|
|
|
|
|
Preventable coma- Lithium induced !
|
|
|
Vasanthi Natarajan1, HS Asha2, Kishore Kumar Behra2, Nihal Thomas2
1Department of Endocrinology, Diabetes and Metabolism, Pondicherry Institute of Medical Sciences, Puducherry; 2Department of Endocrinology, Diabetes and Metabolism, Christian Medical College, Vellore, India. |
|
|
|
|
|
Corresponding Author:
|
Dr. Vasanthi Natarajan
Email: vasanthikarthi2004@yahoo.co.in
|
|
|
|
|
|
|
|
|
Received:
20-DEC-2014 |
Accepted:
29-JAN-2015 |
Published Online:
20-FEB-2015 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
Lithium is the one of the drugs of choice for manic depressive illness. Lithium practice guidelines should be followed for every patient before initiating them on lithium therapy. Here we report a case of elderly man with manic depressive illness, who was prescribed lithium, lost follow-up and presented with lithium toxicity- hypothyroidism, nephrogenic diabetes insipidus, sinus node dysfunction. He was managed with parenteral levothyroxine under steroid cover, multiple sessions of hemodialysis and improved. This case report emphasizes the importance of lithium practice guidelines and the responsibility of prescriber to prevent such an event. |
|
|
|
|
|
Keywords :
|
Bipolar Disorder, Lithium, Thyroxine, Hypothyroidism, Renal Dialysis, Genetic Diseases, Humans.
|
|
|
|
|
|
|
|
|
|
|
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff7417060000006e03000001000b00 6go6ckt5b5idvals|430 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
Lithium is the drug of choice for bipolar disorder. Lithium toxicity is one of the serious and preventable conditions, provided lithium practice guidelines are strictly followed. As lithium has narrow therapeutic range its needs periodic monitoring of serum lithium level while on therapy. Elderly patients on lithium are known to cause hypothyroidism and may rarely develop myxedema coma. Toxic serum lithium level can affect cardiac, renal, nervous system. Lithium induced multisystem toxicity will be worsened by underlying untreated hypothyroidism. It is a challenging clinical condition to handle multisystem lithium toxicity in a patient with bipolar disorder. We report a case of lithium toxicity in an elderly person who presented with severe hypothyroidism, sinus node dysfunction and nephrogenic diabetes insipidus.
Case Report
74 year old gentleman staying alone in remote village was brought to the emergency department by his son with a history of progressive decline in his daily activities, unsteadiness of gait over a period of 1 year. He had decline in alertness, loss of memory, slowness of speech and bladder incontinence lasting for duration of 2 days. On examination, BP: 140/90 mmHg, pulse rate: 34/min, Temp: 99oF (rectal), dry skin with periorbital puffiness was seen. He was drowsy, disoriented without any obvious focal neurological abnormalities. He had progressive decline in his activities for last one year and recent worsening for last 2 days. As he had bradycardia, the immediate electrocardiogram revealed complete heart block and temporary pacemaker was advised by the cardiologist.
His detailed previous history revealed underlying bipolar disorder for the last 15 years, he was on tablet lithium. He had no regular follow up with his treating physician. Considering his lithium intake and complete heart block, lithium induced hypothyroidism was suspected. An elevated TSH with a low total T4 and free T4 [Table 1] and an altered sensorium in the presence of high serum lithium, confirmed the diagnosis of lithium induced myxedema coma. His thyroid auto antibodies were negative.
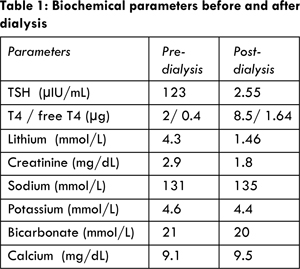
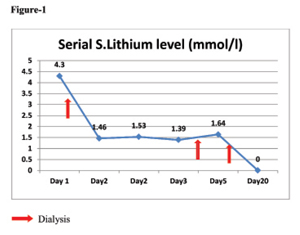
His computerized tomography of the brain was normal; cerebrospinal fluid analysis was unremarkable. His renal function was deranged with an elevated creatinine of 2.9 mg/dL and elevated serum lithium of 4.3 mmol/L (normal range: 0.5-1.5 mmol/L). His serial serum lithium levels are mentioned in figure 1. He underwent three sessions of haemodialysis. Post dialysis his serum lithium level and his renal functions normalized. The details of other biochemical parameters are mentioned in table 1. He was treated with parenteral antibiotics and intravenous levothyroxine 250 mcg once daily for 2 days, oral thyroxine 100 mcg once daily and oral tri-iodothyroinine (cytomel) 25 mcg thrice daily along with parenteral hydrocortisone. He demonstrated remarkable improvement over a period of 72 hours. On sixth day he developed polyuria and hypernatremia (Na: 153 mEq/L), suspected of lithium induced nephrogenic diabetes insipidus which was masked by severe hypothyroidism. He was treated with parenteral fluids and the epithelial sodium channel inhibitor (amiloride hydrocholoride) and improved.
