Introduction
Articular cartilage flap tear of patella is a rare injury seen in children. Osteochondral injuries of the patella following acute lateral patellar dislocation are common in the young, active population and exist in 40-95% of patellar dislocations. Patellar articular cartilage injuries can range from minor cartilaginous fissures to large, displaced osteochondral fractures. When significant fractures of the medial patellar articular surface are present, fracture fixation with open reduction and internal fixation or loose body fragment removal is indicated. The critical fragment size that mandates fixation has not been established, but fragments that are large enough to accept fixation hardware can presumably be fixed. Methods of fixation include headed and headless cannulated or solid screws composed of absorbable material or metal. An awareness of cartilage flap tear, together with its characteristic clinical and radiological features and proper treatment is necessary to avoid misdiagnosis and treatment delay.
Case Report
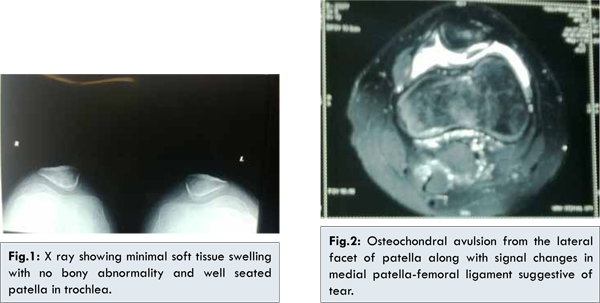
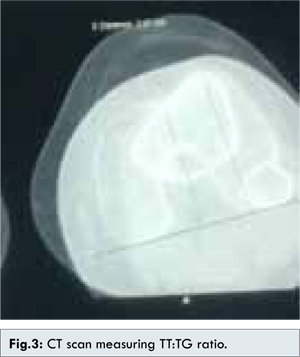
A 16 year old boy sustained twisting injury to left knee while playing basketball. He complained of patellar dislocation which got reduced by itself. He had long-standing knee pain, which got aggravated by injury. He underwent first aid in nearby hospital and came to us after 2 weeks of injury. On examination, there was mild knee swelling and retropatellar tenderness. On physical examination, there was an extension lag of 60°. The active range of motion of the injured knee was 60°-100° and passive range of motion was painful but not restricted. Radiographs of the injured knee showed soft tissue swelling as compared with the contralateral knee. No avulsed bony fragment was visible on the radiographs [Fig.1]. MRI showed cartilage defect with displaced and torn cartilage, focal denuding of articular surface suggestive of chondromalacia patella [Fig.2]. Computed tomography of the injured knee revealed a suspicious avulsed osteochondral fragment and TT:TG ratio of 2.21 (R-2.41), trochlear depth 0.45 (R-0.42), femoral neck anteversion-28° (R-19°), sulcus angle-137°(R-133°), trochlear inclination angle-23°(R-29°) [Fig.3]. There was no evidence of patella sleeve fracture or disruption in extensor mechanism.
Arthroscopy of left knee was done. Grade 4 (outer bridge classification) cartilage flap tear in center and grade 1 in periphery measuring 4×3 cm was noted from the lateral facet of patella [Fig.4]. Through mini-open medial parapatellar approach, microdrilling was done at the base of the lesion and fibrin glue was placed in the margins, stability was confirmed [Fig.5]. Closure was done in layers with double breasting of medial patellar retinaculumn. The wound healed well and no infection occurred. The patient started weight bearing on the operated leg protected with brace till 10 days after surgery. Three months after surgery, he attained right knee function with ROM of 0-120°. At the end of 1 year, he returned to pre-injury sporting activities.
Discussion
Fractures of the patella are relatively rare in children and adolescents with an estimated occurrence of 1% of all fractures in this age group [1]. Among these sleeve fractures of the patella are common and seen in children who have been taking part in activities requiring forceful extension of the knee with the quadriceps contracting against the resistance. Grogan et al. described four patterns of avulsion fractures namely superior, which is the least common; inferior, which is usually caused by an acute injury; medial, which accompanies an acute lateral dislocation of the patella and lateral, which is a chronic stress lesion resulting from repetitive tensile pull from vastus lateralis muscle [2]. Belman and neviaser noticed that the lack of diagnosis or a late diagnosis is common for patellar fractures in children [3].
