|
|
|
|
|
Role of Infliximab in Pediatric Fistulizing Crohn’s Disease
|
|
|
Virtut Velmishi1, Emarjola Brahimllari1, Besa Hidri2, Luciano Mitro1, Guriel Nasto1, Gentiana Cekodhima3, Genti Xhelili4, Paskal Cullufi1
Department of Pediatric Gastroenterology1, Radiology2, Histopathology3 and Pediatric Rheumatology4; University Hospital Center “Mother Teresa” Tirana, Albania. |
|
|
|
|
|
Corresponding Author:
|
Dr. Virtut Velmishi
Email: tutimodh@yahoo.com
|
|
|
|
|
|
|
|
|
Received:
21-FEB-2015 |
Accepted:
21-MAY-2015 |
Published Online:
20-JUN-2015 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
Background: Crohn’s disease, a chronic inflammatory bowel disease (IBD) that was once considered rare in the pediatric population, is currently recognized as one of the most important chronic diseases that affects children and adolescents. Extra-intestinal manifestations rarely can precede IBD leading to a late diagnosis. Case Report: This is a case report of a 13 year old boy admitted for draining abdominal fistulae. The patient refers a six year history of musculoskeletal manifestations with low back pain, recurrent fever and limping. Six months ago he underwent surgery for pelvic abscesses. After surgery he was referred to our service for draining an abdominal fistula. We performed a colonoscopy which shows images and histology compatible with Crohn’s disease. We decided to treat the patient with infliximab, 5 mg per kilogram of body weight administered intravenously at weeks 0, 2, and 6. After the second dose of infliximab we noticed the complete closure of the fistula. Conclusion: Infliximab is a good treatment alternative in patients with Crohn’s disease preceded by musculoskeletal manifestations and complicated by abdominal fistula. |
|
|
|
|
|
Keywords :
|
Inflammatory Bowel Disease, Crohn disease, Infliximab, Fistula, Colonoscopy.
|
|
|
|
|
|
|
|
|
|
|
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff042107000000eb03000001000100 6go6ckt5b5idvals|477 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
Joint involvement is the most common extra-intestinal manifestation in children with inflammatory bowel disease (IBD) and may involve 16%-33% of patients at diagnosis or during follow-up [ 1]. In a large cohort of pediatric IBD patients 6% had at least one extra-intestinal manifestations before diagnosis of IBD [ 2]. Crohn’s disease is characterized by chronic transmural inflammation of the bowel and is associated with serious complications, such as bowel strictures, abscesses, fistula formation, and perforation. The primary goals of the clinician in the treatment of fistulizing CD include defining the anatomy of the fistula, draining any associated infectious material, attempting to eradicate the fistulous tract through medical or surgical therapies, and preventing recurrence of fistulas. Medical therapies include aminosalicylates, corticosteroids, immunosuppressants, and biologic agents [ 3]. As a biologic agent, infliximab, a monoclonal antibody to tumor necrosis factor (TNF), is confirmed for its effectiveness in extra-intestinal manifestations of CD [ 4]. IFX is also indicated for refractory luminal and fistulizing Crohn’s disease that does not respond to other medical therapies or surgery [ 5, 6].
Case Report
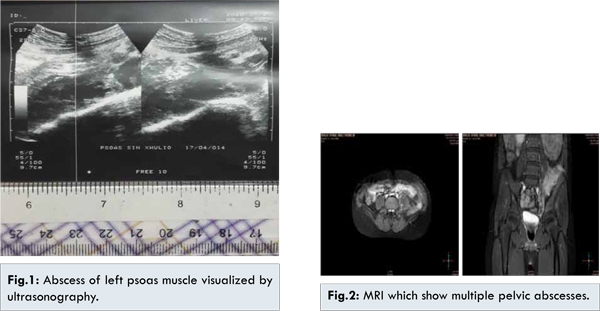
A 13-year-old boy was admitted at service of Pediatric Gastroenterology for draining abdominal fistulae. The history of the disease started at the age of 5 years with low back pain and limping, which improved after one month of conservative treatment. A year later the child was hospitalized with fever and pain in the left thigh. Suspecting osteomyelitis he was treated for more than 10 days with antibiotics. The child presented with recurrent episodes of fever and arthropathy, at least three episodes during the year. A year ago he was consulted by our rheumatologist because of his sacro-iliitis diagnosed on MRI. At the rheumatologic department he tested negative for HLA B27 and rheumatoid factor. Subsequently, he was treated with a short course of cortisone but without any improvement. He had been diagnosed 6 months before coming to our department with pelvic abscesses [Fig.1,2]. He was referred to surgery for abscess removal in the context of osteomyelitis. After intervention, surgeons set a catheter to drain in left lower quadrant of abdomen. After the removal of catheter this percutaneous fistula has leaked continuously. Magnetic resonance imaging of pelvis showed multiple abscesses involving ilio-psoas muscle draining with a fistulous tract in cutis, in inguinal sinister region. Abscesses penetrated into left iliac crest associated with inflammation of gluteus minimus muscle.
