|
|
|
|
|
Hepatopulmonary Syndrome as the First Manifestation of Wilson Disease
|
|
|
lexapro and pregnancy test lexapro and pregnancy
From the Department of General Medicine, IPGMER and SSKM Hospital, Kolkata-700020, India. |
|
|
|
|
|
Corresponding Author:
|
Dr. Durjoy Lahiri
Email: durjoy21288@ymail.com
|
|
|
|
|
|
|
|
|
Received:
03-NOV-2014 |
Accepted:
09-JAN-2015 |
Published Online:
30-JAN-2015 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
Wilson’s disease is considered among the rare etiologies of chronic liver disease. The spectrum of clinical presentation of Wilson disease is broad, the most frequent ones being liver disease and neuro-psychiatric symptoms. An unusual complication of hepatic failure is hepato-pulmonary syndrome, which manifests as dyspnoea and central cyanosis. Wilson disease presenting for the first time as central cyanosis and clubbing is uncommon, which makes this case a reportable one. Here, we report the case of a 20 year old Asian female patient presenting with central cyanosis and clubbing. Clinical examination revealed polycythemia, hypoxemia with orthodeoxia and splenomegaly. No intrinsic cardio-pulmonary disease could be elicited. Bubble contrast echocardiography and X-ray pulmonary angiography revealed the presence of pulmonary arterio-venous fistula. Portal hypertension was detected on ultrasound Doppler of portal vein and endoscopic evidence of large oesophageal varices. Imaging evidence of hepatic fibrosis prompted work up for liver disease. Existence of Kayser-Fleisher ring on slit lamp examination of eyes, reduced serum ceruloplasmin and very high levels of 24 hour urinary copper excretion concluded the diagnosis as Wilson disease and her central cyanosis was attributed to hepato-pulmonary syndrome. This case highlights an unusual presentation of Wilson disease. At the same time, it emphasizes the fact that hepato-pulmonary syndrome may occur without florid clinical manifestation of liver failure and hence needs to be considered in the differential of central cyanosis. |
|
|
|
|
|
Keywords :
|
Hepatopulmonary syndrome, Copper, Cyanosis, Liver Failure, Liver Diseases, Dyspnea, Humans.
|
|
|
|
|
|
|
|
|
|
|
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ffec07060000006003000001000200 6go6ckt5b5idvals|421 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
Liver diseases are not considered high in the list of possibilities while dealing a case of cyanosis and clubbing, particularly if the patient presents for the first time with these features. Chronic liver disease may pave the way for hypoxia due to multiple reasons. Hepatopulmonary syndrome is an entity which is sometimes held responsible for hypoxia in hepatic failure patients. The triad of liver disease, hypoxemia, and intrapulmonary vascular dilatations is typical of HPS [1]. Microvascular alterations and dilatations in the pre-capillary and capillary pulmonary arterial circulation remain the underlying mechanism [2]. Regardless of the etiology of liver disease, patients of HPS present most commonly with respiratory complains. Occasionally, HPS may be the presenting feature of liver disease in some patients. Hence one should remain alert to the possibility of HPS while approaching a case of cyanosis.
Wilson disease, a rare autosomal recessive disorder of copper metabolism presents most frequently with hepatic disease or neuropsychiatric manifestations [3]. Cirrhosis with portal hypertension is not uncommon if we consider the spectrum of liver dysfunction in Wilson disease. As in other liver diseases, HPS has been reported to occur in Wilson disease also [4]. But HPS as the first manifestation of Wilson disease is very unusual. Here, we report the case of a 20 year old female patient presenting with cyanosis and clubbing, who was subsequently diagnosed to have HPS and the underlying etiology of hepatic dysfunction was proved to be Wilson disease.
Case Report
A 20 year old Asian female patient presented with bluish discolouration of lips, fingers and toes for the preceding 6 months along with simultaneous swelling of the terminal part of her fingers and toes. Both the symptoms were progressive over the mentioned duration. Recently, she was experiencing easy fatigability for around 1 month, without any dyspnoea, palpitation, pedal swelling, abdominal distension and chest heaviness. She denied any history of recurrent chest infections in childhood or any history suggestive of cyanotic spells at her school going age. No significant family history was obtained.
On examination, she was found to have central cyanosis [Fig.1], clubbing of all the fingers and toes [Fig.2] and polycythemia. Her pulse rate was 84/min and blood pressure was 110/70 mm Hg. There was no detectable abnormality in her pulse and blood pressure. Pulse oximetry suggested hypoxemia as her SpO2 reading was 86% (in room air and supine posture), which reduced to 80% on upright posture, which was favouring orthodeoxia. Thorough examination of cardiovascular system and respiratory system did not reveal any abnormality. Abdominal examination revealed the presence of splenomegaly which was approximately 5 cm below the left costal margin along the splenic axis and firm in consistency. There was no abdominal distension or prominence of superficial veins. Other system examinations were non-contributory.