X-ray studies of children’s knees are a challenge, even for the most experienced doctors. Most of the pediatric traumatologists must be aware of a child presenting an inconclusive X-ray imaging. Wessel et al. demonstrated that in 51 patients older than 14 years with acute knee trauma and hemarthrosis, a positive simple X ray image could only be seen in 16 of them. Thus, MRI is useful for diagnosing acute injuries. It can also be used to help on the diagnosis of patellar ligament ruptures and fractures in avulsion [4].
First time patellar dislocation commonly occurs in the young physically active population and is associated with a high rate of recurrent patellar instability. Depending on the patient cohort, 44-70% patients sustain recurrent dislocations [5]. With a complete dislocation of the patella, the primary stabilizer, the MPFL (medial patella femoral ligament) is frequently torn. A total or partial MPFL disruption can be observed by MRI [6].
A primary patellar dislocation quite often involves an osteochondral fracture that may require surgical fixation. The majority of primary dislocations can be managed non-surgically, although occasionally surgery is warranted and a thorough evaluation of each case is required [7]. In case of acutely and traumatically detached osteochondral fragments one should always attempt to reattach it in anatomically correct position. Newly detached OD fragments may be reattached with high success rate, especially in young patients. Anatomically correct refixation of osteochondral fragments with resorbable pins, screws, fibrin glue or by means of osteochondral plugs are the described method of fixation in the literature for osteochondral fragments. As given the literature, each technique has its own advantages and limitations.
Articular cartilage involvement can be considered an indication for surgery and cartilage defects should be repaired by reduction and fixation of the fragment. A fragment size more than 5×10 cm can be fixed and based on the experience of the authors, large fragments heal well if fixation is performed within 1 week of injury [7]. Fixation is performed with bioabsorbable nails, pins, small screws, or sutures. Small fractures can be arthroscopically removed if it acts as a loose body and produces symptoms [8].
Concerning the treatment options in this case, it was difficult to perform arthroscopic stabilization. We did a mini-open medial parapatellar approach, identified the cartilage flap tear and microdrilling was done at the base of the lesion. Stabilization of the fragment was done with the help of fibrin glue. Stability of the fragment was confirmed and double breasting of medial patellar retinaculumn was done.
By this technique, we are not doing transosseous drilling or fixation with implants, so that we can avoid patellar growth arrest and iatrogenic patellar fractures. Most of the literature says in-situ fixation with pins or screws is necessary for osteochondral fragment >1 cm and refixation techniques doesn’t have favourable result if fixation is done after 1 week of the injury. In our case, we have done stabilization with fibrin glue for an injury which was >2 weeks old with good outcome. Also, double breasting of medial patellar retinaculumn strengthens medial side structures of patella, thereby reducing the chances of recurrent dislocation of patella.
Conclusion
Patellar articular cartilage flap tear in children are uncommon. If so, they predominantly involve the cartilaginous portions of the patella. The fracture is easily missed by the emergency physicians, if no bony fragment avulsion is present on the X-ray film. An awareness of this type of injury with various surgical techniques is necessary for early diagnosis and appropriate surgical intervention.
References
- Dai LY, Zhang WM. Fractures of the patella in children. Knee Surg Sports Traumatol Arthros. 1999;7:243e5.
- Grogan DP, Carey TP, Leffers D, Ogden JA. Avulsion fractures of the patella. J Pediat Orthop. 1990;10:721e30
- Belman DAJ, Neviaser RJ. Transverse fracture of the patella in a child. J Trauma. 1973; 13:917-918.
- Wessel LM, Scholz S, Rusch M. Characteristic pattern and management of intra-articular knee lesions in different pediatric age groups. J Pediatr Orthop. 2001;21:14-19.
- Stefancin JJ, Parker RD. First-time traumatic patellar dislocation: a systematic review. Clin Orthop Relat Res. 2007;455:93-101.
- Elias DA, White LM, Fithian DC. Acute lateral patellar dislocation at MR imaging: injury patterns of medial patellar soft-tissue restraints and osteochondral injuries of the inferomedial patella. Radiology. 2002;225:736-743.
- Slabaugh M, Hess DJ, Bajaj S, et al. Management of chondral injuries associated with patellar instability. Oper Tech Sports Med. 2010;18:115-122.
- Mehta VM, Inoue M, Nomura E, Fithian DC. An algorithm guiding the evaluation and treatment of acute primary patellar dislocations. Sports Med Arthrosc. 2007;15:78-81.