Myxedema coma is most commonly seen in elderly people with age more than 60 years and frequently during winter [1]. Patients with myxedema coma generally have longstanding hypothyroidism, although this may not have been diagnosed previously. Our case as mentioned, had signs of hypothyroidism in the form of altered mentation, dry skin with a marked reduction in his daily physical activities for last one year.
Myxedema coma can be precipitated by number of factors; including infections, non-compliance with thyroid hormone replacement, drugs like lithium, sedatives, analgesics and anaesthetic drugs [1]. Our patient, was on oral lithium for bipolar disorder since last 15 years. He was neither on regular follow up with psychiatrist nor does monitoring his serum lithium level was being done periodically. As a result he developed lithium toxicity with myxedema coma, cardiac conduction defect and renal dysfunction. All patients with myxedema often present with some form of deterioration of their mental status. This decline may be subtle, so high degree of clinical suspicion was needed for detecting myxedema coma, in the presence of long duration of lithium therapy for BPD.
Myxedema coma is an endocrine emergency which needs prompt recognition and appropriate treatment. Because, mortality could be as high as 30 to 60% if treatment is delayed [2]. Patients with suspected myxedema coma should be admitted to intensive care unit for cardiovascular, pulmonary support and treated with combined oral and parenteral thyroxin supplementation. Parenteral steroids should be administered until the coexisting adrenal insufficiency is ruled out.
Lithium is the drug of choice for bipolar disorder since 1949. Lithium causing hypothyroidism is more common than hyperthyroidism [2]. Lithium inhibits the colloid formation in the apical pole of the thyrocyte, inhibits release of thyroid hormone as well as thyroglobulin-iodination; causing hypothyroidism, which could be either overt or subclinical, with or without the presence of goitre. The development of goitre is more severe in iodine deficient state with prolonged lithium intake.
Hypothyroidism is often precipitated by presence of thyroid antibodies. The occurrence of newer thyroid antibodies is more in a state of long term lithium intake because it augments the activity of B lymphocytes and reducing the ratio of circulating suppressor to cytotoxic T cells. The presence of thyroid antibody in lithium induced hypothyroidism requires supplementation of thyroxine [3,4]. Other risk factors for lithium induced hypothyroidism are older age, longer duration of drug intake, female sex, and co-existing iodine deficiency [5]. Annick Vincent et al. reported that the occurrence of hypothyroidism is more in the initial 2 years of lithium intake, about 38%, 55% and 74% of thyroid dysfunction appears within 6, 12, 24 months of lithium respectively. Early monitoring of thyroid function test is important in patients on long term lithium therapy [6]. Parenteral levothyroxine supplementation under steroid cover should be considered in severe lithium induced hypothyroidism. Hypothyroidism due to lithium involve low T3, in contrast to low T4 in lithium free state [7].
Lithium induced neurologic toxicity is graded as mild: fine tremor, weakness, lethargy; moderate: muscle fasciculation, ataxia, tremor, dysarthria, inco-ordination, confusional state, impaired consciousness and severe: with progression to coma, seizure, muscle flaccidity, cerebellar syndrome, irreversible brain damage and death [8]. Mild and moderate forms of toxicity are reversible after stopping the drug. Severe toxicity is fatal and presents with neurological sequelae. The severe form of neurological manifestation is the Syndrome of Irreversible Lithium Effectuated Neuro toxicity (SILENT) [9]. Our patient had moderate form of lithium induced neurotoxicity which improved with treatment.
Sinus node dysfunction could be related to combined effect of lithium toxicity and severe hypothyroidism. Transient sinus nodal dysfunction has been reported with lithium toxicity [10]. Lithium induced cardiac manifestations are transient and reversible after stopping the drug [11]. Cardiac rhythm disturbances are flattening of T waves, QT prolongation, brady, tachyarrhythmia and sinus node dysfunction [12,13]. Primary hypothyroidism by itself can potentiate lithium induced sinus node dysfunction.