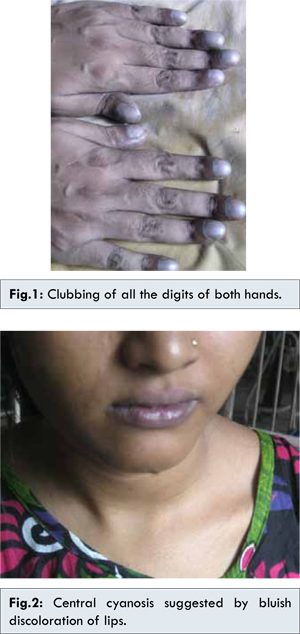
Complete haemogram showed Hb: 18 gm% and haematocrit 62. Chest X-ray showed the presence multiple small dense shadows in both lung fields, involving mid and lower zones [Fig. 3]. ECG had no abnormality except sinus tachycardia. Echocardiography was performed based on the strong suspicion of congenital heart disease. There was no evidence of any congenital defect in heart. Bubble contrast echocardiography was contributory as it detected the presence of contrast in left heart in 3-4 cycles which suggested the presence of pulmonary arterio-venous communication. X ray pulmonary angiography was done, which confirmed the presence of pulmonary arterio-venous fistulae in mid and lower zones of both lungs [Fig. 4]. These were consistent with the clinical findings consisting of central cyanosis, clubbing and hypoxemia with orthodeoxia.
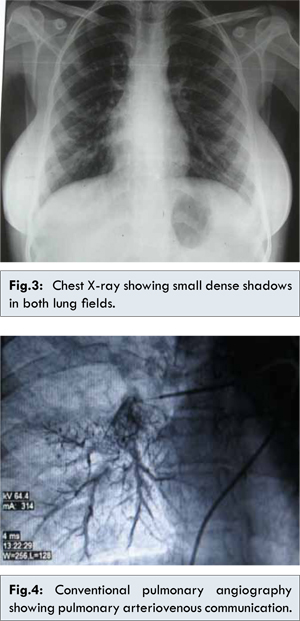
For addressing the issue of splenomegaly, imaging work up was carried out. USG revealed the presence of splenomegaly, hepatomegaly with altered echotexture and portal hypertension (PV diameter 14 mm). On Doppler study, there was no obstruction in splenic vein, portal vein and inferior vena cava. Upper GI endoscopy showed the existence of large oesophageal varices. At this point, we reviewed her clinical history but nothing suggestive of liver disease or upper GI haemorrhage was obtained. She never underwent any abdominal operation and denied any addiction. Now investigation was directed towards finding the etiology of portal hypertension. LFT revealed hypoalbuminemia (serum albumin 2.3 gm/dL) and no other abnormality. Fibroscan of liver was suggestive of grade 3 fibrosis. She was negative for the Hepatitis B, Hepatitis C markers and autoimmune panel. Slit lamp examination was positive for the presence of KF ring in both the eyes. Her serum ceruloplasmin level was 19 mg/dL (normal 25-45 mg/dL) according to turbidometric method and 24 hour urinary copper excretion turned out to be 900 micrograms. She was thus diagnosed to be a case of Wilson disease based on AASLD (American Association for the Study of Liver Diseases) practice guidelines 2008 [5]. The presenting complain of this patient was attributed to HPS developing as a complication of her liver disease.
Discussion
Wilson disease is an autosomal recessive disorder of systemic copper overload and resultant toxicity. Mutations in the ATP7B gene that encodes for a membrane-bound copper transporting ATPase result in impaired biliary excretion of copper, positive copper balance, hepatic copper accumulation, and copper toxicity from oxidative damage [6]. Symptomatic Wilson disease, most commonly, presents as hepatic disease or neuropsychiatric manifestations. Other organs which may be involved, though uncommonly, are kidney, heart and skeletal system [3]. Among the hepatic presentations of Wilson disease, cirrhosis of liver is an important member, consisting of features of hepatocellular failure such as jaundice, ascites, oedema and in extreme cases, encephalopathy. The clinical course of hepatic cirrhosis is complicated by a number of complications and portal hypertension is a significant among them.
There are various reasons of dyspnoea and central cyanosis in a subject with chronic liver disease. Intrinsic cardiopulmonary diseases unrelated to liver disease constitute the major group. Complications of cirrhosis and some uncommon underlying etiologies of liver disease constitute another group. In a subset of patients, two uncommon complications of cirrhosis are observed as the cause pulmonary dysfunction. These are HPS and portopulmonary hypertension [3].
