|
|
|
|
|
Extracutaneous Juvenile Xanthogranuloma in an Infant Presenting as a Renal Mass
|
|
|
Payam Ahmedmaulid1, Fatma Betul Cakir2, Feryal Gun3, Eyup Kaya4, Yasemin Ozluk1, Nesimi Buyukbabani1, Isin Kilicaslan1
Department of 1Pathology and 3Pediatric Surgery, Istanbul University, Istanbul Faculty of Medicine, Turkey. 2Department of Pediatrics, Division of Pediatric Hematology-Oncology, Bezm-i Alem Vakif University, Turkey. 4Department of Radiology, Bakirkoy Dr. Sadi Konuk Training and Research Hospital, Turkey. |
|
|
|
|
|
Corresponding Author:
|
Dr. Payam Ahmedmaulid
Email: upmaulid@gmail.com
|
|
|
|
|
|
|
|
|
Received:
19-NOV-2014 |
Accepted:
26-FEB-2015 |
Published Online:
20-MAR-2015 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
Juvenile xanthogranuloma (JXG) is a benign proliferative disorder of dermal dendrocytes which usually presents with skin lesions. Renal involvement is extremely rare. We present a 40 day old female infant. Radiologic imaging techniques revealed a renal mass, prompting a preliminary diagnosis of a renal tumor. Consequently, nephrectomy and histopathological examinations were performed yielding a diagnosis of “JXG”. The patient did not exhibit any pathognomonic skin lesions. This case is unique with its unusual clinical presentation. Although renal involvement of JXG is very rare, it should be kept in mind in clinical differential diagnosis in infants and children presenting with renal mass. |
|
|
|
|
|
Keywords :
|
Juvenile Xanthogranuloma, Kidney Neoplasms, Histiocytosis, Nephrectomy, Kidney, Humans.
|
|
|
|
|
|
|
|
|
|
|
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ffa017060000009403000001001500 6go6ckt5b5idvals|441 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
Juvenile xanthogranuloma is the most common non-Langerhans cell histiocytosis [1]. The etiology is unknown [2]. It is typically seen early in childhood and usually presents as a yellowish-red papule on the skin of the head, neck and upper abdomen [2]. Systemic involvement is rare. In a large case study series with systemic involvement, solitary skin lesions accounted for 67%, multiple skin lesions 7%, superficial and deep soft tissue lesions 16%, and skin lesions with or without systemic involvement 5% of all patients [3]. Cases with renal involvement are very rare [3-6].
Case Report
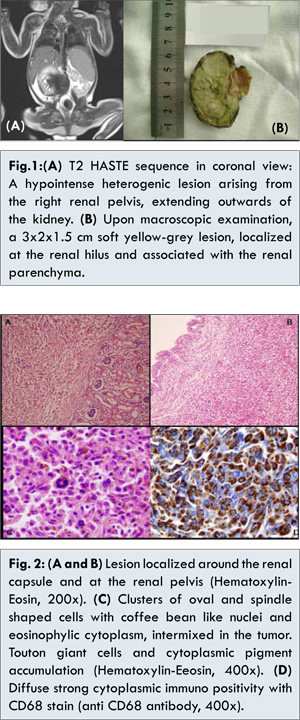
A 40 day-old preterm infant presented at the pediatric clinic with jaundice, abdominal distention and respiratory distress. Investigations revealed pancytopenia, hypoproteinemia, hypoalbuminemia, direct hyperbilirubinemia, elevated hepatic enzymes, prolonged prothrombin time and elevated INR values. Ultrasonographic examinations revealed a double collecting system variation in the right kidney, along with an increase of echogenicity in the parenchyme and perirenal areas. A 44x34x23 mm hypoechoic, heterogenic solid mass lesion with prominent vascularization was determined extending from the pelvis medially and out of the kidney, compressing the renal vein, causing obliteration and dilatation of the abdominal aorta and resulting in expansion of the upper pelvicalyceal structures. Abdominal MR showed a slightly contrast enhanced mass lesion, heterogenously iso-hypointense on T1 weighted series, and heterogeneously hypointense on T2 weighted series, originating from the right renal pelvis, and extending peripherally [Fig.1A].
