over a period of three months. He experienced a weight loss of 8 kilograms in the same time. There was no history of abdominal distension, fever, haematemesis or melena. The physical examination of the patient indicated that there was tenderness and defence in all quadrants of the abdomen. The laboratory analysis showed no other findings than leucocytosis. The abdominal CT scan which was carried out indicated bowel loops which are thought to be resulting from undernourishment. The patient was urgently taken under operation with pre-diagnosis of acute abdomen due to mesenteric embolism. The exploration showed that the loop of small intestine with a size of 40 cm located 120 cm distal to ligament of Treitz was malnourished, and a mass of 3 cm was found on antimesenteric face in the middle of bowel ischemic segment [Fig.1]. The loop of small intestine along with mass was resected. The remaining small intestine loops were applied end-to-end anastomosis. The post-operative pathological examination indicated the existence of a submucosal tumoral lesion of 2.5x2 cm macroscopically located at 18.5 cm from a surgical border and at 19 cm from another one thickening the wall by 1.5 cm. The sectioning showed lobule formation created by pancreatic acinus ductus islets in submucosal and muscular layers. There was no atypia and dysplasia [Fig.2,3]. The patient who had a trouble-free condition in post-operative period was discharged on the 7th post-operative day.
Heterotopic pancreas is a defined as the case where pancreatic tissue is located outside its normal anatomical localisation [1]. Heterotopic pancreas was first defined by Jean Shultz in 1727 [6]. Klob conducted its histopathologic diagnosis in 1859 [7]. Heterotopic pancreas is usually asymptomatic. Nevertheless, it may occur along with symptoms such as nausea, vomiting and abdominal pain depending on the location of the lesion [8]. Most of the time, it is noticed incidentally during laparotomies carried out due to different reasons [10]. The most common localisation of heterotopic pancreas is stomach with a rate of 25-38.2% [11]. The lesion is mostly submucosal although it can occur as intramuscular and subserosal [8]. In our case, it was located in jejenum and subserosa at 120 cm distal to the ligament of Treitz.
Heterotopic pancreas may produce conditions such as pseudocyst formation and pancreatitis which are found in normal pancreatic tissue. Malignant transformation is rarely seen in heterotopic pancreas. Very few cases of adenocarcinoma resulting from heterotopic pancreas are reported in the literature [12,13]. The diagnosis of heterotopic pancreas is difficult due to various presentations, and there is no specific diagnostic method which is being worked on. The function of computed tomography and endoscopic ultrasound in this disease is rare. It is difficult to differentiate between this condition and other submucosal gastrointestinal tumors using these methods, and the evidence to confirm the diagnosis is usually histopathologic. In 1909, Heinrish histologically divided heterotopic pancreas into 3 types [14]: Type 1 indicates the existence of ductus, acini and islets of Langerhans (the most frequent type). Type 2 only indicates ductus and acini, while type 3 only indicates ductus. In the classification modified by Gasper later, type 1 indicates ductus, acini and islets of Langerhans similar to normal pancreas cells, and type 2 only indicates ductus, and type 3 only indicates acini, while type 4 only indicates islets [15]. In our case, the lesion fits into type 1 heterotopic pancreas.
As heterotopic pancreas tissue is asymptomatic, it does not have any clinical significance and does not require surgical treatment. However, where it is symptomatic or where a neoplastic condition cannot be eliminated in a radiologic and endoscopic method, surgical treatment is required [16]. Since it is macroscopically hard to distinguish it from malignancy, an extensive resection must be carried out to clear the surgical borders since it usually imitates a tumoral formation with its macroscopic view during explorations and palpation. Depending on the course of operation and the equipment of the hospital, the diagnosis is histologically performed through frozen section method or examination of the sent resection material by the pathologists.
Conclusion
Ectopic pancreas cases are rare. Inspite of being usually asymptomatic, its location particularly in stomach and duodenum may lead to some non-specific complaints. In such lesions found during laparotomy, the case requires excision even if it is not symptomatic. The definitive diagnosis can only be established through pathological examination.