At physical examination, he looked pale but in good humor. He was chronically malnourished with weight of 39 kg (<2 SD) and height of 152 cm (<1.5 SD). Cardiac auscultation showed no alterations, lung auscultation was also uneventful. He presented an abdominal tenderness in the left lower quadrant where a percutaneous fistula was visualized [Fig.3].
Laboratory tests showed elevation of inflammatory markers. We found PCR= 38mg/L and a high level of calprotectine. Stool culture and parasitological examination were both negative. The rest of analyzes was normal. However, upper and lower digestive endoscopy showed images compatible with Crohn disease [Fig.4]. Histopathological images from stomach, terminal ileum and colon showed topics of Crohn disease [Fig.5]. First image with biopsy from gastric mucosa was suggestive of focally enhanced gastritis showing active and chronic inflammation with associated granulomas. Second image with biopsy from colon mucosa, revealed that each of the fragments has a different degrees of chronic inflammation.
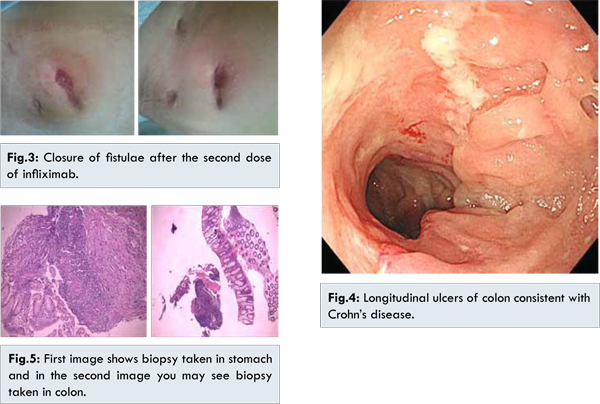
The approach to the patient was discussed in a multidisciplinary meeting and it was decided to start biological therapy. Screening tests were performed before starting infliximab. We decided to start the treatment with infliximab (induction with 5 mg/kg at weeks 0, 2 , 6 and maintenance every 8 weeks). Surprisingly after the second dose of infliximab, complete closure of fistulae was observed. PCR was normalized and the boy has gained weight within a month. Actually we are in treatment with infliximab 5 mg/kg body weight every 8 weeks.
Discussion
Extra-intestinal manifestations in pediatric patients with inflammatory bowel disease (IBD) are very common and are often underestimated, despite provoking a significant impairment in quality of life of patients. Patients with IBD may present with extra-intestinal manifestations (EIMs) of disease before or after diagnosis of IBD. In a cohort study from a large multicenter pediatric IBD registry, EIMs were reported in 6% before diagnosis of IBD, accounting for 25% of the total first EIMs reported by the end of the study follow-up period. EIMs before diagnosis of IBD were found more frequently in children who were older than 5 years at diagnosis.
Joint involvement is the most common extraintestinal manifestation in children with inflammatory bowel disease (IBD). Evidence indicates that a dysregulation of mucosal immunity in the gut of IBD causes an overproduction of inflammatory cytokines into the bowel, thus leading to an uncontrolled intestinal inflammation with joint involvement. Seronegative sacroiliitis and spondyloarthropathy (SpA) are the most frequent forms of arthropathy in children with IBD. In pediatric patients, a correct therapeutic approach relies on the use of nonsteroidal antiinflammatory drugs, local steroid injections, physiotherapy and anti-tumor necrosis factor therapy (infliximab). Early diagnosis of these manifestations reduces the risk of progression and complications, and as well as increasing the efficacy of the therapy. In patients with IBD, the diagnosis of arthritis is essentially clinical and radiological, since magnetic resonance imaging (MRI) has become commonly used in clinical practice, it is possible to recognize early forms of articular manifestations [ 7].