Because the patient had pancytopenia, hemophagocytosis and lymphoproliferative disease with renal involvement were included in the differential diagnosis and a bone marrow aspiration was performed. The aspiration material did not contain blastic cells or hemophagocytosis. Due to deterioration of the clinical condition of the patient, a laparoscopic nephrectomy was performed. Examination of the nephrectomy material showed a soft, yellow-grey 3x2x1.5 cm lesion, located at the hilus, in connection with the parenchyme [Fig.1B]. Histopathological examination revealed a pelvic mass with distinct borders, surrounding the normal hilar structures [Fig.2A,2B]. The lesion contained clusters of oval and spindle shaped cells with eosinophylic cytoplasm and fine chromatin nuclei reminiscent of coffee beans. Additionally Touton type giant cells with abundant cytoplasm were identified in some areas, especially in the periphery of the lesion. Pigment accumulation in the cytoplasm of some cells was striking [Fig.2C]. The Prussian blue stain revealed the pigment to be hemosiderin. Immunohistochemistry was performed and diffuse, strong immunopositivity was obtained with antibodies CD68 (KP1, Thermo, USA), CD163 (10D6, Thermo, USA), and Factor XIIIa (AC-1A1, Thermo, USA), while S100 (4C4.9, Thermo, USA), Langerin (12D6, Novocastra, United Kingdom) and CD1a (MTB1, Novocastra, United Kingdom) were found to be negative [Fig.2D]. Histomorphological and immunhistochemical findings revealed a diagnosis of a “juvenile xanthogranuloma”.
After the nephrectomy, the patient`s clinical condition deteriorated due to hepatic failure. Consequently, systemic chemotherapy was administered. The patient expired 12 days after the operation due to multiorgan failure and/or sepsis.
Discussion
We present a systemic case of juvenile xanthogranuloma demonstrating typical histomorphological findings. In juvenile xanthogranuloma, in early lesions, vacuolated cells without prominent lipid accumulation are seen. Mature lesions exhibit a granulomatous infiltrate composed of foam cells, foreign body and Touton type giant cells [7]. To confirm our diagnosis, we applied immunohistochemistry and received a diffuse, strong positive reaction with antibodies CD68, CD163 and Factor XIIIa, while a negative reaction was obtained with Langerhans cell markers, such as S100, CD1a and Langerin.
Juvenile xanthogranuloma is the most common non-Langerhans cell histiocytosis [1]. It is typically seen in early childhood. It is a benign and self limited disease which usually presents with a yellowish-red papule on the skin of the head, neck and upper abdomen. Systemic involvement is rare. In previously published case reports, single or multiple organ involvement of the ocular, hepatic, intestinal, cardiac, bone marrow, pulmonary, splenic, central and peripheric nervous system has been reported [3,8,9,10]. Cases with renal involvement are very rare [3-6]. No correlation has been established between juvenile xanthogranuloma and the presence or absence of cutaneous lesions [1]. While surgical resection is curative in symptomatic systemic cases which are eligible for surgery, post surgical recurrence has been reported [1]. Lesions that cannot be resected are treated with a Langerhans cell histocytosis based chemotherapy, radiotherapy, or a combination of both [1]. Survival rates in a large case series for systemic juvenile xanthogranuloma patients were reported as being between 50% and 100% [1,11]. Systemic juvenile xanthogranuloma may follow a fatal course. In our case, the patient expired due to multiorgan failure and/or sepsis, in spite of chemotherapy, wide spectrum antibiotics and palliative support.
Juvenile xanthogranuloma is essentially a benign disorder limited to the skin therefore in the presence of the classic cutaneous lesions, radiological screening for probable visceral organ involvement is not recommended. However the mass effect of systemic lesions may cause morbidity and mortality [12]. As illustrated by the case report published by Matcham et al. [12], where there is abdominal wall muscle and pulmonary involvement, juvenile xanthogranuloma can be confused with a tumor. This may lead to difficulties in establishing a radiological or clinical diagnosis.