Lithium induced renal dysfunction is initially functional and disappear after stopping the drug and improve with amiloride. In long term, it may cause structural and irreversible parenchymal renal damage manifesting as nephrogenic diabetes insipitus, chronic interstitial nephritis and progressive renal failure [14]. Our patient developed renal failure with toxic serum lithium level, which improved after dialysis. Renal failure in our case is multifactorial due to dehydration, hypothyroidism per se as a known factor causing decreased renal glomerular filtration rate and toxic serum lithium level is known to cause renal tubulointerstitial damage leading to irreversible reduction of tubular function [15]. On sixth day of his ICU stay he developed polyuria and hypernatremia. This is due to increased glomerular filtration rate following thyroxine supplementation which causes more free water clearance. This manifested on 6th day, because initiation of thyroxin supplementation has unmasked the underlying nephrogenic diabetes insipidus. Lithium induced nephrogenic DI develops in 20% of the patient on long term drug intake, due to resistance of collecting duct to anti-diuretic hormone [14]. Dehydration, hyponatremia as in our patient will increase the chance of lithium induced renal toxicity.
Conclusion
Thyroid and renal function test including thyroid auto antibodies should be assessed in all patients before lithium is prescribed. Periodic monitoring of serum lithium level should be done. Patient education regarding the side effects, thyroid, renal and cardiac monitoring should be addressed in every visit. In our patient, monitoring of thyroid function test, thyroid auto antibodies, assessment of goiter and renal function could have prevented lithium toxicity.
References
- Cristen R. Myxedema Coma: Diagnosis and Treatment. Am Fam Physician. 2000; 62:2485-2490.
- John H. Lithium and thyroid. Best Practice & Research Clinical Endocrinology & Metabolism. 2009; 23:723-733.
- Bocchetta A, Cocco F, Velluzzi F, Del-Zompo M, Mariotti S, Loviselli A. Fifteen-year follow-up of thyroid function in lithium patients. J Endocrinol Invest. 2007;30:363-366.
- Kibirige D, Luzinda K, Ssekitoleko R. Spectrum of lithium induced thyroid abnormalities: current perspective. Thyroid Res. 2013;6:3.
- Johnston AM, Eagles JM. Lithium-associated clinical hypothyroidism. Prevalence and risk factors. The British Journal of Psychiatry. 1999;175:336-339.
- Vincent A, Barush P, Vincent P. Early Onset of Lithium-Associated Hypothyroidism, J Psychiatry Neurosci. 1993;18:74-77.
- Zhang ZJ, Qiang Li, Kang WH, Tan QR, Gao CG, Zhang FG, et al. Differences in hypothyroidism between lithium-free and treated patients with bipolar disorders. Life Sci. 2006; 78(7):771-776.
- Newman PK, Saunders M. Lithium neuro toxicity, Postgraduate Medical Journal. 1979;55:701-703.
- Munshi KR, Thampy A. The syndrome of irreversible lithium-effectuated neurotoxicity. Clin Neuropharmacol. 2005;28:38.
- Rosenqvist M, Bergfeldt L, Aili H, Mathe A. Sinus node dysfunction during long-term lithium Treatment. Br Heart J. 1993;70:371-375.
- Fatih C, Ahmet K, Serkan B, Enver S. Lithium intoxication related multiple temporary ECG changes: Cases J. 2008;1:156.
- Weintraub M, Hes JP, Rotmensch HH, Soferman G, Liron M. Extreme sinus bradycardia associated with lithium therapy. Isr J Med Sci. 1983;19:353-355.
- Menegueti MG, Basile-Filho A, Martins-Filho OA, Auxiliadora-Martins M. Severe arrhythmia after lithium intoxication in a patient with bipolar disorder admitted to the intensive care unit. Indian J Crit Care Med. 2012;16.
- Bendz H, Aurell M, Balldin J, MathéA A, Sjödin I. Kidney damage in long-term lithium patients: a cross-sectional study of patients with 15 years or more on lithium. Nephrol Dial Transplant. 1994;9:1250.
- Grünfeld JP, Rossier BC. Lithium nephro toxicity revisited. Nat Rev Nephrol. 2009;5:270.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
Natarajan V, Asha HS, Behra KK, Thomas NPreventable coma- Lithium induced !.JCR 2015;5:79-83 |
|
Natarajan V, Asha HS, Behra KK, Thomas NPreventable coma- Lithium induced !.JCR [serial online] 2015[cited 2026 Jan 14];5:79-83. Available from: http://www.casereports.in/articles/5/1/Preventable-coma-Lithium-induced.html |

|
|
|
|
|