Introduction
Gall stone disease is a common disease in the Western world with prevalance of arround 10% in the general population [1]. Gallbladder fistulation into other hollow organs may complicate gall stone disease leading to cholecystocholedochal/ cholecystogastric/ cholecystoduodenal or cholecysto-enteric with consequent common bile duct, duodenal/ pyloroduodenal or small bowel obstruction. The management depends on the type of complication and patient’s clinical condition and we have suggested a management flow chart to aid selection of therapy based on the size and site of the stone.
Methods:
PICOS (Population, Intervention, Comparatives, Outcomes, Study designs) were employed in developing the search strategy including Medline 1946 to May 2013 and Embase from 1947 to May 2013 using Ovid Interface relating to human studies. We used the following MESH (medical subject headings) terms: Bouveret’s syndrome, intestinal obstruction and duodenal gall stones. Papers relating to Bouveret’s syndrome presenting with duodenal obstruction were retrieved using Boolean terms ‘AND’, ‘OR’ with construction of filters.
Clinical Presentation
Cholelithiasis is a relatively common health problem; by age 75, about 35% of women and 20% of men have developed gallstones [2]. While the majority of patients with gallstones do well, a small percentage of patients (approximately 6%) develop complications including cholecystoduodenal fistulas leading to Bouveret’s syndrome (BS). Nausea, vomiting, fever, pain, obstructive jaundice on the background of long standing symptomatic gallstones are common presentation features of BS. A large (> 2 cm in diameter) fistulating stone into the duodenum is a common underlying cause [3].
Bouveret’s syndrome usually affects elderly women with a history of gallstones [4] and presents with intermittent attacks of abdominal pain and frequent vomiting consistent with gastric outlet obstruction, occurring over several days. There may or may not be a history suggestive of recent acute cholecystitis. The patient is often elderly and may be significantly dehydrated with electrolyte imbalance by the time they present. The syndrome is associated with a high degree of morbidity and mortality (up to 30%), which is attributed to delays in relieving the obstruction and co-existing medical illness [5].
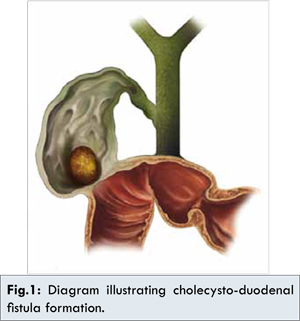
Fistula formation is a feature of a long-standing calculus biliary tract disease; approximately 0.5% of all patients undergoing therapy for chronic gallbladder disease will have fistula. The fistulae have been described to have occurred with virtually every conceivable structure and thought to occur as a result of adhesions between the gallbladder and the bowel wall from chronic inflammation associated with impaired arterial blood supply and decreased venous drainage leading to pressure necrosis.
An inflamed gallbladder may adhere to and perforate the gastrointestinal tract resulting in the formation of a cholecysto-enteric fistula. This may allow resolution of cholecystitis by decompression of the gallbladder but may give rise to gastrointestinal tract obstruction. In the majority (85%) of cases of biliary-enteric fistula the stone passes spontaneously [6]. However, 15% of patients develop clinical features of bowel obstruction [5]. The most common sites for impaction of the gallstone is the terminal ileum (90%) but other sites, in order of decreasing frequency, are the proximal ileum, distal jejunum, colon, duodenum and stomach [5,7].
Investigations
Initial laboratory investigations may reveal a high haematocrit secondary to dehydration and electrolyte imbalance, typically with hypokalemic hypochloraemic metabolic alkalosis. Plain abdominal radiographs may demonstrate pneumobilia (air in the biliary tree), gastric distension and calcified gallstones in unusual sites. Serial radiographs may show a change in the position of the gallstone reflecting its passage through the fistula and gastrointestinal tract.
The triad of stomach distension along with imaging confirmation of a stone in the duodenum and air in the right upper quadrant is diagnostic of Bouveret’s syndrome and occurs in a third of cases [8]. Gallstones giving rise to gastric outlet obstruction may also be diagnosed at endoscopy where a dilated stomach and hard mass at the site of the obstruction may be found [7].