Our patient was a preterm infant that presented at a very early stage of life with jaundice, abdominal distention and respiratory distress. The radiological findings of the patient mimicked a renal tumor. If we take into consideration that the clinical presentation of our case was a renal tumor, it would be beneficial for clinicians and radiologists to bear in mind that juvenile xanthogranuloma, which is a rare disorder, can mimic malignancy in various organs.
References
- Sivapirabu G, Sugo E, Wargon O. Juvenile xanthogranuloma: Challenges in complicated cases. Australas J Dermatol. 2011;52:284-287.
- Juvenile Xanthogranuloma. In: Elder DE, Elenitsas E, Johnson, Jr BL, Murphy GF, eds. Lever Histopathology of the Skin, 9th ed. Lippincott Williams and Wilkins, Philadelphia, 2005: 672-673.
- Janssen D, Harms D. Juvenile xanthogranuloma in childhood and adolescence: A clinicopathologic study of 129 patients from the Kiel pediatric tumor registry. Am J Surg Pathol. 2005;29:21-28.
- Dehner LP. Juvenile xanthogranulomas in the first two decades of life: a clinicopathologic study of 174 cases with cutaneous and extracutaneous manifestations. Am J Surg Pathol. 2003;27:579-593.
- Kolivras A, Theunis A, de Saint-Aubain N, Zelger B, Sass U, Dangoisse C, et al. Congenital disseminated juvenile xanthogranuloma with unusual skin presentation and renal involvement. J Cutan Pathol. 2009;36:684-688.
- Patel P, Vyas R, Blickman J, Katzman P. Multi-modality imaging findings of disseminated juvenile xanthogranuloma with renal involvement in an infant. Pediatr Radiol. 2010; 40 (Suppl 1):6-10.
- Dehner LP. Juvenile xanthogranulomas in the first two decades of life: a clinicopathologic study of 174 cases with cutaneous and extracutaneous manifestations. Am J Surg Pathol. 2003; 27:579-593.
- Azorin D, Torrelo A, Lassaletta A, de Prada I, Colmenero I, Contra T, et al. Systemic juvenile xanthogranuloma with fatal outcome. Pediatr Dermatol. 2009;26:709-712.
- George DH, Scheithauer BW, Hilton DL, Fakhouri AJ, Kraus EW. Juvenile xanthogranuloma of peripheral nerve: a report of two cases. Am J Surg Pathol. 2001;25:521-526.
- Liang S, Liu YH, Fang K. Juvenile xanthogranuloma with ocular involvement. Pediatr Dermatol. 2009;26:232-234.
- Isaacs H Jr. Fetal and neonatal histiocytoses. Pediatr Blood Cancer. 2006;47:123-129.
- Matcham NJ, Andronikou S, Sibson K, et al. Systemic juvenile xanthogranulomatosis imitating a malignant abdominal wall tumor with lung metastases. J Pediatr Hematol Oncol. 2007;29:72-73.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
Ahmedmaulid P, Cakir FB, Gun F, Kaya E, Ozluk Y, Buyukbabani N, Kilicaslan IExtracutaneous Juvenile Xanthogranuloma in an Infant Presenting as a Renal Mass.JCR 2015;5:124-127 |
|
Ahmedmaulid P, Cakir FB, Gun F, Kaya E, Ozluk Y, Buyukbabani N, Kilicaslan IExtracutaneous Juvenile Xanthogranuloma in an Infant Presenting as a Renal Mass.JCR [serial online] 2015[cited 2025 Jul 10];5:124-127. Available from: http://www.casereports.in/articles/5/1/Extracutaneous-Juvenile-Xanthogranulomain-an-Infant-Presenting-as-a-Renal-Mass.html |

|
|
|
|
|