Introduction
Acute laryngotracheobronchitis, an inflammatory disease involving the whole of tracheobronchial tree is a frequent disease in early childhood. Although it is usually self-limited, it may occasionally become life-threatening [1]. It can present as acute onset respiratory distress over two to three days with upper airway obstruction due to edema in the subglottic region which is the narrowest part of the upper airway. Systemic symptoms like malaise, high grade fever with cough are common and the child may be toxic.
Old unnoticed foreign body partially obstructing the upper airway may also present with classical symptoms of laryngotracheobronchitis and may confuse the clinicians in coming to proper diagnosis. Here we present a case of a 3 year old child who was initially diagnosed as laryngotracheobronchitis, but in due course of treatment a foreign body in the subglottic region was found. The case is unique because of the diagnostic dilemma between laryngotracheobronchitis and foreign body in larynx and also the unusual nature of the foreign body and its presentation.
Case Report
A 3 year old girl presented to the pediatric emergency with acute onset stridor for 1 day, cough and rise of surface temperature. At presentation, the patient was conscious, co-operative with surface temperature 102 F and 48/min respiratory rate. She had a shallow respiration with subcostal and intercostal suction and biphasic stridor, pulse 156/min, blood pressure 86/40 mmHg, no cyanosis and 88% SpO2. Bilateral chest auscultation showed coarse crepitations and decreased air entry on both sides. X-ray chest revealed no obvious abnormality. She was diagnosed to be a case of laryngotracheobronchitis and was treated by conservative management for around 8 hours with 100% oxygen through mask, intravenous antibiotics and steroids. In view of non-improvement of symptoms and steadily declining SpO2, otolaryngology opinion was sought for.
Considering the biphasic stridor and SpO2 of 60% at the time, emergency tracheostomy was done with 4 mm (ID) cuffed tracheostomy tube which immediately relieved the respiratory distress. Conservative management was continued for 4 days with strict monitoring of vitals. Blood reports showed: hemoglobin 13 gm%, total count 9800/cu. mm, with neutrophilia of 70%. Rest of the laboratory investigations including renal function tests, liver function tests, coagulation profile revealed no abnormality. As the respiratory distress and stridor was completely relieved after tracheostomy, the need for upper airway examination by bronchoscopy was taken into account. So, following all investigations, a check bronchoscopy was planned under general anaesthesia to examine the upper airway above the tracheostomy.
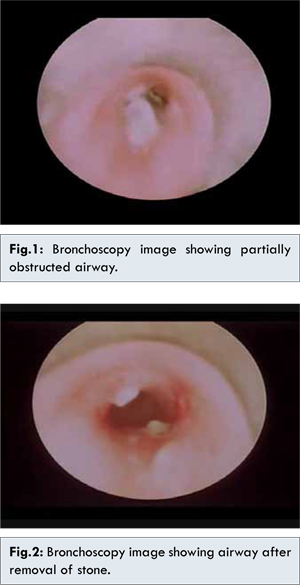
On bronchoscopy on the fifth day after admission, a sloughy mass was found to be impacted in the subglottic region with local edema partially obstructing the airway [Fig.1]. On suction over the mass a black colored stone was identified and removed in the same sitting [Fig. 2] and the tracheostomy was maintained with uncuffed tracheostomy tube to allow for the edema to settle. The patient was kept on intravenous steroids and antibiotics for seven days and oral diet was allowed. After 7 days repeat bronchoscopy was performed and whole of the upper airway was found to become normal. Gradual decannulation of the tracheostomy was performed over one week and the recovery of the patient following decannulation was uneventful. The patient was discharged after another three days with oral medications.
On follow-up after two weeks, the patient had no further complains and was leading a normal life. However the patient was followed up for 2 months post-operatively without any significant morbidity.
Discussion
The foreign bodies in the throat pose a variety of challenge to the otorhinolaryngologists. Among them foreign body in the respiratory tract is unique because of its life threatening ability and difficulty in diagnosis. Classical history of choking and coughing is not available in most of the cases, especially in children thereby delaying and misleading the diagnosis. The diagnosis and treatment of the problem requires highest degree of suspicion of signs and symptoms of foreign body aspiration [2]. Irregular foreign bodies or orientation in the sagittal plane may produce only partial obstruction allowing adequate air movement around the obstruction [3]. This can lead to definite difficulty in diagnosis in these patients. A long standing foreign body may cause local inflammation and subsequent infection leading to systemic signs and symptoms of toxicity in the patients. Some symptoms may mimic croup, misdiagnosing the case to be laryngotracheobronchitis and subsequent delayed or wrong treatment leading to catastrophe.
Majority of the children presenting with foreign body aspiration are under the age of 3 years [4]. Foreign body in the respiratory tract presents with classical symptoms of acute onset respiratory distress with history of something kept in mouth with sudden development of choking and cough. Tracheostomy is occasionally indicated in foreign body extraction, when they are subglottic in location [5]. Usually there is no history of fever in these cases while laryngotracheobronchitis presents with history of respiratory distress and high grade fever. But in this particular case, the patient presented with respiratory distress and fever, probably due to foreign body reaction and secondary infection which mislead the pediatricians in diagnosis of laryngotracheobronchitis. But the diagnosis was put to question when blood reports were normal and loading dose of steroid could not relieve the symptoms. Another point of concern was that no foreign body was seen in the trachea when tracheostomy was being performed. However, confirmative diagnosis could only be made when the foreign body was seen on diagnostic bronchoscopy. So if decannulation of tracheostomy tube had been done without bronchoscopic evaluation respiratory distress would once again set in.
The patients presenting with features of laryngotracheobronchitis and not improving with conservative treatment should be further evaluated for a foreign body in the airway, even in absence of classical history of foreign body aspiration.
Conclusion
Pediatric stridor simulating laryngotracheobronchitis is thus a real challenge to the clinicians and upper airway foreign bodies may be the possible cause even without typical history of foreign body or food ingestion requiring urgent tracheostomy and mandatory diagnostic bronchoscopy for upper airway examination.
References
- Petrocheilou A, Tanou K, Kalampouka E, Malakasioti G, Giannios C, Kaditis AG. Viral croup: diagnosis and a treatment algorithm: Pediatr Pulmonol. 2014;49(5):421-429.
- Kalyanappagol VT, Kulkarni NH, Bidri LH. Management of tracheobronchial foreign body aspirations in pediatric age group: A 10 year retrospective analysis. Indian Journal of Anaesthesia. 2007;51(1):20-23.
- Ghai A, Wadhera R, Hooda S, Kamal K, Verma V: Subglottic foreign bodies- Two Case Reports: Anaesth, Pain & Intensive care. 2008;12(1):27-29.
- Siddiqui MA, Banjar AH, Al-Najjar SM, et al. Frequency of tracheobronchial foreign body in children and adolescents. Saudi Med J. 2000; 21:368-371.
- Singh JK, Vasudevan V, Bharadwaj N, Narasimhan KL. Role of tracheostomy in the management of foreign body airway obstruction in children: Singapore Med J. 2009; 50(9):871-874.