References
- Armstrong CP, King PM, Dixon JM, Macleod IB. The clinical significance of heterotopic pancreas in the gastroin-testinal tract. Br J Surg. 1981;68:384-387.
- Tanaka K, Tsunodo T, Eto T, Yamada M, TajimaY, Shimogama H, et al. Diagnosis and management of heterotopic pancreas. Int Surg. 1993;78:32-35.
- Monig SP, Selzener M, Raab M, Eidt S. Heterotopic pancreas. A difficult diagnosis. Dig Dis Sci. 1996;41:1238-1240.
- Göksoy E, Perek S, Perek A, Oral C, Insel H. Kanamaya yolaçmis midede lokalize heterotopik pankreas olgulari. GATA Bülteni. 1985;27:771-775.
- Ueno S, Ishida H, Hayashi A, Kamagata S,Morikawa M. Heterotopic pancreas as a rare causeof gastrointestinal hemorrhage in the newborn:report of case. Surg Today. 1993;23:269-272.
- Hunt VC, Bonsteel HTS. Meckel’s diverticulum containing aberrant pancreas. Arch Surg. 1934;28:425-439.
- Klob L. Pancreas accesorium. Zeitschrift der Kaiserl. Konigl. Gesellschaft der Aerzte zu Wien. 1859;15:732.
- The Pediatric Clinics of North America. In: Emanuel Lebenthal editor: Pancreatic Diseasesin children Philadelphia: WB Saunders. 1996;pp.125-150.
- Mboti F, Maassarani F, De Keulencer R. Cholecysitis associated with heterotopic pancreas. Acta Chir Belg. 2003;103:110-112.
- Cankorkmaz L, Atalar MH, Müslehiddinoglu A, Dumlupinar Y, Köylüoglu G. Ektopik Pankreas Dokusunun Sebep Oldugu Bir Invajinasyon: Olgu Sunumu. C. Ü. Tip Fakültesi Dergisi. 2005;27:129-132.
- Huang YC, Chen HM, Jan YY, Huang TL, Chen MF. Ectopic pancreas with gastric outlet obstruction: report of two cases and literature review. Chang Gung Med J. 2002;25:485-490.
- Legel L, Louvel A, Chiche B, Michali P. Heterotopic pancreas. Report of 8 new cases. J Chir (Paris). 1979;116:553-560.
- Bini R, Voghera P, Tapparo A, Nunziata R, Demarchi A, Capocefalo M, Leli R. Malignant transformation of ectopic pancreatic cells in the duodenal wall. World J Gastroenterol. 2010;16:1293-1295.
- Von Heinrich H. Ein peitrang zur histrologie des sogen akzessorischen pancreas. Virchows Arch. 1909;198:392-401.
- Gaspar Fuentes A, Campos Tarrech JM, Fernandez Burgui JL, Castells Tejon E, Ruiz Rossello J, Gomez Perez J, et al. Pancreatic ectopias. Rev Esp Enferm Apar Dig. 1973;39:255-268.
- Haj M, Shiller M, Loberant N, Cohen I, Kerner H. Obstructing gastric heterotopic pancreas: case report and literature review. Clin Imaging. 2002;26:267-269.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
Mollaoglu MC, Soylu S, Bozkurt B, Egilmez HR, Turan MAn Unusual Cause of Acute Abdomen: Intestinal Ischemia due to Jejunal Heterotopic Pancreas.JCR 2015;5:128-131 |
|
Mollaoglu MC, Soylu S, Bozkurt B, Egilmez HR, Turan MAn Unusual Cause of Acute Abdomen: Intestinal Ischemia due to Jejunal Heterotopic Pancreas.JCR [serial online] 2015[cited 2026 Feb 3];5:128-131. Available from: http://www.casereports.in/articles/5/1/An-Unusual-Cause-of-Acute-Abdomen.html |

|
|
|
|
|