Stawarsky et al. [ 8] carried out an epidemiological study on pediatric IBD patients that confirmed IBD-associated arthropathy in 7%-25% of patients. Subclinical intestinal inflammation in patients with SpA is frequent in pediatric populations, and a long-term follow-up may be needed to determine if indeterminate colitis and intestinal nodular lymphatic hyperplasia can be considered as early forms of IBD. Moreover, we can use certain leukocyte proteins, such as lactoferrin and calprotectin, as markers of the presence of leukocytes in stools, to assess intestinal inflammation. Other non-invasive methods of screening patients presenting arthropathies where intestinal involvement is suspected, include abdominal ultrasound to visualize bowel wall thickness and capsule endoscopy of the small intestine to detect intestinal inflammation before performing endoscopic evaluation [ 10]. HLA-B27 confers an additional risk for inflammatory low back pain in patients with IBD [ 11]. An association between genetic background and human leukocyte antigen-B27 status is less common in pediatric than adult populations. This fact showed why our patient resulted negative for this antigen although he has an extraintestinal manifestation of Crohn disease such as sacroiliitis. But the frequency of HLA B27 in the IBD population is generally not higher compared with the general population. IFX has been effective in inducing and maintaining endoscopic and clinical remission in pediatric CD [12]. Brandt et al. [ 13] reported beneficial effects of IFX on axial and peripheral symptoms in patients with CD and Kaufman et al. confirmed the efficacy of IFX in EIMs of CD. Ellman et al. [ 14] described four patients with CD arthritis where IFX has induced clinical improvement with reduced need for corticosteroids. Generini et al. [ 15] have proposed a therapeutic flowchart in SpA associated with CD, with the use of IFX at a dose of 5 mg/kg. A maintenance schedule provided infusions every 5-8 weeks, and results showed clinical remission in both intestinal and articular diseases for 12-18 mo. IFX appears to be the drug of choice for treating both pathologies. Braun et al. [ 16], in a multicenter randomized trial, demonstrated the persistent clinical efficacy and safety of anti-TNF therapy with IFX (5 mg/kg) in patients with AS over 5 years of almost continuous treatment, with low rates of drug-related adverse events.
Fistulas are a frequent and serious complication of Crohn’s disease [ 17]. Fistulizing Crohn’s disease is a heterogeneous disease, ranging from simple perianal fistulas to complex enterovaginal and enterocolic fistulas. The effect of this drug in fistulizing Crohn’s disease has also been evaluated [ 18]. In a placebo-controlled trial to evaluate the healing of fistulas in Crohn’s disease [ACCENT II (A Crohn’s disease Clinical trial Evaluating infliximab in a New long-term Treatment regimen)] [ 19], infliximab was shown to be highly effective. There was a high response rate, with 68% of patients receiving infliximab 5 mg/kg at weeks 0, 2 and 6 showing a reduction of the fistula by more than 50%, and 55% of patients presenting with the closure of all fistulas. All of the patients included in this study had external fistulas, almost all perianal.
Our patient was treated with infliximab for the confirmed effectiveness of this treatment in randomized studies in patients with extra-intestinal manifestations of CD and to avoid a second surgery in this very young patient.
Conclusion
IBD disease in children may be preceded by extraintestinal manifestations, therefore is very important to draw the attention of pediatricians to suspect IBD in cases of children with a long history of articular manifestations that do not respond to standard therapy, moreover when they see complications such as abscesses and fistula formation. Infliximab is a good treatment alternative in patients with Crohn’s disease preceded by musculoskeletal manifestations and complicated by abdominal draining fistula because it gives them chance for long remission and improvement of quality of life.
References
- Cardile S, Romano C. Current issues in pediatric inflammatory bowel disease-associated arthropathies. World J Gastroenterol. 2014;20(1):45-52.
- Jose FA, Garnett EA, Vittinghoff E, Ferry GD, Winter HS, Baldassano RN, et al. Development of extraintestinal manifestations in pediatric patients with inflammatory bowel disease. Inflamm Bowel Dis. 2009;15(1):63-68.
- Hanauer SB, Sandborn W. Practice Parameters Committee of the American College of Gastroenterology. Management of Crohn’s disease in adults. Am J Gastroenterol. 2001;96:635-643.
- Kaufman I, Caspi D, Yeshurun D, Dotan I, Yaron M, Elkayam O. The effect of infliximab on extraintestinal manifestations of Crohn’s disease. Rheumatol Int. 2005;25:406-410.