HPS is typically diagnosed in the background of cirrhosis of liver and portal hypertension. However, cases of HPS have been reported in patients with portal hypertension without cirrhosis and in patients with liver dysfunction without established portal hypertension [3]. Association between HPS and severity of liver has not yet been clearly established [3]. The major cause of hypoxemia in HPS is thought to be due to intrapulmonary vascular abnormalities resulting from following factors: first, raised levels of ET-1 circulating in whole body [7]; second, few hepatic products required for pulmonary vasomotor control are decreased by liver disease or low hepatic venous flow [8,9]; third, translocation gut bacteria causing accumulation and activation of macrophages in the lungs with consequent rise in inducible NO synthase production and vasodilatation [10].
Dyspnoea is the most common symptom of HPS. Platypnoea and orthodeoxia, representing shortness of breath and oxygen desaturation respectively on assuming the sitting position are typical clinical features supporting HPS. Additional clinical features consist of clubbing, cyanosis, and the presence of cutaneous spider nevi. Spider nevi may bear special significance in HPS as they may be a marker of intrapulmonary vascular dilatations. In the case described above, the patient presented with features suggestive of hypoxia and did not have any clinical feature suggesting liver dysfunction. The only available clue was orthodeoxia and splenomegaly which prompted the evaluation for HPS and portal hypertension respectively. The underlying cause of portal hypertension turned out to be cirrhosis of liver resulting from Wilson disease in this case. The uniqueness of the case was that the patient presented to the medical facility for the first time with features favouring hypoxia and was ultimately diagnosed to be a case of cirrhosis of liver with a pulmonary vascular complication, namely HPS. Besides highlighting an unusual presenting feature of Wilson disease, this case draws our attention to the fact that HPS should be considered in the differential list of central cyanosis even in absence of clinical features of liver disease.
Conclusion
This case describes an unusual presentation of Wilson disease and thus adds to the wide spectrum of clinical presentation of this disease. It also highlights the fact that considering HPS in the differential diagnosis of patients presenting with central cyanosis cannot be overemphasized.
References
- Aboussouan LS, Stoller JK. The hepatopulmonary syndrome. Baillieres Best Pract Res Clin Gastroenterol. 2000;14(6):1033-1048.
- Moises Ilan Nevah, Michael B. Fallon. Hepatic Encephalopathy, Hepatorenal Syndrome, Hepatopulmonary Syndrome, and Systemic Complications of Liver Disease. In: Mark Feldman, Lawrence S. Friedman, Lawrence J. Brandt, editors. Sleisenger and Fordtran’s Gastrointestinal and Liver Disease, 9th ed. 2010. p: 1549-1555.
- Kochar R, Fallon MB. Pulmonary Manifestations of Liver Disease. In: Eugene R. Schiff, Willis C. Maddrey, Michael F. Sorrell,editors. Schiff’s Diseases of Liver, 11th ed.2012. pp: 381-383.
- Almohana S. Prevalence of clinically significant Hepatopulmonary Syndrome among Patients with Chronic Liver Disease and Portal Hypertension. Al-Kindy Col Med J. 2011;7(1):61-66.
- Eve A. Roberts, Michael L. Schilsky. Diagnosis and Treatment of Wilson Disease; An Update. Hepatology. 2008;47(6):2089-2111.
- George J. Brewer. Wilson’s Disease. In: Dan L. Longo, Dennis L. Kasper, J. Larry Jameson, Anthony S. Fauci, Stephen L. Hauser, Joseph Loscalzo, editors. Harrison’s Principles of Internal Medicine, 18th ed.2012.pp: 3188-3190.
- Asbert M, Gines A, Gines P, Jimenez W, Claria J, Salo J, et al. Circulating levels of endothelin in cirrhosis. Gastroenterology. 1993;104(5):1485-1491.
- Srivastava D, Preminger T, Lock JE, Mandell V, Keane JF, Mayer JE Jr, et al. Hepatic venous blood and the development of pulmonary arteriovenous malformations in congenital heart disease. Circulation. 1995;92(5):1217-1222.
- Shah MJ, Rychik J, Fogel MA, Murphy JD, Jacobs ML. Pulmonary AV malformations after superior cavopulmonary connection: resolution after inclusion of hepatic veins in the pulmonary circulation. Annals of Thoracic Surgery. 1997;63(4):960-963.
- Rabiller A, Nunes H, Lebrec D, et al. Prevention of Gram negative translocation reduces the severity of hepatopulmonary syndrome. American Journal of Respiratory and Critical Care Medicine. 2002;166(4):514-517.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
Lahiri D, Agarwal R, Mondal D, Roy MK, Sarkar N, Mukhopadhyay JHepatopulmonary Syndrome as the First Manifestation of Wilson Disease.JCR 2015;5:37-41 |
|
Lahiri D, Agarwal R, Mondal D, Roy MK, Sarkar N, Mukhopadhyay JHepatopulmonary Syndrome as the First Manifestation of Wilson Disease.JCR [serial online] 2015[cited 2025 Dec 15];5:37-41. Available from: http://www.casereports.in/articles/5/1/Hepatopulmonary-Syndrome-as-the-First-Manifestation-of-Wilson-Disease.html |

|
|
|
|
|