Mixed Gallstones
It has been postulated that calcium precipitation in bile is a critical event in cholelithiasis [9]. Copper and iron may act as chelating agents for calcium bilirubinate. The central aggregates of calcium salts constitute hard foreign bodies which may lead to ulceration of gallbladder mucosa and microscopic haemorrhage. The iron released by this process may be another source of its deposition in gallstones. Injury to gallbladder mucosa also provides an opportunity for release of epithelium. Beta-glucorunidase, an additional enzyme contributes towards precipitation of calcium bilirubinate [10]. Been et al. [11] reported the presence of small amount of iron in a thick black shell around the central dark inclusion of gallstones. The high iron content in mixed gallstones might be promoting aggregation of calcium bilirubinate particles which are the major constituents especially due to the polyelectrolytic nature of iron. All these theories proposed by various authors will explain the formation of large gall stones which are the potential root cause for Bouveret’s syndrome.
Management of Bouveret’s Syndrome
Halasz et al. in 1964 [12] suggested removal of the stone through gastrostomy or enterolithotomy and then cholecystostomy for removal of stones from the gall bladder; and that definitive closure of the fistula and cholecystectomy are best left for a later time. Warshaw et al. in 1966 [13] however suggested that cholecystostomy is inferior to cholecystectomy for relief of symptoms because of residual diseased gall bladder. Warshaw recommended cholecystectomy and closure of the fistula at later time in patients with residual symptoms or demonstrable biliary stones, and should be considered in those with persistent cholecystoenteric fistula. Mohammad et al. 2002 [14] reported small bowel obstruction following the use of Holmium:YAG laser necessitating urgent enterolithotomy. Laser or shock wave lithotripsy might actually lead to various other complications worsening the existing situation.
As with all cases of obstruction, the initial management is resuscitation of the patient who may be critically dehydrated. Nasogastric suction is initiated and fluid and electrolyte imbalance rapidly corrected. Once the site of the obstructing stone is identified, removal of the stone can be carried out either endoscopically or surgically.
Endoscopic Retrieval
Smaller stones located in the stomach and proximal duodenum may be amenable to endoscopic retrieval, especially in patients with higher surgical risk. Options for endoscopic management include endoscopic lithotomy using foreign body forceps or Dormia basket, mechanical fragmentation, endoscopic or percutaneous laser lithotripsy or extra-corporeal shock wave lithotripsy. Advantages of endoscopic management include the fact that it may be more suitable in elderly patients and those with co-morbidities as well as the fact it avoids enterotomy in a duodenum, which may be ulcerated and friable as a consequence of stone impaction.
Fragmentation of the stone by lithotripsy or dislodgement during attempts to remove it endoscopically with its subsequent impaction downstream may result in small bowel obstruction necessitating enterolithotomy [15]. In addition, several attempts at endoscopic lithotripsy may be required before complete fragmentation of the stone is achieved, resulting in repeat endoscopies and a long overall treatment time. Furthermore, the use of endoscopic intervention may be limited by the location of the stone in the distal duodenum, which may make it inaccessible to the endoscope, particularly in the presence of gross gastric distension.
Surgical Therapy
A large stone may be larger than the gastro-oesophageal junction making endoscopic retrieval impossible, and those impacted in the distal duodenum or beyond require operative management with enterolithotomy.
At surgery, the site of the obstruction stone should be identified and an enterotomy performed in healthy bowel proximal to the site of the obstruction. The site of the obstruction stone itself may be quite bruised, oedematous or ulcerated. The duodenum or small bowel should be examined back to the region of the cholecysto-duodenal fistula to ensure there are no further stones in transit or in the gallbladder. If present, these should be milked distally and removed through the enterotomy. The enterotomy is then closed in two layers to prevent leak. The decision of whether or not to perform cholecystectomy and cholecysto-duodenal fistula closure is controversial.
The surgical literature suggests that neither should be attempted during the initial procedure to relieve obstruction in sick elderly patients since the majority of patients require no further treatment of biliary tract disease and the fistula usually closes spontaneously.