- Present DH, Rutgeerts P, Targan S, Hanauer SB, Mayer L, van Hogezand RA, et al. Infliximab for the treatment of fistulas in patients with Crohn’s disease. N Engl J Med. 1999;340:1398-1405.
- Rutgeerts P, Van Assche G, Vermeire S. Optimizing anti-TNF treatment in inflammatory bowel disease. Gastroenterology. 2004;126:1593-1610.
- De Vos M, Van Praet L, Elewaut D. Osteoarticular manifestations: specific treatments and/or treating intestinal disease? Dig Dis. 2013;31:239-243.
- Stawarski A, Iwanczak B, Krzesiek E, Iwanczak F. Intestinal complications and extraintestinal manifestations in children with inflammatory bowel disease. Pol Merkur Lekarski. 2006;20:22-25.
- Conti F, Borrelli O, Anania C, Marocchi E, Romeo EF, Paganelli M, et al. Chronic intestinal inflammation and seronegative spondyloarthropathy in children. Dig Liver Dis. 2005;37:761-767.
- Taddio A, Simonini G, Lionetti P, Lepore L, Martelossi S, Ventura A, Cimaz R. Usefulness of wireless capsule endoscopy for detecting inflammatory bowel disease in children presenting with arthropathy. Eur J Pediatr. 2011;170:1343-1347.
- de Vlam K, Mielants H, Cuvelier C, De Keyser F, Veys EM, De Vos M. Spondyloarthropathy is underestimated in inflammatory bowel disease: prevalence and HLA association. J Rheumatol. 2000;27:2860-2865.
- Wynands J, Belbouab R, Candon S, Talbotec C, Mougenot JF, Chatenoud L, et al. 12-month follow-up after successful infliximab therapy in pediatric Crohn disease. J Pediatr Gastroenterol Nutr. 2008;46:293-298.
- Brandt J, Haibel H, Cornely D, Golder W, Gonzalez J, Reddig J, et al. Successful treatment of active ankylosing spondylitis with the anti-tumor necrosis factor alpha monoclonal antibody infliximab. Arthritis Rheum. 2000;43:1346-1352.
- Ellman MH, Hanauer S, Sitrin M, Cohen R. Crohn’s disease arthritis treated with infliximab: an open trial in four patients. J Clin Rheumatol. 2001;7:67-71.
- Generini S, Giacomelli R, Fedi R, Fulminis A, Pignone A, Frieri G, et al. Infliximab in spondyloarthropathy associated with Crohn’s disease: an open study on the efficacy of inducing and maintaining remission of musculoskeletal and gut manifestations. Ann Rheum Dis. 2004;63:1664-1669.
- Braun J, Baraliakos X, Listing J, Fritz C, Alten R, Burmester G, et al. Persistent clinical efficacy and safety of antitumour necrosis factor alpha therapy with infliximab in patients with ankylosing spondylitis over 5 years: evidence for different types of response. Ann Rheum Dis. 2008;67:340-345.
- Schwartz D, Loftus E, Tremaine W, Panaccione R, Harmsen WS, Zinsmeister AR, et al. The natural history of fistulizing Crohn’s disease in Olmsted County, Minnesota. Gastroenterology. 2002;122:875-880.
- Chambrun G, Peyrin-Biroulet L, Le´mann M, Colombel JF. Clinical implications of mucosal healing for the management of IBD. Nat Rev Gastroenterol Hepatol. 2010;7:15-29.
- Sands B, Anderson F, Bernstein C, Chey W, Feagan B, Fedorak R, et al. Infliximab maintenance therapy for fistulizing Crohn’s disease. N Engl J Med. 2004; 350: 876-885.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
Velmishi V, Brahimllari E, Hidri B, Mitro L, Nasto G, Cekodhima G, Xhelili G, Cullufi PRole of Infliximab in Pediatric Fistulizing Crohn’s Disease.JCR 2015;5:263-268 |
|
Velmishi V, Brahimllari E, Hidri B, Mitro L, Nasto G, Cekodhima G, Xhelili G, Cullufi PRole of Infliximab in Pediatric Fistulizing Crohn’s Disease.JCR [serial online] 2015[cited 2025 Dec 31];5:263-268. Available from: http://www.casereports.in/articles/5/1/Role-of-Infliximab-in-Pediatric-Fistulizing-Crohns-Disease.html |

|
|
|
|
|