In fitter and younger patients or those with persistent biliary tract symptoms, a cholecystectomy is necessary [16]. These pathological “non-surgical” fistulae are potentially harmful as they tend to open and close leading to recurrent cholecystitis and cholangitis when drainage is inadequate. If at time of cholecystectomy a fistula is still present, it should be excised and the duodenum closed in two layers.
Other authors have described various techniques used to retrieve the gallstone from its difficult position in the duodenum. Singh et al. [5] discussed a case where a gallstone was retrieved piecemeal from the duodenal bulb after crushing it with forceps introduced via a pyloroplasty incision. In cases where surgical retrieval of the stone is not possible, gastro-jejunostomy to bypass the site of obstruction may be performed [7].
Previous authors have suggested that endoscopic management should always be attempted prior to surgical retrieval despite acknowledging that these endoscopic attempts are rarely successful [4]. We suggest a tailored approach for Bouveret’s syndrome management as per the above flow chart based on stone size, location of obstruction and patient fitness for surgery. With the availability of the appropriate skills, minimal access surgery represents a further management option.
Acknowledgments
We thank John Evans for assistance in preparing the photos.
References
- Koulaouzidis A, Moschos J. Bouveret’s syndrome. Narrative review. Ann Hepatol. 2007;6(2):89-91.
- Doycheva I, Limaye A, Suman A, Forsmark CE, Sultan S. Bouveret’s syndrome: case report and review of the literature. Gastroenterol Res Pract. 2009; 2009: 914951. 9.
- Lowe AS, Stephenson S, Kay CL, May J. Duodenal obstruction by gallstones (Bouveret’s syndrome): a review of the literature. Endoscopy. 2005;37(1):82-87.
- Cappell MS, Davis M. Characterization of Bouveret’s syndrome: a comprehensive review of 128 cases. Am J Gastroenterol. 2006;101(9):2139-2146.
- Singh AK, Shirkhoda A, Lal N, Sagar P. Bouveret’s syndrome: appearance on CT and upper gastrointestinal radiography before and after stone obturation. Am J Roentgenol. 2003;181(3):828-830.
- Wagholikar GD, Ibrarullah M. Bouveret’s syndrome--an unusual cause of spontaneous resolution of gastric outlet obstruction. Indian J Gastroenterol. 2004;23(3):109-110.
- Joshi D, Vosough A, Raymond TM, Fox C, Dhiman A. Bouveret’s syndrome as an unusual cause of gastric outlet obstruction: A Case Report. J Med Case Rep. 2007;1:73.
- Rigler LG, Borman CN, Noble JF. Gallstone Obstruction. J Am Med Assoc. 1941;117(21):1753.
- Moore EW. The Role of Calcium in the Pathogenesis of Gallstones: Ca++ Electrode Studies of Model Bile Salt Solutions and Other Biologic Systems. Hepatology. 1984;4(S2):228S-243S.
- Verma GR, Pandey AK, Bose SM, Prasad R. Study of serum calcium and trace elements in chronic cholelithiasis. ANZ J Surg. 2002;72(8):596-599.
- Been JM, Bills PM, Lewis D. Electron probe microanalysis in the study of gallstones. Gut. 1977;18(10):836-842.
- Halasz NA. Gallstone Obstruction of the Duodenal Bulb (Bouveret’s Syndrome). Am J Dig Dis. 1964;9:857-861.
- Warshaw AL, Bartlett MK. Choice of operation for gallstone intestinal obstruction. Ann Surg. 1966;164(6):1051-1055.
- A Mohamed NB. Gall Stone Ileus: A Rare Complication of Gallstone Disease. Case Report and Literature Review. Internet J Surg. 2008;21(1).
- Alsolaiman MM, Reitz C, Nawras AT, Rodgers JB, Maliakkal BJ. Bouveret’s syndrome complicated by distal gallstone ileus after laser lithotropsy using Holmium: YAG laser. BMC Gastroenterol. 2002;2:15.
- Chou JW, Hsu CH, Liao KF, Lai HC, Cheng KS, Peng CY, et al. Gallstone ileus: report of two cases and review of the literature. World J Gastroenterol. 2007;13(8):1295-1298.